
Pineal Gland Mass presenting as Parinaud Syndrome in a 21 Year Old Patient
*Corresponding Author(s):
Patricia Abigail LimDepartment Of Ophthalmology, Rizal Medical Center, Pasig Boulevard, Pasig City, Philippines
Email:patriciaabigaillim@gmail.com
Abstract
We report a case of a 21-year-old Filipino, with a history of progressive diplopia, who presented with headache, dizziness and vomiting. Ophthalmologic exam revealed light near dissociation, physiologic anisocoria, bilateral upgaze palsy, convergence retraction nystagmus and pseudo-abducens palsy of the left eye. Imaging was done, which revealed pineal neoplasm with obstructive hydrocephalus. This text aims to present a case of pineal gland neoplasm which presented as diplopia alongside signs and symptoms of Dorsal Midbrain Syndrome (Parinaud Syndrome).
Parinaud Syndrome (PS) is a sporadic condition, with a classic triad of up gaze palsy, convergence nystagmus, and pupillary light near dissociation. It occurs due to compression of the rostral midbrain and pretectum at the level of the superior colliculus. Neuroimaging via MRI is often required for diagnosis. Management of PS lies in treating the underlying condition, in this case a pineal gland tumor. Surgical treatment, such as the Endoscopic Guided Biopsy of pineal neoplasm and venticuloperitoneal shunting, left-sided with left tube Ventriculostomy, as was done in our patient, is an option for treatment.
Keywords
Convergence Retraction Nystagmus; Diplopia; Dorsal midbrain syndrome; Light near dissociation; Parinaud syndrome, Pineal Neoplasm; Pseudo abducens palsy
Introduction
Parinaud Syndrome involves supra-nuclear vertical gaze palsy secondary to lesions damaging the vertical gaze center in the posterior commissure of the dorsal midbrain. The classical triad of this syndrome consists of 1) paralysis of conjugate up gaze, 2) light-near dissociation of the pupils and 3) convergence-retraction nystagmus during attempted upward saccades. However only about 65% of cases presents with all three. Conversely other sign and symptoms may be present such as: blurring of vision, visual field defect, ataxia, manifest squint, lid retraction. The most common causes are pineal gland tumors and midbrain infarction. According to studies, 65% of cases are due to primary midbrain lesions like strokes, hemorrhages, and neoplasms. To elaborate, 30% of cases were due to Pineal gland tumors causing pressure on the reflex centers in the dorsal midbrain [1].
Case
One year prior to consult, patient complained of intermittent binocular horizontal diplopia on primary gaze. Diplopia was of sudden onset, relieved by rest, but with no aggravating factor. This was accompanied by intermittent generalized headache, squeezing in character and with pain scale varying from four to six out of ten. Patient had episodes of headache relieved by rest and Ibuprofen. No further consults or interventions were done.
One month prior to consult, patient had sudden onset of binocular horizontal diplopia now on all gazes with no noted aggravating factors. Increased intensity of headaches as well as occurrence of intermittent dizziness and vomiting was noted.
Two weeks prior, patient was brought to a local primary hospital due to persistence of symptoms. He was admitted for observation and discharged two days after with a final diagnosis of peptic ulcer disease. Patient was given Omeprazole 40mg/tab, one tab once a day before breakfast for 14 days which afforded no relief of symptoms.
Ten days prior, patient still with persistence of diplopia and accompanying symptoms, hence was brought to another local hospital. Laboratories done which allegedly showed normal results. He was then given unrecalled antibiotics.
However, patient still with no improvements, was brought to a local tertiary hospital one week prior to consult. A Computed Tomography (CT) scan was then done which revealed a neoplasm of the pineal gland. Patient was then referred to our institution for further evaluation and management. For a holistic approach, patient was referred by the neurosurgery service to the Ophthalmology service for evaluation of papilledema.
At the time of ophthalmologic examination patient was in pain, with a Glascow Coma Scale (GCS) of 14 (E4V4M6) and intermittently follows commands. Bedside examination reveals best correct visual acuity (BCVA) of J5 on right eye, J7 on the left eye. Color vision with the use of Ishihara test was 15/15 plates on both eyes. Confrontation test revealed no gross defect on all quadrants tested. On Hirschberg, the pupillary light reflex fell on the midpupil of both eyes. On checking the pupil, physiologic anisocoria was noted and light near dissociation was observed (Figure 1). Patient also presented with bilateral upgaze deficit and pseudo abducens palsy, left eye (Figure 2 and Videos 1 & 2). Convergence retraction nystagmus was also elicited (Figure 3).
