
The Lived Experience of Chemo Brain in Early Stage Breast Cancer in Women 50 and Under
*Corresponding Author(s):
Patricia A GibbonsDoctor Of Philosophy In Nursing, Seton Hall University, United States
Tel:+1 9145250911,
Email:patricia.gibbons@student.shu.edu
Abstract
Cognitive deficits have been shown to affect those who have undergone treatment with chemotherapy. This is often referred to as chemo-brain. The purpose of this descriptive phenomenological study was to explore the lived experience of the chemo brain after undergoing chemotherapy for breast cancer. The study sample consisted of six women between the ages of 29 and 50 with early stage breast cancer. Descriptive phenomenological method guided data analysis. The recurrent themes identified in this study were (1) Struggles with day to day life (2) Emotions related to diagnosis and treatment, (3) Fatigue (4) Coping and support, and (5) Feeling grateful. Findings of this study confirm the existence of cognitive changes during and after chemotherapy and describe as well the effects on daily life including fatigue, emotions, and the importance of support. This study suggests the importance of educating both healthcare providers and patients about the cognitive changes related to chemotherapy and ways to cope with these changes.
INTRODUCTION
Problem
Researchers use different terminology, for example, cognitive impairment or chemo fog, to discuss the phenomenon of chemo brain, offer many factors to explain it, and use various tools to evaluate the different cognitive processes that are affected [4].
Although there are anecdotal accounts from healthcare providers, there is only minimal qualitative research that describes women’s experiences with chemo brain. According to [2] specific elements of thinking or cognitive function that can be negatively affected by chemo brain include language ability, memory, concentration, and attention.
Hindsight, foresight, and judgment can also be affected [5]. Describe chemo brain as having feelings of fuzzy headedness, or mental slowness, and patients who experience it often complain about weakened cognitive abilities, such as a diminution of their usual speed in processing information, poor reaction time and poor organizational skills. Patients offer examples such as not being able to remember where they put their keys, parked their cars, or who wrote the book they just finished reading[2]. Others complain they have trouble finding the right words to describe everyday things, such as a calculator, or a pencil [6]. In research using a case study method, cognitive dysfunction associated with chemotherapy was found to affect the ability of women with breast cancer to maintain usual family, career, and community responsibilities[7].
The Oncology Nursing Society (ONS) emphasizes the importance of the study of cancer symptoms and the side effects of treatment measures as a priority for research. They are particularly interested in neurological effects that include cognitive impairment and mental status changes [8]. Healthy People 2010 and 2020 cite increasing quality and years of a healthy life as one of its main, national healthcare goals and additionally, has named cancer related issues as a major research focus. The aim is to reduce the number of new cancer cases, as well as the illnesses, disabilities, and deaths caused by cancer [9]. Chemo brain, as a result of chemotherapy treatment of women diagnosed with breast cancer, is an important, and little understood phenomena both for the women using the healthcare system and for the professional nurses who are their major healthcare providers[10].Symptoms of chemo brain that significantly impact the quality of life for women with breast cancer who are receiving chemotherapy are evident in their daily lives; however, patients with manifestations of chemo brain often do not receive validation, treatment or education about these symptoms[11].Although chemo brain is reported in up to 90% of women receiving chemotherapy treatment for breast cancer, depth of knowledge related to it is lacking[3].Learning about the experience of chemo brain may ultimately improve the lives of women who experience it.
Problem statement
Assumptions
Aim of the study
Research method
Research question
Relevance to nursing
REVIEW OF LITERATURE
According to [2], Cognitive functions like language ability, memory, concentration, judgment, and attention can be negatively affected by chemotherapy. Patients describe chemo brain as being mentally slow as evidenced by lack of speed in processing information, having poor organizational skills, and having poor reaction time [5]. They offer examples such as not being able to remember who their favorite author is, where they parked their car in the mall, and where they put their keys [2]. They may also have trouble finding the right words to describe everyday things, such as a calculator, or a pencil [6]. Cognitive dysfunction associated with chemotherapy can affect the ability of women with breast cancer to maintain their usual daily responsibilities [20-24]. Have concluded that adjuvant chemotherapy causes neurochemical changes in the brain and can influence brain structure which may account for previously observed cognitive impairments. In addition, chemotherapeutic agents such as cyclophosphamide, adriamycin, methotrexate, fluorouracil, epirubicin, and paclitaxol, although once thought to have little ability to penetrate the blood-brain barrier, have been found in higher concentrations than expected in cerebrospinal fluid and brain tissue [24]. These drugs are hypothesized to have neurotoxic potential by interfering with DNA and RNA synthesis and function, inhibition of microtubule formation, and/or immunosuppressive properties [24].
Similarly, [25] also found that some chemotherapeutic agents affect neuroanatomic structures which can have an effect on cognitive function. These researchers found that neurotoxicity associated with specific chemotherapies can be caused by leukoencephalopathy, cytokine-induced inflammatory response in brain tissue, chemotherapy-induced anemia affecting oxygen carrying ability of the blood, and chemotherapy- induced menopause that triggers hormone imbalances. Each of these changes may affect the overall structure and function of the brain and result in chemo brain.
