Improving Access to HIV and Sexual Reproductive Health Services for Key Populations along Nigeria’s Transport Corridors: The STOP Project
*Corresponding Author(s):
Obinna Ositadimma OleribeExcellence And Friends Management Consult, P.O. Box 200 PSIN Dutse, Dutse Abuja FCT, 901101, Nigeria
Tel:+234 8096083335,
Email:Obinna.oleribe@expertmanagers.org
Abstract
Methods: The Strategic Travelers Outreach Program (STOP) took place between February and August 2016 in Sagamu/Ogere and Obollo-Afor travel corridors. Through community advocacy and outreach, house-to-house, door-to-door and community/office testing, key populations were provided with targeted HIV, SRH and referral services.
Results: Over 50,000 people were contacted with HIV and SRH education/counselling. 19,275 (M: 10,965, 56.9%; F: 8,310, 43.1%) were tested with all receiving their results same day. General positivity rate was 1.3%: female (1.9%). Brothel-based female sex workers had higher positivity rate (3.2%). The study also revealed prostitutes did not use condoms with their husbands or long-term boyfriends and that knowledge of HIV was poor.
Conclusion: The results highlight an urgent need to mobilize educational and healthcare resources to mitigate HIV transmission along these corridors. A socio-anthropological approach is required to alter long-held beliefs and change risk-seeking behavior.
Keywords
INTRODUCTION
Although HIV is most common among key populations (females who sell sex brothel and non-brothel based), Men-who-have-Sex-with-Men (MSM), People who Inject Drugs (PID), military and paramilitary personnel and long distance drivers; their access to reproductive and sexual health is limited [1,2]. Such limitations are also seen among women and men living with HIV as there is little programmatic guidance as to how best ensure access to sexual and reproductive health services [3]. As HIV/AIDS remains a major public health burden around the world, affecting over 36 million people and leading to the death of about 34 million people, there has been an increasing awareness and discussion of the benefits of linkage between Sexual Reproductive Health (SRH) and HIV programs at the policy, systems and service delivery levels [4,5]. Moreover, in 2010, HIV/AIDS was reported as having the 5th largest associated Disability-Adjusted Life Year (DALY) measurement - a measure of overall disease burden, expressed as the number of years lost due to ill-health, disability or early death. HIV had the most prominent DALY association for people of both sexes, aged from 30-44 years in Eastern, Southern and Central Africa, the Caribbean and Thailand [6]. On that background, HIV has remained one of the most important communicable diseases in Nigeria, affecting close to 3.5 million people with about 1,476,741 requiring Anti-Retroviral Drugs (ARV) in 2013 [7].
Despite a seeming decline in HIV prevalence, the burden of HIV disease is disproportionately high among key populations, such as females who sell sex, men-who-have-sex-with-men, people who inject drugs and long distance transport workers where rates have remained relatively high with spikes in incidence across the world [8-10]. In Nigeria, the Integrated Biological and Behavioral Surveillance Survey (IBBBS) study revealed that Men-who-have-Sex-with-Men (MSM) have the highest prevalence of 22.9%, followed by Brothel-Based Females Who Sell Sex (BBFWSS) with 19.4% prevalence, Non-Brothel-Based Females Who Sell Sex, (NBBFWSS) at 8.6% and long distance truck drivers, who had the lowest prevalence of the at-risk populations at 1.6% [11]. Some of the factors which increase the vulnerability of these groups to HIV infection and maintenance of the epidemic at the population level include risky sexual behavior, current sex-work laws and enforcement-based policies, poor perception of HIV risk, poverty, ineffective STI programming, poor integration of HIV/AIDS and sexual and reproductive health services and gender inequality [12,13].
Furthermore, key populations have remain highly stigmatized and are unable to access appropriate health care services or exercise their rights to health due to legal restrictions, discrimination and society mediated violence [14]. For instance, in Nigeria, sex trade is an illegal trade and practitioners are criminalized; and when seen, they are arrested, required to either pay fine for their release (bail) and spend some time in prison/detention [15,16]. In the midst of the current global economic recession, it is important to track the magnitude of the HIV/AIDS epidemic, its drivers and consequences, to allocate efficiently the limited resources and to maintain funding for effective HIV/AIDS interventions and treatments [6]. In Nigeria, a particular focus for disease transmission is the “travel corridor”, which is a resting zone along the long distance high traffic motorways, where travelers stop for rest, refreshment and ad hoc purchases, before continuing to their final destinations. To track the epidemic, the Nigerian National Agency for the Control of AIDS (NACA) conducted a travel corridor assessment and mapping exercise in 2013, which revealed the need for a specific travel corridor project to assess the microculture and HIV disease prevalence in these communities [17]. The goal of this project was to improve the access of key populations to reproductive and sexual health along two travel corridors in Nigeria.