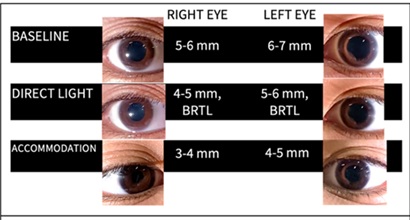 Figure 1: Pupillary response to light and near.
Figure 1: Pupillary response to light and near.
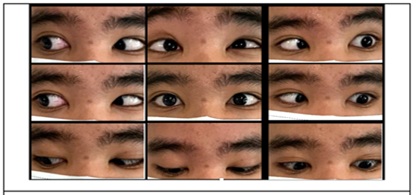 Figure 2: Extraocular motility
Figure 2: Extraocular motility
 Video 1: Extraocular motility video.
Video 1: Extraocular motility video.
 Video 2: Convergence retraction nystagmus video.
Video 2: Convergence retraction nystagmus video.
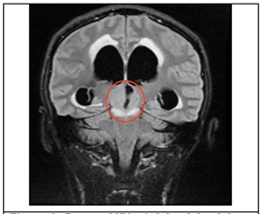 Figure 3: Repeat MRI. A 2.8 × 2.9 × 2.8 cm (CC × W × AP) fairly-defined, lobulated and heterogeneously enhancing lesion with restricted diffusion, intermediate-T2/FLAIR and slightly hypointense-T1W signals is seen in the pineal region, almost completely effacing the quadrigeminal cisterm. A small hypointense round focus with magnetic susceptibility is further noted within the said mass.
Figure 3: Repeat MRI. A 2.8 × 2.9 × 2.8 cm (CC × W × AP) fairly-defined, lobulated and heterogeneously enhancing lesion with restricted diffusion, intermediate-T2/FLAIR and slightly hypointense-T1W signals is seen in the pineal region, almost completely effacing the quadrigeminal cisterm. A small hypointense round focus with magnetic susceptibility is further noted within the said mass.
Forced duction testing showed no resistance. On doll’s eye testing, patient was able to overcome extraocular movement limitations. Patient also presented with good bell’s phenomenon. Anterior chamber exam using ophthalmoscope revealed clear cornea, deep looking chambers, and clear lens for both eyes. Funduscopic findings of both eyes revealed: positive red- orange reflex, clear media, distinct disc border, 0.3 cup-disc ratio, 2:3 artery: vein ratio, no hemorrhages or exudates seen. Cranial nerves were normal with the exception of the Extraocular Muscle (EOM) limitation. Motor and sensory findings were also normal.
A Magnetic Resonance Imaging (MRI) showed Pineal germ cell tumor with possible involvement of the midbrain, associated obstructive hydrocephalus and transependymal effusion (Figure 3).
There was a dramatic decrease in the level of sensorium of the patient following the ophthalmologic assessment. Hence, the Neurosurgery service performed emergency Endoscopic Guided Biopsy of Pineal Neoplasm and Ventriculoperitoneal (VP) shunting, left and Left tube Ventriculostomy.
Discussion
Dorsal midbrain syndrome also known as Parinaud syndrome is due to the Compression of the rostral midbrain and pretectum at the level of the superior colliculus.
According to literatures, the etiology of PS differs with age. Neoplastic causes are more common in children and young adults, such as our patient. Vascular causes are more common in the middle-aged and elderly [1,2]. Furthermore in a 25 year review of parinaud cases by Shields et al, Pineal lesions causing pressure on the reflex nuclei of the quadrigeminal plate are the classic cause of PS and were responsible for 30.0% of cases [1]. This is again consistent with our case which revealed in which the imaging revealed a pineal gland lesion.
Parinaud syndrome usually presents with a classic triad of up gaze palsy, convergence nystagmus, and pupillary light near dissociation [2]. Furthermore, patients may also present with complaints of diplopia, blurred vision, visual field defect, ataxia, manifest squint and collier lid retraction [1].
Our patient first complained of diplopia. On physical examination, vertical gaze palsy, convergence nystagmus, light near dissociation, poor visual acuity were also elicited. According to shields et al, only 65% of patients with PS present with the classical triad, even less present with each and every symptom listed above [1].
Our patient’s chief complaint diplopia happens to be the most common presenting symptom in patients with PS. This may be explained by skew deviation or associated unilateral or bilateral cranial nerve IV palsies [3].