Historical perspective
Experiential context
In my clinical experience, I have observed that patients are frustrated and concerned about the loss of cognitive abilities that most of us take for granted. Healthcare professionals are just starting to recognize this symptom as a side effect of chemotherapy, but do not know how to evaluate it or treat it.
Gaps in the literature
According to [4], more than 80 instruments have been used to assess various attributes of cognitive function in patients with cancer and no current standard exists for measurement or assessment of cognitive function in cancer patients. [31] Reviewed 91 eligible articles regarding cognitive impairment between August 2010 and February 2014 to determine if evidence-based interventions existed for cancer and treatment- related cognitive impairment. They were able to break down interventions into four categories: likely to be effective, effectiveness not established, effectiveness unlikely, and not recommended for practice. Information about chemo brain and interventions used to treat it are still lacking.
Nurses can offer support and assess for aspects of cognitive impairment but, knowledge about intervention and treatment will remain limited because of inadequate identification and inconsistent measures of the phenomenon of chemo brain.
Qualitative research that describes the lived experience of chemo brain in women with early stage breast cancer remains limited [28].Studied the lived experience of self- reported cognitive impairment in women treated with chemotherapy for breast cancer. She interviewed 10 women between the ages of 18 and 75 who had received chemotherapy in the 15- 52 months prior to the interview. Similarly[14],explored the experience of neurocognitive changes experienced by women with breast cancer undergoing chemotherapy.
The women in this study were currently being treated or had completed chemotherapy with 12 months of the study. The 13 participants were between 35 and 62 years old. [15] Specifically studied chemo brain in underserved African American breast cancer survivors by conducting focus groups. Findings of [14,28] Thielen’s and Mulrooney’s studies revealed that symptoms of chemo brain often started out as vague, but were cumulative, related to dose and worsened with each treatment and impacting all aspects of the lives of the women in these studies, while Rust and Davis found chemo brain to be variable among the women they studied [28].
Identified three dominant themes as a result of qualitative analysis: “I just don’t feel like me,” “trying my best to live with it” and “I am alive.” Participants in this study stated that they had problems with memory, concentration, learning, language and multitasking and that chemo brain could occur at any time during treatment and had an impact on their ability to perform their usual activities. Coping mechanisms for these women were practical, but self-esteem was sometimes negatively affected. Some women reported more isolation from family and friends while others reported greater emotional support; however, all of the women felt that surviving was the most important thing of all [14].Identified eight similar themes following analysis which included: “Insidious recognition and delayed validation of cognitive changes,” “Looking for answers in all the wrong places,” “Attention: Can’t keep my eye on the ball,” “Underwhelming information for an overwhelming experience,” “Work department: Hold please,” “Missing Label: Caution: Woman on chemotherapy on board,” “Coping: Not on the cancer journey alone” and “What the future holds.” Women in this study found a decrease in cognitive function related to chemotherapy to be insidious and multi-factorial, yet were very resourceful in finding ways to cope and compensate with concentration and memory impairment. They were optimistic that changes in cognitive function were temporary and reversible and most of the women in this study had great support from family and friends [15].
Discussed four themes that overlapped with the themes of Thielen and Mulrooney. They included: the concept of chemo brain, variability among individuals, the stigma of chemo brain, and methods of coping. They found that individuals studied did not use health professionals as a resource for education and support during their experience of chemo brain. They concluded that nursing professionals are in the frontline of care and should be a resource for breast cancer survivors by providing information, education, and coping methods during the cancer journey. This, they hypothesized, would improve quality of life for breast cancer survivors.
Although these three studies examined cognitive changes in women with breast cancer, none of the studies exclusively addressed women 50 years of age and younger. Women in this age group often have different family, work, and social responsibilities that can be impacted by the effects of chemo brain [7,32] state that cognitive dysfunction associated with adjuvant chemotherapy can affect the ability of women with breast cancer to maintain usual family, career, and community responsibilities. Women age 50 and under may have jobs that require higher cognitive functioning such as a business executive, university faculty or a lawyer. They may have multiple responsibilities that require them to multi-task in their daily lives at work as well as at home.
They also have less diminished cognitive effects that could be accounted for by age-related changes that may occur in the absence of disease[16], and therefore may have a different experience with chemo brain. The aim of this study is to gain a better understanding of chemo brain in women 50 years of age and under.
Summary
METHODOLOGY
Rationale for choosing method
Background
Translation of concepts and terms
Hermeneutics: To interpret or translate [34]
Hermeneutic Phenomenology: Is a qualitative research methodology that asks for meanings of a phenomenon with purpose of understanding human experience as it is lived [39].
Being: The nature or the meaning of a phenomenon [40].
Bracketing: Is a fundamental strategy in phenomenology which differentiates the chasm between phenomenology as a philosophy and as a research endeavor [41].
Being in the world: The way in which human beings act and exist in the world [1].
Lifeworld: The world of lived experience as described by Husserl. “The world of immediate experience, the world as already being there “[40].
