Response Rates of rTMS Treatment for Depression at Tranquil TMS - a UK-based Clinic
*Corresponding Author(s):
Nikhila DeshpandeFounding Director And Consultant Psychiatrist, Tranquil TMS, United Kingdom
Tel:+44 08001930914,
Email:nikhilad@hotmail.com
Abstract
Background
There is strong evidence supporting efficacy of repetitive Transcranial Magnetic Stimulation (rTMS) in the treatment of depression. There is a paucity of research in the UK in this area.
Aims
The aim of the study was to measure the response rate of rTMS in depression in the UK population.
Methods
Patients attending Tranquil TMS clinic at North West of England from the 1st Feb 2018 to 31st Dec 2019 were included in the study. HDRS and HAM-A applied before and at the end of the treatment to measure the response rate. This was then compared to response rates for similar patient groups from international studies.
Results
This sample showed remission rate of 37.03%. Response rate was 66.66%. Dropout rate was 18.18% which was unrelated to rTMS treatment.
Conclusion
The study once again shows the efficacy of rTMS in the treatment of depression. There is a need of further research in this area in the UK population.
Keywords
Depression; rTMS
INTRODUCTION
The treatment of depression has continued to evolve over the years. Despite newer antidepressant medications, the STAR-D trial has clearly shown the limitations of psychopharmacology in the treatment of depression [1]. In recent times, neuromodulation has provided a ray of hope for that section of the population whose symptoms fail to respond to traditional measures.
One of these neuromodulation treatments, repetitive Transcranial Magnetic Stimulation (rTMS) has been shown to be an effective treatment for depression. In the UK, rTMS has been approved for the treatment of depression by the NICE in 2015 and the Royal College of Psychiatrists in 2017. In the USA, the FDA has approved this treatment for treatment-resistant depression in 2008 [2]. Health Canada has approved this treatment for the treatment-resistant depression in 2002 [3].
NICE Guidance IPG542 (December 2015) states. The evidence on repetitive transcranial magnetic stimulation for depression shows no major safety concerns. The evidence on its efficacy in the short?term is adequate, although the clinical response is variable. Repetitive transcranial magnetic stimulation for depression may be used with normal arrangements for clinical governance and audit [4]. Studies have shown that repetitive Transcranial Magnetic Stimulation (rTMS) has a definite antidepressant effect on major depression [5]. The evidence suggests that rTMS used solely or in combination with antidepressants for first-episode major depressive disorder may be more effective than antidepressants alone. Thus, the use of rTMS may shorten the treatment odyssey for patients with MDD [6].
Aim
The aim of this study is to evaluate the success rates of the rTMS in the treatment of depression in private North West UK-based clinic.
The general consensus is that 1in 3 patients achieve complete remission by the end of 1 year and that 1in 2 patients will show a 50% reduction in their symptoms with the rTMS [7].
We expect patients to halve their scores on two different rating scales -Hamilton Depression Rating Scale (HDRS) and Hamilton Anxiety Rating Scale (HAM-A) by the end of their treatment course (which could last 4-6 weeks) in order to consider it a response to treatment.
For HDRS scores, any score of 7 or under is regarded as remission. The HAM-A scores of 10 or under were regarded as remission for the purpose of this study.
Methods
We analysed data of all the patients who received rTMS treatment in Tranquil TMS from 1st Feb 2018 to 31st Dec 2019. We used 2 rating scales, Hamilton Depression Rating Scale (HDRS) and Hamilton Anxiety Rating Scale (HAM-A).
All patients undertook HDRS and HAM-A assessments at the beginning of the treatment and this was then repeated at the start of every week of their treatment subsequently. For the purposes of this study, we decided to only include the scores from the start of the treatment and following the completion of the treatment.
Results
During the study period, 33 patients commenced rTMS treatment. Out of this number, 6 patients dropped out by the end of the 1st week (18.18%). The reasons for dropouts were varied-2 people thought clinic was geographically too far to commute, 3 patients changed their mind within the first few days regarding the treatment and 1 had a family incident - but none of the dropouts were due to side effect issues.