METHODOLOGY
Pre-project activities


Permission to execute the work was sought and obtained from appropriate state, institutional and local government authorities. HIV Rapid Diagnostic Kits, information bulletins and fliers and condoms were sourced from NACA and shipped to Sagamu and Obollo-Afor. Startup meetings were held in Abuja, Sagamu and Obollo-Afor. Information, Education and Communication (IEC) materials were produced and distributed.
Project areas
Site 1:
Site 2: Obollo-Afor: Obollo-Afor is the head quarter of Udenu LGA and is situated at the regional boundary between the South-East and North-Central geopolitical zones of the country [17]. Obollo-Afor has mostly farmers and traders as inhabitants. The traders sell mostly locally made and harvested farm products such as cassava, yams, cocoyam, cashew and palm kernels. The Afor market of Obollo-Afor runs every four days and is highly patronized by people from the northern and southern regions of the country. This makes Obollo-Afor a very busy travel corridor linking northern Nigeria to the south. However, healthcare services are scarce as the only secondary care center is in another community.
Project activities

Qualitative studies
Results
| Male | Female | Total | ||||
| Location | Tested | Positive | Tested | Positive | Tested | Positive |
| Sagamu | 5,594 | 57 (1.0%) | 4013 | 113 (2.8%) | 9,607 | 170 (1.8%) |
| Obollo-Afor | 5,371 | 32 (0.6%) | 4297 | 41 (1.0%) | 9,668 | 73 (0.8%) |
| Total | 10,965 | 89 (0.8%) | 8,310 | 154 (1.9%) | 19,275 | 243 (1.3%) |
| Description | Ogere | Sagamu | Total | Obollo-Afor | ||||
| Tested | Positive | Tested | Positive | Tested | Positive | Tested | Positive | |
| Touts (Agbero) | 6 | 0 (0.0%) | 293 | 2 (0.7%) | 299 | 2 (0.0%) | 300 | 4 (1.3%) |
| Long Distant Drivers | 2195 | 29 (1.3%) | 809 | 18 (2.2%) | 3004 | 47 (1.6%) | 1400 | 10 (0.7%) |
| Commercial Moto Cycle (Okada) Riders | 955 | 0 (0.0%) | 1110 | 2 (0.2%) | 2065 | 2 (0.1%) | 2200 | 10 (0.45%) |
| Hawkers/Market Women &Men | 448 | 22 (4.9%) | 1998 | 31 (1.6%) | 2446 | 53 (2.2%) | 4040 | 27 (0.67%) |
| Females who sell sex | 306 | 24 (7.8%) | 309 | 20 (6.5%) | 615 | 44 (7.2%) | 320 | 6 (1.9%) |
| Military and paramilitary personnel | 23 | 0 (0.0%) | 106 | 0 (0.0%) | 129 | 0 (0.0%) | 54 | 1 (1.8%) |
| Travellers and General Population | 203 | 3 (1.5%) | 845 | 23 (2.2%) | 1048 | 23 (2.2%) | 1354 | 15 (1.11%) |
| Description | Tested | Positive | Positivity Rate |
| Long Distant Drivers | 63 | 2 | 3.2 |
| Commercial Motor Cylce (Okada) Riders | 51 | 2 | 3.9 |
| Hawkers/Market Women | 34 | 3 | 8.8 |
| Military and Paramilitary Personnel | 44 | 1 | 2.3 |
| Female who sell sex | 6 | 2 | 33.3 |
| Total | 220 | 10 | 4.5% |
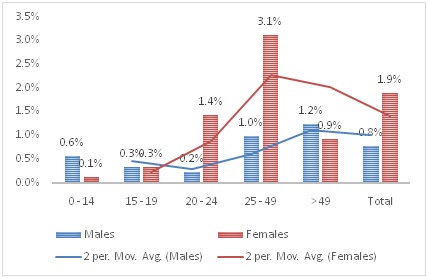
Generally, people aged 25-49 years-old had the highest positivity rate (2.4%). In Ogere alone, those within the age bracket 20-24 years had a higher prevalence rate of 3.9%, as against 3.8% for those 25-49 years (Table 4). A similar finding was made in Obollo-Afor where persons aged 25-29 years had the highest age specific positivity rate (Table 5).
