
Longitudinal Evaluation of an Acute Nd:YAG Laser-Induced Macular Hole: A Case Report
*Corresponding Author(s):
Mauricio Bayram-SuverzaDepartment Of Ophthalmology, Unidad Medica De Alta Especialidad, Hospital De Especialidades “Bernardo Sepúlveda Gutiérrez”, Centro Medico Nacional Siglo XXI, IMSS, Mexico City, Mexico
Email:mau_203@hotmail.com
Abstract
Macular Holes (MHs) caused by neodymium-doped yttrium aluminum garnet (Nd:YAG) lasers are increasingly reported worldwide, but there is little experience with their management. Furthermore, longitudinal evaluations of their characteristics are scarce. Here, we describe the ophthalmologic findings and follow-up of a patient with an accidental Nd:YAG laser-induced MH. The patient attended with central scotoma of the right eye. The initial Best-Corrected Visual Acuity (BCVA) was 20/400, and fundoscopy revealed a foveal disruption with vitreous hemorrhage. A Swept-Source Optical Coherence Tomography (SS-OCT) scan showed a full-thickness MH. The patient received oral prednisone and follow-up every two weeks. Over time, the patient reported improvement of the scotoma perception. Also, subsequent evaluations showed reabsorption of the vitreous hemorrhage, progressive parafoveal swelling, and complete formation of the MH that stabilized after six weeks (final BCVA 20/80). Our report illustrates the longitudinal characteristics of acute Nd:YAG laser-induced MHs and their short-term response to systemic corticosteroids.
Introduction
Neodymium-doped yttrium aluminum garnet (Nd:YAG) lasers have been increasingly used for different applications in ophthalmology, including photocoagulation of proliferative diabetic retinopathy, iridotomy for glaucoma, disruption of vitreous eye floaters, and correction of posterior capsular cataracts [1-3]. These lasers produce infrared light beams emitted at short pulses of less than one microsecond, with a wavelength of 1064 nm [4,5], larger than other lasers used in ophthalmology such as femtosecond (1053 nm), argon (488 to 515 nm), krypton (530 to 647 nm), or helium lasers ( 632.8 nm) [5].
Of note, lasers could also cause significant lesions to important ocular structures, as is the case of accidental macular holes (MHs) [6]. Although rare, laser-induced MHs have a negative impact on visual acuity that could be irreversible in some cases [7,8]. Specifically, MHs associated with Nd:YAG lasers are originated from a mechanical injury of the retina through the formation of plasma that generates bubble-shaped cavitation and disrupts all retinal layers. Hence, these lesions might be more severe than thermic injuries of argon, krypton, or diode lasers [6-9]. Despite their importance, Nd:YAG laser-induced MHs have been poorly characterized clinically [8-16], and there is little experience available in the literature about their evaluation and management in developing countries.
Here, we describe the ophthalmologic findings, swept-source optical coherence tomography (SS-OCT) evaluation, and longitudinal follow-up of a patient with an accidental traumatic MH associated with Nd:YAG laser.
Case Report/Case Presentation
A 30-year-old man who worked as a technician in laser equipment repair attended our ophthalmologic emergency department due to sudden visual acuity decrease, central scotoma, and myodesopsia of the right eye. The symptoms began five hours before the consultation while the patient was repairing an Nd:YAG laser for cosmetic surgery without wearing protective glasses. The laser parameters at the time of the incident were: 300 mJ pulse energy, 7 seconds pulse duration, 10 Hz frequency, 1064 nm wavelength. Other aspects of his medical history were not relevant.
On admission, the patient was aware and oriented to person, place, and time. General physical examination did not reveal any neurological, cardiological, thoracic, or abdominal abnormality. The best-corrected visual acuity (BCVA) of the right eye was 20/400, and fundoscopic evaluation revealed a disruption in the foveal region and remnants of parafoveal vitreous hemorrhage. An SS-OCT scan (DRI-OCT Triton, Topcon Medical System Inc., USA) showed a full-thickness MH with mild vitreous hemorrhage (Figure 1). Thus, treatment was started with a single dose of IV methylprednisolone 1 mg/kg and follow up every two weeks. During the second evaluation, the patient reported improved visual acuity and reduced subjective perception of scotoma. BCVA was 20/140, and the SS-OCT scan showed similar characteristics of the MH with inflammatory infiltrates (Figure 2A). Hence, steroid treatment was continued with a weekly tapering prednisone regimen starting at 50mg/day.