Essence: The nature of an experience is adequately described in language when the description reawakens or shows us the lived meaning or significance of the experience in a fuller or deeper manner[1].
General steps
The second step involves investigating the experience as it is lived rather than as conceptualized. In this step, the phenomenon is explored by using personal experience as a starting point, tracing the etymological sources, searching idiomatic phrases, obtaining experiential descriptions from participants, locating experiential descriptions in literature and art, and consulting phenomenological literature [40].
The third step in van Manen’s method is phenomenological reflection. In this step, thematic analysis is conducted by uncovering thematic aspects in lifeworld descriptions, isolating thematic statements, composing linguistic transformation and gleaning thematic descriptions from artistic sources by reflecting on them, recreating them, and transcending them [40].
The fourth step is the phenomenological writing. In this step, the researcher focuses on the language, varying of examples and writing and rewriting. This is particularly important because in this step, the quality of writing makes the story become more compelling to both the researcher and to those that read it.
The fifth step involves manipulating a strong and oriented pedagogical relation to the phenomenon. In this step, rich, thick descriptions of the lived experience will help to give depth to the true meaning of the experience.
The final step is to balance the research context by considering both the parts and the whole, and by taking into account all ethical considerations and knowing that the researcher may affect and be affected by the research [40].
APPLIED METHODOLOGY
Aim
Participants
Flyers were placed in private oncology practices in New York City and Westchester where participants were to be obtained; however, this recruitment strategy was not effective and participants were recruited through networking with nurses and friends through word of mouth.The women were asked to describe what it was like for them to experience chemo brain. In qualitative research, sample size is not determined by the need to ensure generalizability, but by data saturation [36]. In this study data saturation was reached with 6 participants. At that point, there was no new information provided. Participants included women age 50 and under with early stage breast cancer (stages I &II) who had the experience of chemo brain. The women ranged in age from 30-50, with one woman 29 about to turn 30, two others 38, the fourth 42, the fifth 46 and the last woman, 50.
All of the women except for one (who had just completed chemotherapy) had completed chemotherapy within the previous 6 months and none except one required Herceptin therapy because of her HER2 positive hormone receptor status. All of the women were premenopausal prior to receiving chemotherapy and because of that; all were required to take Tamoxifen for 5 years after chemotherapy. All of the women were well educated and performed jobs that required high cognitive functioning. Two of the participants were teachers, but one was a stay at home mom since she was diagnosed while on maternity leave, 3 were nurses, but one of three was working in business instead of nursing and the sixth was retired from owning her own business. These women had multiple life responsibilities that required multi-tasking in their daily lives and were invited to participate because they had personal knowledge about the experience of chemo brain.
Setting
Gaining access and establishing rapport
Membership in a professional organization like ONS, as well as my in-depth oncology experience working with women with breast cancer, and the fact that I am a woman, did help to enhance my credibility as a researcher and helped to establish trust and rapport with participants.
In order to gain access to potential participants, the presidents of the local ONS chapters were contacted to ask for permission to speak at the monthly meetings. The study was described to nurses at the local chapters of the organizations to which I belonged, and I distributed a recruitment flyerthat contained information about the study and contact information for potential participants. Women who were interested in participating could contact me directly. Private oncology practices were also contacted by a written letter where I asked potential participants to pass the study information along to fellow breast cancer patients in anticipation that this word of mouth communication would help to create a “snowball effect”.
At the local chapter meetings of ONS, I presented the purpose of my research to oncology nurses who work in private practice settings in order to gain access to potential participants. I also asked oncology nurses to pass the word on to other colleagues in the private setting. I provided a flyer outlining my proposed research to those women who might be interested in participating in this study. This flyer described the study and included the eligibility and contact information along with a statement informing participants that they would be asked questions about their experience with chemo brain after chemotherapy. The flyer stated that there was no monetary compensation for participating. Potential participants were provided with a letter of invitation. I explained to the nurses that when a woman would contact me, the proposed number of interview sessions, the amount of time for each interview, and information related to data collection and assurance of confidentiality would be provided.
I did not receive any participants via this formal method; however, I did speak to colleagues and friends about my proposed research and was able to get participants through word of mouth. All of the participants were gained through this method.
General steps in data collection
|
Participant Name N=6 |
Age |
Ethnicity |
Educational Level |
Job |
|
Sherry |
42 |
Jamaican |
MSN |
Nurse |
|
Julie |
38 |
Caucasian |
BSN |
Nurse |
|
Cathy |
30 |
Caucasian |
M. Ed |
Teacher |
|
Carol |
50 |
Caucasian |
BBM |
Retired business owner |
|
Tina |
38 |
Filipino |
BA |
Business executive |
|
Sheila |
47 |
Caucasian |
M. Ed |
Teacher |
Audiotapes were transcribed verbatim and reviewed by me while simultaneously being checked for accuracy. Once accuracy had been confirmed, initial data analysis was begun. This helped to identify additional questions for future interviews as well as identify any content that needed further clarification. At the end of each interview sessions, participants were thanked for their time and participation and were asked for their permission to contact them should further clarification be needed. At the end of each interview, participants were provided with a 25.00 Starbucks gift card as a token of appreciation for participating.