| Ogere | Sagamu | Total | ||||
| Age group | Tested | Positive | Tested | Positive | Tested | Positive |
| 0-14 | 112 | 1 (0.9%) | 688 | 3 (0.4%) | 800 | 4 (0.5%) |
| 15-19 | 194 | 2 (1.0%) | 751 | 4 (0.5%) | 945 | 6 (0.6%) |
| 20-24 | 463 | 18 (3.9%) | 987 | 2 (0.2%) | 1450 | 20 (1.4%) |
| 25-49 | 1430 | 54 (3.8%) | 4024 | 76 (1.9%) | 5454 | 130 (2.4%) |
| > 49 | 113 | 3 (2.7%) | 844 | 8 (0.9%) | 957 | 11 (1.1%) |
| Total | 2312 | 78 (3.4%) | 7295 | 93 (1.3) | 9606 | 171 (1.8%) |
| Males | Females | |||
| Age Group | Tested | Positive (%) | Tested | Positive (%) |
| 0-14 | 715 | 4 (0.6%) | 816 | 1 (0.1%) |
| 15-19 | 1168 | 4 (0.3%) | 1189 | 4 (0.3%) |
| 20-24 | 1804 | 4 (0.2%) | 1463 | 21 (1.4%) |
| 25-49 | 6393 | 63 (1.0%) | 3985 | 124 (3.1%) |
| > 49 | 885 | 11 (1.2%) | 857 | 8 (0.9%) |
| Total | 10965 | 86 (0.8%) | 8310 | 158 (1.9%) |
Interviews of FWSS revealed that they did not use condoms with their husbands or long-term boyfriends. Also, their knowledge of HIV transmission risk was poor as less than 10% had a good understanding of the real meaning of HIV, transmission channels and prevention strategies. Unstandardized interviews of some FWSS revealed that a number of them knew their status (some for over 3 years), were already on antiretroviral medications or had stopped their medications because of lack of access to antiretroviral therapy (as some moved out from their previous locations to seek acceptance in new locations). Also, a number of them were married with grown-up children, had boyfriends with whom they do not use condoms and were unwilling to share their positive HIV status with their partners, clients and boyfriends. Finally, less than 10% of all those surveyed had adequate knowledge of HIV, its origin, channels of transmission and control strategies.
DISCUSSION
The FWSS had the highest prevalence of 7.8% in Ogere, 6.5% in Sagamu and 1.9% in Obollo-Afor while military and paramilitary personnel had the lowest positivity rate in Sagamu/Ogere axis but higher rates in Obollo-Afor. These finding are in line with the recent Nigerian study which showed an overall HIV prevalence among the target groups of 9.5% with the highest prevalence seen among MSM (22.9%), followed by brothel based females who sell sex (19.4%), non-brothel based females who sell sex (8.6%), people who inject drugs (3.4%), police (2.5%), transport workers (1.6%) and armed forces (1.5%) [11]. A field study by EFMC in 2012 showed a similar high prevalence among females who sell sex with some brothel based females who sell sex having positivity rate of over 50% [19].
The different positivity rate among the military and paramilitary groups in both regions may reflect their higher level of mobility in the Nigerian South East, compared to the South-West zone. Also, there was no identifiable pattern for the positively rates seen in the rest of the key populations. This calls for a more detailed controlled study to uncover the sociological factors responsible for the current positive rates seen in the communities. During the project, it was found that FWSS were not disclosing their status, not even to their long-term boyfriends. The non-disclosure of status by FWSS shows the dangers men face when they patronize FWSS. This risk is high as studies have shown prevalence rates of up to 50% among BBFWSS [11,19]. What is more disturbing is the fact that some male customers pay extra money to the FWSS for sex without condoms, a practice that increases the possibility of new or multiple infection(s). The high HIV positivity level seen in travelers along the Obollo-Afor corridor is another issue of concern, as recent studies show a rising prevalence in Anambra (from 8.7% in 2010 to 9.7% in 2014) and Imo (3.0% to 7.5%) States, but a slightly reducing prevalence in the other States in the South East of Nigeria, including Enugu State, which decreased from 5.1% in 2010 to 4.9% in 2014 [20,21]. If the majority of those with HIV were traveling to the region (this was not studied in this work), the region may be at the risk of rising prevalence, if nothing is done.
More males were found to be reactive early in life (2.7%). Prevalence among the various sex groups gradually decreased until 20-24 years and begins to rise again (Table 5 and Figure 4). Among females, the trend was different. Females aged 0-14 years had the lowest HIV rate, but the rate increases in a linear pattern over the age-groups considered up to 25-49 years and then began to decline (Figure 4). This study, therefore, observed that more males were found to be HIV-infected at younger ages, with HIV prevalence decreasing up to 25 years, then increasing after 25 years of age. With females, the HIV prevalence increased gradually increases up to 49 and by 50 years and above, began to decline. An STI screening and HTC conducted among FWSS at other locations in Enugu State in 2016 showed that HIV prevalence was highest among those aged 25-49 [21]. Beyond sexual exposure, the factors behind this trend are not immediately apparent. The reason for this trend will need further exploration and thus will require future expanded qualitative studies. Refusal to disclose HIV status, even to close sexual partners, can negatively affect the overall outcome of any control measure. Working to improve their HIV knowledge will facilitate control efforts.