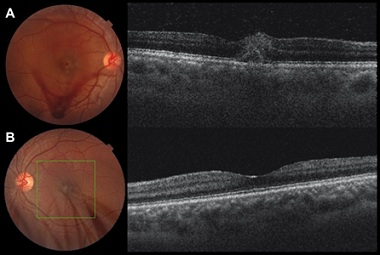 Figure 1: Initial characteristics of an Nd:YAG laser-induced MH. A) Fundoscopic photograph of the affected eye on the day of injury showing loss of continuity of the retina in the foveal region and vitreous hemorrhage along the inferior temporal arch (left panel). The SS-OCT scan revealed a full-thickness central disruption at the fovea (right panel). B) Evaluation of the contralateral eye without injury.
Figure 1: Initial characteristics of an Nd:YAG laser-induced MH. A) Fundoscopic photograph of the affected eye on the day of injury showing loss of continuity of the retina in the foveal region and vitreous hemorrhage along the inferior temporal arch (left panel). The SS-OCT scan revealed a full-thickness central disruption at the fovea (right panel). B) Evaluation of the contralateral eye without injury.
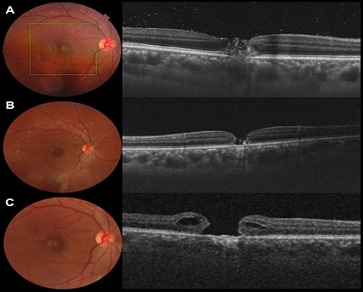 Figure 2: Longitudinal evaluation of an Nd:YAG laser-induced MH. A) Fundoscopy (left panel) and SS-OCT scan (right panel) two weeks following the initial event showing partial reabsorption of the vitreous hemorrhage and a full-thickness MH. B) Four weeks after the exposure, the hemorrhage is completely reabsorbed, the MH is apparent in the fundoscopic evaluation, and the SS-OCT scan shows inflammatory debris and non-apparent involvement of the retinal pigment epithelium. C) After six weeks, the MH shows elevated retinal edges that display cystic characteristics.
Figure 2: Longitudinal evaluation of an Nd:YAG laser-induced MH. A) Fundoscopy (left panel) and SS-OCT scan (right panel) two weeks following the initial event showing partial reabsorption of the vitreous hemorrhage and a full-thickness MH. B) Four weeks after the exposure, the hemorrhage is completely reabsorbed, the MH is apparent in the fundoscopic evaluation, and the SS-OCT scan shows inflammatory debris and non-apparent involvement of the retinal pigment epithelium. C) After six weeks, the MH shows elevated retinal edges that display cystic characteristics.
Four weeks after the incident, BCVA improved to 20/100, but the subjective perception of the scotoma and the MH characteristics in the SS-OCT evaluation remained unchanged (Figure 2B). For this reason, an inverted Internal Limiting Membrane (ILM) flap technique with vitrectomy was proposed, but the patient refused the surgical treatment. The BCVA continued to improve until stabilizing at 20/80 after six weeks of follow-up. Clinical and SS-OCT findings did not improve ever since, and the final measurements of the MH were 192 µm height and 505 µm width at the base (Figure 2C). Currently, the patient is still under periodic surveillance with bimonthly SS-OCT scans.
Discussion/Conclusion
Atypical or secondary MHs are full-thickness disruptions of the retinal layers at the fovea caused by numerous ocular pathologies, including vascular abnormalities, uveitis, degenerative causes, infections, retinal dystrophies, miscellaneous causes, and postprocedural iatrogenic or accidental injuries [7]. Contrary to their primary or idiopathic counterpart, the management of secondary MHs is not well defined, and current therapeutic modalities are advocated according to the specific etiology. Among these lesions, MHs caused by lasers that use neodymium as a dopant and the host crystal yttrium aluminum garnet have been increasingly reported recently, but experience with their management is restricted to a few small case reports and series [8,9,11,13,15,16]. Also, evidence about detailed evaluation and longitudinal follow-up through the natural course of Nd:YAG laser-induced MHs is scarce in the literature [10-12,14,15].