Analysis
These criteria comprise four domains that include; credibility, transferability, auditability, and confirmability. The principle of credibility is one of the most important elements of trustworthiness because it allowed me, the researcher to demonstrate that the findings are based in reality [42]. Qualitative studies are credible when they provide rich descriptions and interpretations of the phenomenon under study such that those who have had the experience would recognize the experience as their own or others can identify with the study just by reading it [42,43].I was able to identify with the experience of chemo brain just as others reading the study could because of the rich descriptions and examples that the participants provided.
Three elements can enhance credibility in qualitative research. They are prolonged engagement, persistent observation, and triangulation of the data [42].
Prolonged engagement refers to the time the researcher spends establishing trust, understanding the culture and clarifying information [42].This allows the researcher and participant to build a relationship based on trust and understanding and will begin with the first interview. Credibility was enhanced by meeting each participant at their desired location. I went to two participant’s homes for initial interviews as well as a follow up interviews. I scheduled a study room in the library for another participant in order to provide a quiet and private environment. I met another in a Starbucks near her job in downtown Manhattan for her interviews. The fifth participant asked me to meet her at her job for both of her interviews and the sixth set of interviews took place in a hotel. Each time I interviewed a participant, I would bring pastries and a Starbucks gift card as token of my appreciation for their participation in my study. By making myself available to each participant and meeting them where it was most convenient for them, I was able to easily gain access.
During the interviews, I observed and recorded observations in field notes. I often observed crying, anxiety, forgetting and scatterbrained behavior during these sessions. Continued observation along with writing field notes was an important part of the interview and data collection process. Reviewing field notes while transcribing the interviews allowed me to have a different perspective of the content that I may not have had without the field notes. They were an important part of the underlying and nonverbal content and reminded me of what I was thinking and feeling at the time.
Triangulation refers to the combination of two or more data sources that when put together, will form the essential data elements of qualitative research [42]. Interview and observation served as two data sources that were used to verify the experiences and perspectives of the women, who shared their experiences of chemo brain with me, and helped me to confirm the meaning of the story. During the interviews, I observed behaviors such as crying, forgetting their train of thought, or showing a lack of focus, while in the midst of telling their stories. One of the women was crying because she forgot to pay a bill on time.
Another women offered me coffee during the interview and asked me if I wanted sugar, but then forgot to bring it to the table when I said yes. She laughed and got up to get it but forgot it a second time. Another participant was 45 minutes late for the interview because she forgot to get gas in her car and could not find my phone number to tell me she would be late. When she did arrive, she came in flustered and spilled her coffee all over the library table. By observing the women when they told their story, the experience of chemo brain came alive with the words, gestures and actions used by the women, thus helping to verify the experience.
Transferability allows the reader to determine if the broad, rich descriptions described by the researcher are meaningful and able to be applied to their own experiences, and it is up to the reader to determine if the experience can be transferred to other situations [42,43]. Transferability refers to how well the descriptions fit to the experiences of others in similar situations. Consequently, the researcher must convey lived experiences in language that fully captures their essence. I focused on writing rich descriptions of the experience of chemo brain, using the women’s own words.
Auditability is another important aspect of trustworthiness in qualitative research.
[42,43] believe that auditability is achieved when another researcher can follow the audit trail used by the investigator from its beginning to its end, follow the progression of events in the study, and has comprehension of the logic by the researcher. Trustworthiness is not a matter of claiming to be right about a phenomenon, but rather, it is a matter of having practiced good science. By making the path followed visible, for example, keeping careful documentation of all research transactions, it is auditable and therefore trustworthy [44]. The path of this qualitative research study has an auditable trail.
Finally the principle of confirmability was upheld. Confirmabilty is achieved when the findings of the study accurately describe the experience as well as the ideas of the participants rather than the subjective or objective stance of the researcher [43]. The goal of this research was to accurately describe the lived experience of chemo brain in breast cancer without interjecting my beliefs about what the experience is. By having the participants confirm all conclusions and clarify ideas during the follow up interview, it ensured that the principle of confirmability was upheld and that the beliefs of the researcher were not implanted. By being aware of the researcher stance and when creditability or truth value, plus auditability, and transferability are established, then confirmability is also achieved [42,43]. Trustworthiness was maintained throughout this research study by using the four domains of rigor, by saturating the data, and by conducting ongoing member checks that clarified and validated what was told about the experience of chemo brain. Additional attention was paid to decentering[34],by being aware of thoughts and feelings about the experience of chemo brain, by really listening and by focusing on what the participants were telling me during each interview.
Researcher stance
Protection of human subjects
During the informed consent process and throughout the study, the principle of respect for persons and autonomy were sustained. Participants were provided with a copy of the consent form and were reminded that their participation was voluntary and that their consent could be withdrawn at any time during the study without consequence. Participants were provided with all the necessary information needed for informed consent including: the aim of the study, privacy/confidentiality procedures, risks/benefits of participating in the study and my contact information for any questions or concerns throughout the study.
