
Glioblastoma & Hyperbaric Oxygen Therapy
*Corresponding Author(s):
Malcolm R HooperClinical Director Oxymed, Australia
Tel:+61 3 9826 9898,
Email:info@oxymed.com.au
IMAGE ARTICLE
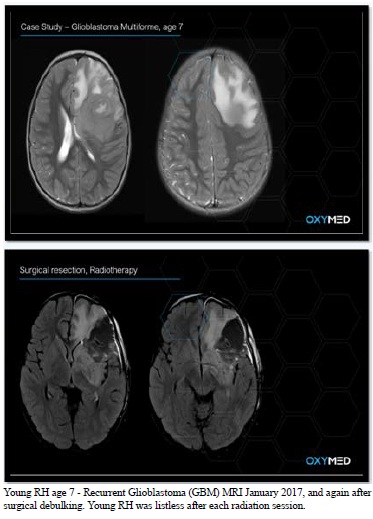
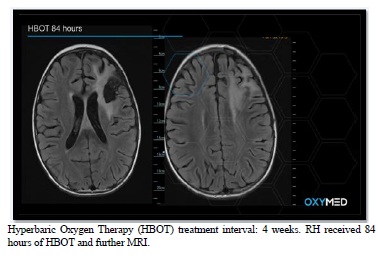
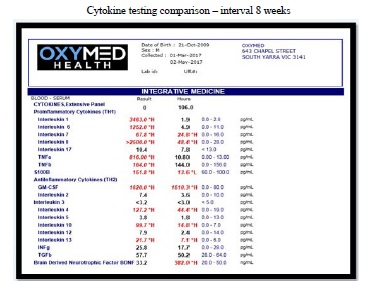
RH was treated using Hyperbaric Oxygenation Therapy (HBOT) at 1.8ATA and 100% O2 with regular air breaks. RH continued with a strict ketogenic diet [1,2] and supplements focused on cytokine modulation. RH did not experience any side effects or seizures during or after HBOT sessions. RH’s improvement whilst undertaking HBOT was extraordinary. He returned to school and mostly to a normal life.
Oxygen that is given at a pressure that is higher than the pressure of the atmosphere at sea level. In medicine, breathing hyperbaric oxygen increases the amount of oxygen in the body. It is used in treating certain kinds of wounds, injuries, and infections. It is also used to treat carbon monoxide poisoning and other conditions in which the tissues are not getting enough oxygen [3]. It is being studied in the treatment of some types of cancer. Hyperbaric oxygen may increase the amount of oxygen in cancer cells, which may make them easier to kill with radiation therapy and chemotherapy. It is a type of radio sensitizing agent and a type of chemosensitizing agent [3,4]. HBOT assists immune responses to chemotherapy reducing immunosuppression and neutropenia [4].
Glioblastoma multiforme (GBM) is the most common type of malignant intracranial tumor in adults and has a poor prognosis, with a median survival of about 12 months. It is rare in children with the prognosis unfavourable [5]. Despite advances in surgery and adjuvant treatment, the average survival is about 1 year, which has not been improved significantly during the last three decades [3,5].
Tumor hypoxia, high mitotic rate, and rapid tumor spread account for its poor prognosis [6-8]. Hypoxia alters cancer cell metabolism and contributes to therapy resistance [9]. Hypoxia stimulates a complex cell signaling network in cancer cells, including the HIF, PI3K, MAPK, and NF?B pathways. Tumor hypoxia and HIF cell signaling are involved in tumor blood vessel formation, metastasis, and development of the resistance to therapy [8,9].
Hyperbaric Oxygen Therapy may improve the sensitivity of radio-chemotherapy by increasing oxygen tension within the hypoxic regions of the neoplastic tissue [10].
Limited clinical trials and suggest that radiotherapy immediately after HBOT enhances the effects of radiotherapy in some cases [6,11]. HBOT also is able to strengthen the anti-tumor effect of chemotherapy when applied together [12]. Overall, HBOT is well tolerated in the GBM patients and does not significantly increase toxicity [6]. HBOT applied by itself as curative strategy against GBM and other cancer forms is controversial [13,14]. In addition to HBOT favorably managing the therapeutic resistance of GBM, research is now focussed on the multimodal or cocktail approaches to treatment, as well as molecular strategies targeting GBM stem cells [12]. The reoxygenation brings additional benefit of making glioblastoma multiforme cells even more responsive to the killing effect of a cytotoxin [12].
DISCUSSION
HBOT has been described as the 'integrative bridge' between orthodox medicine and complimentary approaches. Oxygen is essential to drug delivery [15].