Our sample included 27 patients all of whom were on at least 1 antidepressant medication and showing no significant response to it. Only 4 patients were drug naive. 27 patients out of 33 (81.81%) completed the treatment see (Table 1) Out of those, 9 patients received intermittent theta bursts protocol (50 Hz) for depression whilst 18 patients received standard protocol for depression (10Hz).
|
HDRS initial |
HDRS Final |
HAM-A Initial |
HAM-A final |
|
|
Patient 1 |
14 |
5 |
24 |
5 |
|
Patient 2 |
27 |
3 |
26 |
3 |
|
Patient 3 |
31 |
24 |
33 |
27 |
|
Patient 4 |
15 |
8 |
29 |
12 |
|
Patient 5 |
11 |
3 |
26 |
4 |
|
Patient 6 |
30 |
21 |
41 |
32 |
|
Patient 7 |
22 |
10 |
34 |
16 |
|
Patient 8 |
21 |
9 |
21 |
15 |
|
Patient 9 |
19 |
12 |
33 |
25 |
|
Patient 10 |
11 |
1 |
6 |
2 |
|
Patient 11 |
20 |
6 |
26 |
7 |
|
Patient 12 |
14 |
18 |
21 |
26 |
|
Patient 13 |
13 |
10 |
28 |
16 |
|
Patient 14 |
22 |
10 |
27 |
15 |
|
Patient 15 |
11 |
6 |
23 |
10 |
|
Patient 16 |
13 |
4 |
12 |
6 |
|
Patient 17 |
24 |
11 |
30 |
17 |
|
Patient 18 |
9 |
5 |
13 |
7 |
|
Patient 19 |
16 |
18 |
23 |
27 |
|
Patient 20 |
24 |
13 |
25 |
15 |
|
Patient 21 |
18 |
9 |
17 |
12 |
|
Patient 22 |
18 |
16 |
22 |
15 |
|
Patient 23 |
17 |
5 |
35 |
2 |
|
Patient 24 |
22 |
4 |
32 |
4 |
|
Patient 25 |
30 |
7 |
34 |
7 |
|
Patient 26 |
28 |
8 |
38 |
15 |
|
Patient 27 |
18 |
5 |
23 |
2 |
Table 1: below highlights the change in HDRS scores from initial to final rating scores.
Patients received 20-40 treatments of high frequency rTMS on the Left Dorsolateral Pre-frontal cortex and a minimum of 10 treatments of low frequency rTMS (1 Hz) on the right dorsolateral prefrontal cortex. Out of the 27, 2 patients (7.4%) are currently receiving maintenance treatment every few weeks
HDRS scores showed 12 out of the 27 patients achieved full remission at the end of the treatment (37.03%).Out of 27 patients 18 had achieved more than a 50% drop in HDRS score (66.66%).
On HAM-A scale see (Figure 1-3) below 12 out of the 27 patients achieved full remission with scores of 10 or under (37.03%). 17 out of 27 patients had achieved more than 50% drop in HAM-A score (62.96%).
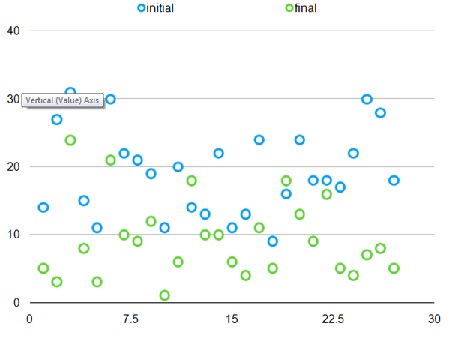 Figure 1: HDRS - Initial to final scores.
Figure 1: HDRS - Initial to final scores.
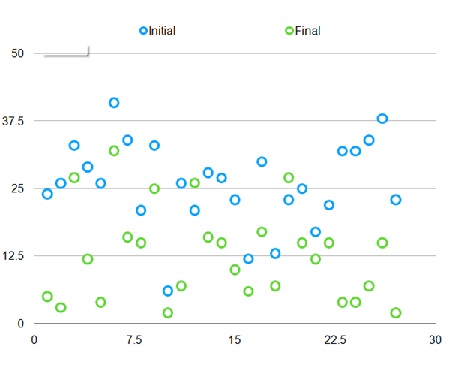 Figure 2: HAM-A - Initial to final scores.