Participants in the study were assured that all of the information obtained throughout the study would be kept confidential. All interview tapes and transcripts were secured in a locked filing cabinet when not in use. Informed consents were kept separate from transcripts in a second locked file cabinet. In order for participants to remain anonymous, each was be given a number so that their information would remain confidential throughout the study. All tapes and field notes were kept for a period of at least three years as per the Institutional Review Board (IRB) application at Seton Hall University.
The principle of beneficence guided me throughout the research. Women who agreed to participate in the study gained personal satisfaction by telling their experience of this little known phenomenon. They were listened to and allowed to describe their experience of living with chemo brain. They were also provided with a list of support groups in the event that discussing their personal experiences with chemo brain distressed them in any way. The principle of justice ensures the fair distribution of benefits and costs to potential research participants [45]. (NIH, 1979). Participation in the study was voluntary and all participants were treated equally, fairly, and ethically. Information gained from this research can only add to the limited body of knowledge regarding chemo brain in breast cancer and will benefit women with chemo brain symptoms as a result of chemotherapy for breast cancer in the future.
PARTICIPANT PROFILES
Carol
Carol is a wife and mother of 12 year old fraternal twins and life is busy. She was from Jewish descent. She has an upper middle class background and lived in NYC until she had her twins and then moved to Westchester with her husband and children. She has one brother and her father was still living. She is very close to them. Her father has a history of Alzheimer’s disease for the previous 10 years and she was always looking for ways to improve his memory; techniques that she would later try to improve her own memory. She has a master’s degree in guidance counseling and owned and ran a multinational clothing business for 10 years. She is organized, hardworking, and great at multi-tasking and did not need to rely on others for help prior to receiving chemotherapy for breast cancer.
Carol indicated that prior to receiving chemotherapy, she had a photographic memory and prided herself with never needing to write anything down. In fact, she was able to run her own business of 682 employees without using technology to assist her. She could even remember phone numbers without looking them up. Chemo brain was devastating for Carol. It affected most aspects of her life including being organized, multitasking, remembering details and phone numbers, and getting to places on time. Simple tasks, like grocery shopping, remembering main events, even being on time to commitments became daily struggles and greatly affected her social and emotional well-being. Although Carol needed to rely on her friends, husband and children to assist her with daily routines, she did not give up trying to improve the quality of her life. Carol was interviewed 6 weeks after completing chemotherapy.
Cathy
Cathy is a wife, mother of 2 children, and a teacher. She has a master’s degree in special education and had been teaching for three years prior to her diagnosis. She has 3 sisters and her parents all living close to her. She is of Irish descent. She lives in a middle class neighborhood in a suburban area in Westchester County and was home on maternity leave when she received her diagnosis. She considered herself to be hardworking, organized, charitable, great at multi-tasking and caring prior to chemotherapy.
Before getting a diagnosis of breast cancer and receiving treatment, Cathy was the one that everyone relied on for help. She is the oldest in her family and was used to being there for others. She worked with small children and was able to multi-task. She was able to accomplish multiple things at the same time both in and out of school.
Chemo brain was difficult for Cathy. Not only did she have hormonal fluctuations as a result of recently giving birth, but she also had hormonal fluctuations as a result of chemotherapy and hormonal treatment which further compounded cognitive dysfunction. She felt fatigued and had difficultly remembering to do things. Cathy would walk into a room to get something and forget why she was there. She relied on her husband, mother, sisters, friends and even her little 7 year old daughter Emily to remind her to take care of everyday tasks. She also relied on her vast support system to help with the children, preparing meals and getting her to chemotherapy appointments. Cathy was extremely frustrated by the havoc that chemo brain had on her life. Cathy was interviewed 1 year after completing chemotherapy.
Julie
Julie is the youngest of 3 daughters. She came from an upper middle class Italian background and lived on Staten Island. She is very close to her family and they all live nearby. Julie worked as a medical biller prior to going to nursing school at age 28. Her first nursing job was in a hospital setting before working as a corporate nurse for 5 years. She then moved back to the inpatient setting. She bought a house that needed renovations and was working hard to attain her goals of completing the renovations on her house and becoming a mother. She was organized, goal oriented, and had a great memory before chemotherapy.
After receiving the diagnosis of cancer she said she felt like a “failure” and felt as though her body wasn’t strong enough to fight off cancer. Not only did she have feelings of inadequacy but she also had to deal with the experience of chemo brain.
Chemo brain changed Julie’s life. She had many changes taking place at the same time.
Her in vitro fertilization treatments did not work. She started a new job and was having difficulty keeping up with life’s demands. Julie was overwhelmed. She was always good at remembering tasks and details, names and faces, and staying organized. When she completed chemotherapy she initially thought when asked about chemo brain that she didn’t have it but months after treatment she realized that she did. That was when all the difficulties occurred. She had difficulty with memory and concentration and quickly noticed that she did not feel as sharp as she did before and needed to be assisted by family, friends, coworkers, and technology. Without this assistance Julie said she would not have been able to go along with daily activities. She now had to learn new strategies to help her cope with these cognitive changes without constantly relying on her family. Julie wanted to have a baby and become debt free but the side effects of chemotherapy made it hard for her to achieve her goals. Julie was interviewed 1 year after completing chemotherapy.