LIMITATIONS
CONCLUSION
RECOMMENDATIONS
REFERENCES
- WHO (2014) Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. WHO, Geneva, Switzerland.
- Dellar RC, Dlamini S, Karim QA (2015) Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc 18: 19408.
- Gruskin S, Ferguson L, O'Malley J (2007) Ensuring sexual and reproductive health for people living with HIV: an overview of key human rights, policy and health systems issues. Reprod Health Matters 15: 4-26.
- Kennedy CE, Spaulding AB, Brickley DB, Almers L, Mirjahangir J, et al. (2010) Linking sexual and reproductive health and HIV interventions: a systematic review. J Int AIDS Soc 13: 26.
- WHO (2016) Global Health Observatory (GHO) data. HIV/AIDS, WHO, Geneva, Switzerland.
- Ortblad KF, Lozano R, Murray CJ (2013) The burden of HIV: insights from the Global Burden of Disease Study 2010. AIDS 27: 2003-2017.
- National Agency for the Control of AIDS (NACA) (2014) Federal Republic of Nigeria Global AIDS Response Country Progress Report, Abuja, Nigeria.
- Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, et al. (2012) Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 12: 538-549.
- Beyrer C, Abdool Karim Q (2013) The changing epidemiology of HIV in 2013. Curr Opin HIV AIDS 8: 306-310.
- Wolf RC, Cheng AS, Kapesa L, Castor D (2013) Building the evidence base for urgent action: HIV epidemiology and innovative programming for men who have sex with men in sub-Saharan Africa. J Int AIDS Soc 16: 18903.
- Federal Ministry of Health (2015) Integrated Biological and Behavioral Surveillance Survey (IBBSS) 2014. National HIV/AIDS & STIs Control Programme, Abuja FCT Nigeria, Nigeria.
- Shannon K, Strathdee SA, Shoveller J, Rusch M, Kerr T, et al. (2009) Structural and environmental barriers to condom use negotiation with clients among female sex workers: implications for HIV-prevention strategies and policy. Am J Public Health 99: 659-665.
- Kasedde S, Luo C, McClure C, Chandan U (2013) Reducing HIV and AIDS in adolescents: opportunities and challenges. Curr HIV/AIDS Rep 10: 159-168.
- NACA (2013) Minimum Prevention Package Intervention (MPPI): A simple Implementation Guide. NACA, Government of Nigeria, Abuja, Nigeria.
- Harcourt C, Egger S, Donovan B (2005) Sex work and the law. Sex Health 2: 121-128.
- Izugbara OC (2010) ‘Ashawo suppose shine her eyes’: Female sex workers and sex work risks in Nigeria. Health, Risk & Society 7: 141-159.
- NACA (2013) Nigerian Transport Corridor Project: Mapping of selected locations. NACA/MDG Supported Transport Corridor Project.
- Federal Ministry of Health (2013) National HIV and AIDS and Reproductive Health Survey (NARHS Plus II, 2012). Federal Republic of Nigeria, Federal Ministry of Health, Abuja, Nigeria.
- Oleribe OEO, Fasuba M, Osita-Oleribe PI, Udoh PU, Nwachukwu EC (2013) Targeting Most at Risk Populations (MARPS) and HIV Prevalence in North-Central Nigeria. 29th National Scientific and Annual general meeting of Association of Public Health Physicians of Nigeria (APHPN), Ilorin, Kwara, Nigeria. Pg no: 20.
- Federal Ministry of Health (2015) 2014 National HIV Sero-prevalence - Sentinel Survey among Pregnant Women Attending Antenatal Clinics in Nigeria. National AIDS/STI Control Programme, Federal Ministry of Health, Abuja FCT Nigeria, Nigeria.
- NACA (2016) Demand Creation for STI services and management of Sexually Transmitted Infections among High Risk Women and Vulnerable Girls in selected High Burden States: Report of Enugu State Intervention, Nigeria.
- Heckman JJ (2010) Selection bias and self-selection. In: Durlauf SN, Lawrence E. Blume (eds.). Microeconometrics. Palgrave Macmillan, Basingstoke, UK. Pg no: 242-266.
- Nilsen RM, Vollset SE, Gjessing HK, Skjaerven R, Melve KK, et al. (2009) Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr Perinat Epidemiol 23: 597-608.
Citation: Oleribe OO, Iyalla G, Okoro U, Ezechukwu C, Agogo E, et al. (2017) Improving Access to HIV and Sexual Reproductive Health Services for Key Populations along Nigeria’s Transport Corridors: The STOP Project. J AIDS Clin Res Sex Transm Dis 4: 011.
Copyright: © 2017 Obinna Ositadimma Oleribe, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.