Figure 2: HAM-A - Initial to final scores.
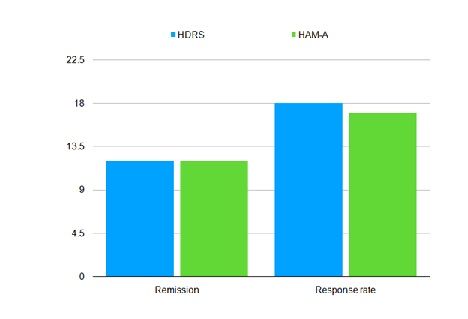 Figure 3: Remission and response rates.
Figure 3: Remission and response rates.
DISCUSSION
The study showed that our remission rate for rTMS was high (37.03%). This is comparable to the study done by Connolly et al, 2012 which showed the HDRS remission rate of 35.3% [8].
Our response rate (66.66%) was higher than the response rate of 41.2% quoted in the study by Connolly et al, 2012 [8]. Our rates were also higher than the metanalysis done by Berlim et al in 2014. Berlim et al carried-out analysis of the data from 29 RCTs covering 1371 patients. They found that 29.3% of patients responded to treatment and 18.6% of patients could achieve remission with high frequency rTMS [9].
We did not have any patients discontinuing the treatment because of the side effects of rTMS. Though our dropout rates were higher than other studies, they were not related to rTMS treatment as such. Once again, this study shows that rTMS is an effective treatment for depression including treatment resistant depression. HAM-A scores highlights the success of anxiety protocol in helping patients with co-existing anxiety symptoms. There is a dearth in the literature regarding rTMS experience in the UK. We recommend further studies with larger sample sizemainly targeting the UK’s population.
DECLARATION OF INTEREST
Nikhila Deshpande and Babu Nayar are the directors of Tranquil TMS.
REFERENCES
- Lonescu DF, Rosenbaum JF, Alpert JE (2015) Pharmacological approaches to the challenge of treatment-resistant depression. Dialogues in Clinical Neuroscience 17: 111-126.
- McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, et al. (2018) Consensus recommendations for the clinical application of repetitive Transcranial Magnetic Stimulation (rTMS) in the treatment of depression. J Clin Psychiatry 79: 16cs10905.
- Tu AH, Palimaka S, Sehatzadeh S, Blackhouse G, yap B, et al. (2016) Health quality ontario. Repetitive transcranial magnetic stimulation for treatment-resistant depression: An economic analysis. Ont Health Technol Assess Ser 16: 1-51.
- NICE (2015) Repetitive transcranial magnetic stimulation for depression. NICE, London, United Kingdom
- Lefaucheur JP, Andre?-Obadia N, Antal A, Ayache SS, Baeken C, et al. (2014) Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol 125: 2150-2206.
- Voigt J, Carpenter L, Leuchter A (2019) A systematic literature review of the clinical efficacy of repetitive transcranial magnetic stimulation (rTMS) in non-treatment resistant patients with major depressive disorder. BMC Psychiatry 19: 9-13.
- McDonald WM, Durkalski V, Ball ER, Holtzheimer PE, Pavlicova M, et al. (2011) Improving the antidepressant efficacy of transcranial magnetic stimulation: maximizing the number of stimulations and treatment location in treatment-resistant depression. Depress Anxiety 28: 973-980.
- Connolly KR, Helmer A, Cristancho MA, Cristancho P, Reardon JP (2012) Effectiveness of transcranial magnetic stimulation in clinical practice post-FDA approval in the United States: results observed with the first 100 consecutive cases of depression at academic medical centre. J Clin Psychiatry 73: e567-73.
- Berlim MT, Eynde FVD, Tovar-Perdomo S, Daskalakis ZJ (2014) Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med 44: 225-39.
Citation: Deshpande N, et al. (2020) Response Rates of rTMS Treatment for Depression at Tranquil TMS - a UK-based Clinic. J Psychiatry Depress Anxiety 6: 033.
Copyright: © 2020 Nikhila Deshpande, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.