Sheila
Sheila is a wife and mother of 2 teenage boys and responsible for the family dog. She is Irish American, middle class and is a special education teacher in the local community. She has a master’s degree in special education. She is very close to her sisters who live within a 30 minute driving distance. Both of her parents are deceased; her mom from breast cancer.
Sheila indicated that before starting chemotherapy, she was organized because she had to be prepared for her students. Between work, home life and family, Sheila was kept busy but she did not have any problems keeping up with her daily activities until the effects of chemotherapy began to take its toll. Because of all the side effects and complications that Sheila was experiencing, she had to miss much of the school year. Her life was put on hold. Sheila did not know what chemo brain was per se, but knew that she was experiencing cognitive decline and was unable to keep up with the demands of her life. She said that lost over a year of her life because she could not be fully present. She had to rely on family, friends, and coworkers to help her cope with everyday life. Sheila was interviewed one year after completing chemotherapy.
Sherry
Sherry was a born in Jamaica and migrated to the United States when she was 10 and her culture and family are very important to her. She loved her life. She was newly married for a year prior to her diagnosis and has 2 teenage stepsons that she adored. She also had a new dog that quickly became part of her family. She has a deeply religious background and trusts God in all matters. She is a nurse for over 20 years who started working as an Oncology nurse administering chemotherapy in the hospital setting then worked with the NCI counseling women with breast cancer and finally earned an advanced degree in psychiatric nursing and she knew about cancer. At the time of diagnosis, she was working in the field of nursing informatics and was very knowledgeable in research and technology. Sherry was very intelligent and considered herself a nerd. She always went the extra mile and provided more information than was required. She was well organized, well-spoken, a great multi-tasker and known for her writing and communication skills. She said:
Ok, I’m a nerd. You know, I’m the one with 3.8 GPA throughout college and schools and it’s been even 4 at times and I gotta get the A you know and the teacher asks you for like a 10 page paper and mine was 25 pages. I’m the girl where when I sat in my college classroom and the teacher would go through the criteria for the paper they’d look at you and say only 10 pages. You know they’d look at you and say like ok Sherry, yes you.
So, I’m the one who would stick a note with my term paper and tell the teacher that the first 10 pages is what you wanted ; the other 10 pages is what I thought you needed, you know (laughing). And I said just go ahead and just grade the first 10, but I just want you to read the other you know. So that’s me, you know.
Sherry was living a dream and then was diagnosed with breast cancer and her world turned upside-down. She experienced many side effects as a result of her chemotherapy including nausea and vomiting, fatigue, hot flashes and worst of all, chemo brain. She had heard about it but did not believe that she would experience it. Sherry was devastated by her experience with chemo brain. Communication skills and writing came naturally to her. She loved to journal but after chemotherapy, she had great difficulty trying to express herself. Her memory was also greatly affected. She could no longer remember things that were important to her like birthdays and anniversaries and even appointments. Chemo brain changed her life. She was a woman in charge, but now had to take a backseat and let family, friends and coworkers assist her. Despite her diagnosis, Sherry believed that her cancer journey was to serve a purpose and she trusted that all would turn out well. Sherry was interviewed five weeks after completing her last chemotherapy treatment.
Tina
After surgery, she completed chemotherapy and began treatment with monoclonal antibodies and hormonal treatment.
Tina is a middle class lesbian woman from the Philippines who lives in NYC since she came to the country almost 20 years ago. At the time of the first interview, Tina was in the process of bringing her fiancé and her children over from the Philippines so that they could marry and she could adopt the 3 teenage children and they could begin their life together. She has no other family in the United States and is anxious for her new family to come. Tina works in business but also went to nursing school to become an LPN. She worked hard and was great at doing what she had to do. She could remember everything she needed to do without writing it down. She was proud that she could do her job so well without relying on technology before she received chemotherapy.
Prior to beginning chemotherapy, Tina was well organized and could multi-task without difficulty. She did not need to rely on others to do her work. She did her job well and enjoyed her life until she started to experience chemo brain. Chemo brain had a major impact on Tina’s life. She started to notice that she had difficulty finding words and remembering things on her to do list; things that she was known to do well. She did not want to admit that she experiencing chemo brain and tried to exercise her mind by remembering rather than using technology. She would use her outlook account as her backup to her memory and found that she often left something out. Her coworkers were very helpful in reminding her to get to appointments and when her family came from the Philippines they too helped to remind her about daily things.
Although she was grateful for the help and support, Tina felt that she lost her independence. Tina wanted her life to return to what it was before and show her new family that she was still independent and able to take care of them. Tina had completed chemotherapy 3 months prior to being interviewed but was still being treated with Pertuzumab and Trastuzumab monoclonal antibody infusions every 3 weeks.
RESEARCH FINDINGS
Based on the analysis of data gathered through individual interviews, five main themes emerged: (1) struggles with day to day life, (2) fatigue, (3) emotions related to diagnosis and treatment, (4) coping with cancer and support during cancer, and (5) feeling grateful for surviving cancer.