Here, we described a case of an accidental MH caused by exposure to an Nd/YAG laser which was longitudinally evaluated by fundoscopy and SS-OCT during the first six weeks after the incident and treated with systemic steroids. This report adds evidence to the current knowledge about the natural progression of Nd/YAG laser-induced MHs, complementing previous illustrations of the clinical findings that characterize this type of retinal lesions during the acute phase [8,9,11,12,15]. In this regard, the literature available indicates that the most frequent manifestations of Nd/YAG laser-induced MHs are central scotoma and decreased visual acuity. The initial BCVA might vary from 20/20 when the lesion is parafoveal to 20/200-400 in central MHs [11]. On fundus examination, it is also possible to observe vitreous and subretinal hemorrhages that reabsorb during the first one-to-two weeks after the injury. Similar characteristics were found in our case, showing that inflammatory infiltrates with parafoveal swelling can also be part of the retinal changes induced by Nd/YAG lasers, as previously described by Sou and colleagues [8].
The MHs associated with Nd/YAG lasers might be apparent since the first evaluation, as demonstrated here, or develop during the following two weeks [8,9,11,12,15]. In some other cases, the laser trauma does not lead to full-thickness retinal destruction, and these incomplete lesions might be covered by an epiretinal layer which subsequently reabsorbs, resulting in minimal visual deficit [10,15]. Long-term characteristics of laser-induced MHs have not been studied extensively. Some reports indicate that MHs and BCVA stabilize after a few months, as observed in our case, whereas some might increase in dimensions over time, and others can close spontaneously [11,14]. Importantly, Nd/YAG laser-induced full-thickness MHs do not form chronic subretinal neovascularization and epiretinal membranes compared to less severe lesions generated with other lasers [11]. Without surgical treatment, visual loss ranges from complete recovery to persistent central scotoma, depending on the distance between the lesion and the foveal center [11].
The benefits of medical and surgical management for accidental MHs are not well established. The case described in this report showed a partial symptomatic improvement with the administration of prednisone. Systemic corticosteroids remain the main treatment for laser injuries and are administered as an attempt to decrease the extent and expansion of damage to the retina by reducing the local inflammatory reaction [6,11,15]. Generally, they are prescribed in doses of 1 mg/kg/day with weekly tapering. However, the effect of corticosteroids on visual acuity might be modified by several factors, including the extent of damage to the retinal pigment epithelium, the time of treatment initiation, and the distance of the trauma with the fovea [11,15].
Finally, there is no consensus on the curative potential of surgery and the most appropriate approaches to limit visual loss in individuals with MHs caused by Nd:YAG lasers. Qi et al., in a series of 11 patients with MHs generated by incidental laser damage [16], found that 100% of them closed after surgery using Pars Plana Vitrectomy (PPV), peeling of the ILM, and tamponade with gas or silicone oil, and visual acuity significantly improved in the postoperative follow-up. Also, in another study conducted by Wang et al. [17], the authors found that treatment with PPV, ILM peeling, and gas tamponade can be successful in closing laser-induced full-thickness MHs and improving visual acuity. However, outcomes might vary according to the presence of preoperative retinal pigment epithelium destruction, choroidal ischemia, and level of preoperative visual acuity.
In conclusion, Nd/YAG laser-induced full-thickness MHs are increasingly reported worldwide, but controversies remain about their management. Our report adds illustrative reference data about the longitudinal clinical and SS-OCT characteristics of these lesions during the acute phase and their response to prednisone administration. Additional longitudinal studies with a larger sample size are still required to assess the benefits and effectiveness of corticosteroids and surgery for retinal laser injuries.
Acknowledgement (optional)
To the patient and his relatives for their collaboration in the publication of the case.