The vertical gaze palsy seen in patients with Parinaud results from the involvement of the posterior commissure, interstitial nucleus of Cajal or the rostral interstitial nucleus of medial longitudinal fasciculus (riMLF) which is involved in the vertical gaze pathway. Posterior commissure is said to be very susceptible to increased CSF pressures which may be the case in our patient since his imaging findings present with hydrocephalus. Furthermore, in patients with PS, downgaze may be spared due to the difference in pathway; upgaze projections from riMILF traverse through the Posterior commissure while for downgaze, direct projection from riMILF to CN 3 and CN4 nuclei ensues [3,4].
Further distinction can be observed that while our patient has an upgaze palsy both doll’s eye maneuver and bell’s phenomenon remained normal. In focal lesions: only saccades: upward, downward, or saccades in both directions. In a chapter from Neuro- ophthalmology Illustrated on Diplopia by Talmage Cooper, he states that in focal lesions such in our patient only saccades (either upward, downward, or both directions) are affected; eye movements by vestibular stimulation and forced eye closure (Bell’s phenomenon) are spared [5].
Light near dissociation presents with poor pupillary constriction to light but preserved constriction with convergence. According to literature, nuclei for the pupillary light reflex are thought to lie more dorsally than for near reflex, making them more susceptible to compressive effects [3].
Convergence retraction nystagmus seen in our patient is not a true nystagmus. These are quick phases that converge and retract both eyes upon up gaze. This is said to be die to damage to Inhibitory fibers of the rectus muscles causing excess convergence tone. Damage of the midbrain supranuclear fibers cause an inhibitory effect on the CN 3 nucleus, preventing activation of the EOMs innervated by CN 3. As a result, superior rectus and inferior rectus muscles receive constant stimulation, resulting in retraction of the globe. Additionally, stimulation of the middle rectus overpowers the lateral rectus leading to involuntary convergence [3].
Pseudo- abducens palsy is characterized by failure of ocular abduction which is not due to dysfunction of the sixth nerve. This is thought to be caused by increased convergence activity. Further physical examination finding in our patient that points to a pseudo abducens palsy more than a true CN 6 palsy is that Doll’s eye maneuver overcame abduction deficit. Thus while apparent impairment in lateral gaze is observed, intact vestibulo-ocular reflex demonstrates full abduction as seen when doll eye maneuver overcame limitation of EOM. The intact VOR a indicates the integrity of the infranuclear abducens nerve, thus suggesting that a pseudo-abducens palsy is likely caused by supranuclear pathology such is the case of our patient [6].
Management of PS lies in treating the underlying condition [1]. Such as in our case, patient underwent Endoscopic Guided Biopsy of Pineal Neoplasm and VP shunting, left with Left tube Ventriculostomy. Symptoms may completely be reversed in patients with early hydrocephalus. Conservative management are sufficient in most cases although surgical treatment of upgaze palsy can be a useful option in refractory cases.
Conclusion
Parinaud syndrome usually results from Pineal Gland lesions (tumors) affecting the structures in the dorsal midbrain.
Diplopia is the common presenting sign of patients with PS. Of patients with PS, only 65% present with the classical triad of up gaze palsy, convergence nystagmus, and pupillary light near dissociation. Neuroimaging with MRI is suggested for all patients with symptoms suggestive of PS.
Management of patients with PS rely heavily on finding cure of the underlying condition.
References
- Shields M, Sinkar S, Chan W, Crompton J (2017) Parinaud syndrome: a 25-year (1991-2016) review of 40 consecutive adult cases. Acta Ophthalmol 95: e792–e793.
- Frank A, Weber C, Bendig J, Schaefer J (2022) Teaching video NeuroImage: Parinaud syndrome due to ventriculoperitoneal shunt malfunction in a patient with neurosarcoidosis. Neurology 98: 947-948.
- Liu G, Volpe N, Galetta S (2018) neuro-ophthalmology: diagnosis and management. Edinburgh: Elsevier Inc;
- Ocular motor control (section 3, chapter 8) (2020) Neuroscience Online, an Open-Access Neuroscience Electronic Textbook, Neuroscience.
- Cooper T (2020) Neuro-ophthalmology illustrated chapter 13 diplopia 13 – localization of findings & treatment of diplopia - syndromes - neuro-ophthalmology.
- Reid MS, DePoe SA, Darner RL, Reid JP, Slagle WS (2015) Clinical presentation of pseudo-abducens palsy. Optom Vis Sci 92: S76-S80.
Citation: Lim PA, Ang L (2022) Pineal Gland Mass presenting as Parinaud Syndrome in a 21 Year Old Patient. J Ophthalmic Clin Res 9: 101.
Copyright: © 2022 Patricia Abigail Lim, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