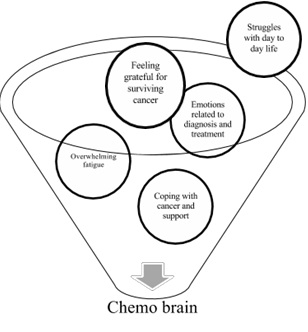 Figure 1: Connection between the emerged themes and chemo brain.
Figure 1: Connection between the emerged themes and chemo brain.In addition, four main sub-themes became apparent in relation to the first main theme about struggles with day to day life. These sub-themes include: (a) memory loss, (b) difficulty with concentration, (c) inability to communicate using writing skills/disorganization of thoughts and words, and (d) difficulty keeping track of and managing time.
Struggles with day to day life
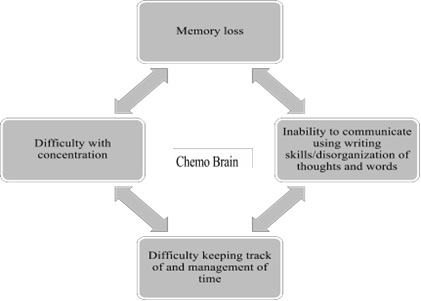 Figure 2: Sub-themes related to struggles with day to day life.
Figure 2: Sub-themes related to struggles with day to day life.Memory loss in most participants was related to the side effects of receiving cytotoxic drugs and hormonal treatment. The challenge of enduring memory loss affected them daily. It had impacted them personally, their family life and their work life because they could not remember to do things that they did without question before cancer and chemotherapy. Most of them got through the day but all of their stress and extra efforts made to compensate for their imposed memory loss often left them feeling confused and tired. Julie reflected: “I can’t think right now. I’m tired. My brain is not functioning a hundred percent.” In addition, Sherry commented, “I don’t by any means have the energy that I did before and it takes me a lot longer to do stuff and that’s been hard.” These examples indicate the extra energy necessary that participants had to expend in relation to memorization.
All participants were disturbed about the way memory loss impacted their lives and the impact it had on how they felt about themselves. Sherry was upset that her memory was failing her. She shared her feelings when she said: “The fact that I couldn’t remember really special things really bothered me”. She commented that she previously remembered sending cards for special occasions like birthdays and retirements and would remember to text a friend to wish her well when she had a job interview, but after chemotherapy she no longer could. This caused her great distress.
Difficulty with concentration: Most participants in this study indicated certain difficulties with concentration. This difficulty was another main area related to cognition and a decline of functionality that most participants agreed affected them and their relationship with others. Participants described having to spend more time and needing to reread materials because they could not grasp ideas the first time. Julie explained “I had a really difficult time just concentrating. I was in school for my Bachelor’s degree so I just stopped going.” Sheila added, “I couldn’t concentrate. I couldn’t remember. I couldn’t read a book.” Most participants also had difficulty reading books and paying attention at work, for example in meetings and conference calls. Sherry explained:
So I had to pull away from it and then come back to it, to say okay, ‘now what is it saying?’ So the concentration is still bad and …it doesn’t come as quickly as before. So I know that and because of it, I have to reread stuff more to just make sure it sounds okay. Before I didn’t really have to put that much effort into it.
Another participant, Carol, felt that she had to work much harder just to keep up with daily demands and could only focus on one thing at a time while in the past, she could easily multitask. Carol said: “I found that also I lack concentration that I used to have. I don’t focus as clearly. She explained, “I have to de-compartmentalize everything. Like that goes there. Your mind is like almost working twice as hard now”. These are just a few illustrations of the effects that chemo brain has on concentration which impacts work life and everyday life. The participants described having to work much harder after having the experience of chemo brain. They had to spend more time completing tasks that they had no trouble completing prior to receiving chemotherapy.
Keeping track of and management of time: Time management was an area of concern for all women in this study. They all related challenges on keeping track of time due to chemo brain. Carol commented:
I cannot make it anywhere on time. I can’t get myself, even knowing, even trying to get myself out the door like say okay when I write the time down on my calendar say it’s at 11 and I write down the appointment, I am still late.
As Carol, Sherry also had similar experiences with time management. She was always the first person on the line waiting for the rest of her team for conference calls until she had chemo brain. She said:
The job was calling and I thought oh, someone from work is trying to check in and they say, “Sherry, are you going to join the call because we started about 10 minutes ago and we didn’t want to call and bother you.
All six participants in this study expressed distress over their lack of ability to complete tasks in a sufficient amount of time. This situation made them feel insufficient, and simple tasks and regular activities took much longer and required greater efforts to complete. In Sheila’s words: “At work I wrote everything I was going to do in because I would get distracted and forget. I would go off on a tangent on something else.”
These feelings were supported by other participants, such as Cathy and Sherry. Sherry explained:
Usually I am in front of 2 computer monitors. I have the domain which is the training part that we are building of the electronic medical record and then on another computer monitor, I have a spread sheet. So, what usually happens in my work, I go from the domain to the spread sheet back and forth, back and forth. So, I am checking what’s in the domain and making sure that it’s in the spread sheet or vice versa. In the spread sheet is the data elements. Because the spread sheets would start to get blurry and confusing and I am like is this line 110 or is it line 120. Because I really had to pay attention to rows and columns and I couldn’t do that. So that’s how I ended up using a lot more medical leave than I originally thought. You know I couldn’t really focus.