Study Approval Statement
Not applicable.
Consent to Publish Statement
The patient provided written informed consent for the publication of the details of their medical case and any accompanying images according to the Declaration of Helsinki.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The current report did not receive financial support.
Author’s Contribution
Design of the study: MBS, JVL. Patient´s evaluation and management: MBS, JVL, EVR, MAD. Clinical data retrieval: MBS, EVR, MAD. Drafted the manuscript: MBS, EVR, JCP. Revision and corrections: JCP, JVL. All the authors approved the manuscript in its final version and met authorship requirements.
Data Availability Statement
The anonymous clinical data of this case report are available from the corresponding author upon reasonable request.
References
- Findl O, Buehl W, Bauer P, Sycha T (2010) Interventions for preventing posterior capsule opacification. Cochrane Database Syst Rev 2010: 003738.
- Kokavec J, Wu Z, Sherwin JC, Ang AJ, Ang GS (2017) Nd:YAG laser vitreolysis versus pars plana vitrectomy for vitreous floaters. Cochrane Database Syst Rev 6: 011676.
- Rivera AH, Brown RH, Anderson DR (1985) Laser iridotomy vs surgical iridectomy. Have the indications changed? Arch Ophthalmol 103: 1350-1354.
- Cinotti AA, Maltzman BA, Cinotti DJ, Shapiro E (1985) The Nd:YAG laser in ophthalmology. N J Med 82: 787-791.
- Gilmour MA (2002) Lasers in ophthalmology. Vet Clin North Am Small Anim Pract 32: 649-672.
- Wolfe JA (1985) Laser retinal injury. Mil Med 150: 177-185.
- Kumawat D, Venkatesh P, Brar AS, Sahay P, Kumar V, et al. (2019) ATYPICAL MACULAR HOLES. Retina 39: 1236-1264.
- Sou R, Kusaka S, Ohji M, Gomi F, Ikuno Y, et al. (2003) Optical coherence tomographic evaluation of a surgically treated traumatic macular hole secondary to Nd:YAG laser injury. Am J Ophthalmol 135: 537-539.
- Boldrey EE, Little HL, Flocks M, Vassiliadis A (1981) Retinal injury due to industrial laser burns. Ophthalmology 88: 101-107.
- Alhalel A, Glovinsky Y, Treister G, Bartov E, Blumenthal M, et al. (1993) Long-term follow up of accidental parafoveal laser burns. Retina 13: 152-154.
- Thach AB, Lopez PF, Snady-McCoy LC, Golub BM, Frambach DA (1995) Accidental Nd:YAG laser injuries to the macula. Am J Ophthalmol 119: 767-773.
- Lam TT, Tso MO (1996) Retinal injury by neodymium: YAG laser. Retina 16: 42-46.
- Ciulla TA, Topping TM (1997) Surgical treatment of a macular hole secondary to accidental laser burn. Arch Ophthalmol 115: 929-930.
- Hagemann LF, Costa RA, Ferreira HM, Farah ME (2003) Optical coherence tomography of a traumatic Neodymium:YAG laser-induced macular hole. Ophthalmic Surg Lasers Imaging 34: 57-59.
- Park DH, Kim IT (2009) A case of accidental macular injury by Nd: YAG laser and subsequent 6 year follow-up. Korean J Ophthalmol 23: 207-209.
- Qi Y, Wang Y, You Q, Tsai F, Liu W (2017) Surgical treatment and optical coherence tomographic evaluation for accidental laser-induced full-thickness macular holes. Eye (Lond) 31: 1078-1084.
- Wang X, Zhang T, Jiang R, Xu G (2021) Vitrectomy for laser-induced full-thickness macular hole. BMC Ophthalmology 21: 135.
Citation: Bayram-Suverza M, Vázquez-Ramírez EI, Alcántara-Delgado MA, Villar-López J (2022) Longitudinal Evaluation of an Acute Nd:YAG Laser-Induced Macular Hole: A Case Report. J Ophthalmic Clin Res 9: 095.
Copyright: © 2022 Mauricio Bayram-Suverza, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