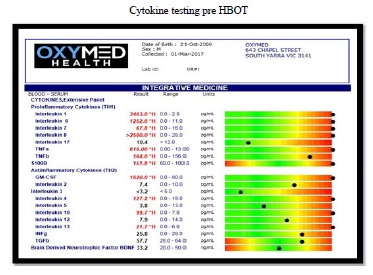
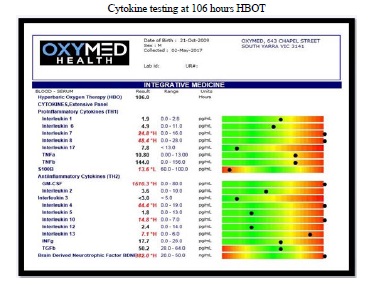
HBOT reduces inflammatory cytokines including IL-1β, IL-6, IL-8, TNF-α, S100B through several transcription factors regulating inflammation, including hypoxia inducible factor 1 (HIF-1), Nrf2 and NFkB [10,12-14,16].
HBOT up regulates the patient’s own target specific Stem Cells {an 8-fold (800%) increase in circulating CD34+} [17,18].
HBOT enhances Mitochondrial respiration and function [12,19].
ACKNOWLEDGEMENT
I would like to thank the parents of RH for permission to use the clinical findings to support this presentation.
REFERENCES
- Poff AM, Ward N, Seyfried TN, Arnold P, Agostino DP (2015) Non-Toxic Metabolic Management of Metastatic Cancer in VM Mice: Novel Combination of Ketogenic Diet, Ketone Supplementation, and Hyperbaric Oxygen Therapy. Plos One 10: e0127407.
- Seyfried TN, George Yu, Maroon JC, D'Agostino DP (2017) Press-Pulse: A novel therapeutic strategy for metabolic management of cancer. Nutr Metab (Lond) 14: 19.
- Jain KK (2004) Chapter 35 The role of HBO in Enhancing Chemosensitivity: Textbook of Hyperbaric Medicine, 4th Edition, ed. Kewel K. Jain. Springer, Cham, Switzerland, 2004.
- https://www.cancer.gov/publications/dictionaries
- Ansari M, Nasrolahi H, Kani AA, Mohammadianpanah M, Ahmadloo N, et al. (2012) Pediatric glioblastoma multiforme: A single-institution experience. Indian J Med Paediatr Oncol 33: 155-160.
- Graham K, Unger E (2018) Overcoming tumor hypoxia as a barrier to radiotherapy, chemotherapy and immunotherapy in cancer treatment. Int J Nanomedicine 13: 6049-6058.
- Augur ZM, Doyle CM, Li M, Mukharjee P, Seyfried TY (2018) Nontoxic Targeting of Energy Metabolism in Preclinical VM-M3 Experimental Glioblastoma. Front Nutr 5: 91.
- Daruwalla J, Christophi C (2006) Hyperbaric oxygen therapy for malignancy. World J Surg 30: 2112-2131.
- Muz B, Puente P, Azab F, Azab AK (2015) The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Dove Press Journal. Hypoxia 3: 83-92.
- Huang L, Boling W, Zhang JH (2018) Hyperbaric oxygen therapy as adjunctive strategy in treatment of glioblastoma multiforme. Med Gas Res 8: 24-28.
- Ogawa K, Kohshi K, Ishiuchi S, Matsushita M, Yoshimi N, et al. (2013) Old but new methods in radiation oncology: Hyperbaric oxygen therapy. Int J Clin Oncol 18: 364-370.
- Liu TF, Cai J, Gibo DM, Debinski W (2009) Hyperbaric Oxygenation of Hypoxic Glioblastoma Multiforme Cells Potentiates the Killing Effect of an Interleukin-13-Based Cytotoxin. Clin Cancer Research 15: 160-168.
- St?pien K, Ostrowski RP, Matyja E (2016) Hyperbaric oxygen as an adjunctive therapy in treatment of malignancies, including brain tumours. Med Oncol 33: 101.
- Feldmeier F, Carl U, Hartmann K, Sminia P (2003) Hyperbaric Oxygen does it promote growth or recurrence of malignancy? Undersea Hyperb Med 30: 1-18.
- Hooper MR (2018) Hyperbaric Medicine-The Life is in the Blood. 6th International Conference on Brain Disorders and Therapeutics.
- https://www.townsendletter.com/article/oxygen-and-pressure-epigenetics-understanding-hyperbaric-oxygen-therapy-after-355-years-as-the-oldest-gene-therapy-known-to-man/
- Shandley S, Wolf EG, Schubert Kappan CM, Baugh LM, Richards MF, et al. (2017) Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy. Undersea Hyperb Med 44: 257-269.
- Thom SR, Bhopale VM, Velazquez OC, Goldstein LJ, Thom LH, et al. (2005) Stem cell mobilization by hyperbaric oxygen. Am J Physiol Heart Circ Physiol 290: H1378-1386.
- Moen E, Stuhr LEB (2012) Hyperbaric Oxygen Therapy and Cancer--A Review.Target Oncol 7: 233-242.
Citation: Hooper MR (2020) Glioblastoma & Hyperbaric Oxygen Therapy. J Alzheimer’s Neurodegener Dis 6: 044.
Copyright: © 2020 Malcolm R Hooper, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