Financial demands were an example of a stressful area that was indicated by several of the participants. Sherry got behind on paying her bills because she no longer managed time demands well and could no longer keep track of when bills were due. She explained:
I got behind on bills so I ended up during chemo paying a lot of late fees because I just wasn’t as organized so the whole concept of chemo brain interferes with your ability to really organize your life not just the medical part but your home life you know um your financial life has to do with you pay your bills on time.
Sherry became very emotional about this issue and cried about this during the interview. She was always able to keep track of things and keep up with home and work demands until she had the experience of chemo brain and could no longer remember appointments or pay bills on time. Like Sherry, Sheila also complained about her lack of memory and organizational skills caused by chemotherapy. She would forget things like paying bills on time and booking appointments on a daily basis, she said:
I’ll say to myself, Oh, I really need to book that doctor's appointment, and then 5 hours will go by, and then I'll say, Oh my God. I never booked that doctor's appointment.
Things just completely slip your mind, but I don't know if that's part of getting older or if it's from the chemo.
Overall, participants in this study felt that keeping track of time and time management was difficult as a result of experiencing chemo brain and commented on this many times throughout the interview. This inability to focus on particular tasks and plan ahead made most participants feel unable to perform in their jobs and daily activities as they did prior to chemotherapy.
Inability to communicate using writing skills/disorganization of thoughts and words: Research findings in this study indicate that cognitive skills, such as writing and the organization of thoughts and words were compromised. Sherry explained:
I knew what I wanted to write. I wanted to write about what I was going through that day and some of the conversations I was having with God. I couldn’t get the words together you know. And that was really hard because I don’t usually have a problem with words. So, focus and word construction and sentence construction- I just couldn’t put it together you know, and it was frustrating.
To this, Tina added: “One thing I also noticed about the chemo is words. Words that escape me. Even simple words.” Difficulty finding words to describe something was evident throughout the interviews, for example when Tina wanted to borrow my pen but could not remember what it was called. She asked for “the thing you write with” instead. Sherry and Tina both found that this had an effect on the ability to do their jobs. This was difficult for both Sherry and Tina as it was for all of the participants of this study. These women were all hard working individuals whose jobs required attention to detail as well as impeccable verbal and written communication skills.
To summarize, research findings in this study indicate that all six participants were affected by the experience of chemo brain and this took a toll on their ability to fully participate in all aspects of their lives. The six participating women in this study were unable to maintain their usual daily activities while having the experience of chemo brain that began shortly after starting chemotherapy and continued through the interview process. All of them explained that it took them longer to do their routine activities and errands, such as housework and laundry, as well as going to the grocery store after receiving chemotherapy. They found the need to pace themselves and take breaks while doing them because of the debility they felt both mentally and physically.
Chemo brain had devastating effects on the lives of the women in this study. Minor tasks became something that had to be planned for in advance with reinforcement. They could no longer take things for granted. Carol, as all participants, was frustrated by her lack of organization. She described her trips to the grocery store as a clear example of how disorganized she felt and described herself as having a scattered mind. She explained:
The grocery store is all of eight minutes from my house, so even if it is a bad day, the whole thing should have taken me a half hour. Two and a half hours it took me. … Because I left my house five times because I forgot my wallet, my bag, my keys, and then finally the list.
Thus, chemo brain prevented participants from working to full capacity and participating in usual family activities. The women in the study experienced cognitive dysfunction that had a profound impact on essential aspects of their lives. They dealt with daily disruptions of even the simplest activity that most people would take for granted.
Overwhelming fatigue
Tina was athletic and an avid volleyball player prior to starting chemotherapy, but after starting treatment she said that she gained weight and lost energy and was not able to play while on treatment. Julie stopped going to school while on chemotherapy because she did not have the energy to get her work done and Sheila was unable to work at all because of the effects of chemotherapy that included fatigue. Thus, fatigue had a major impact on life during and after chemotherapy.
Emotions related to diagnosis and treatment
A range of feelings and emotions were expressed by all six participants from the time of diagnosis through survivorship. Some of the main feelings expressed included being afraid, nervous, depressed, indecisive, anxious, frustrated, and stressed. Women in this study wanted to talk about their experiences and share them with others in order to help themselves cope with the experience of having cancer, as well as to help others understand what this experience meant to them. Similar opinions regarding the emotional aspects of chemo brain were expressed by Cathy, Carol, and Sheila. For example, Cathy was filled with emotion about her experience before and after getting diagnosed and starting treatment, and she explained:
I would get myself so worked up and convince myself that something is wrong and have to tell myself that everything will be fine. …Especially with no family history. It was just so sudden, you were so young…there were so many scenarios here. …And once it happens to you it is always in the back of your mind. Is it going to happen again?
Because you know you never expected it to happen so it’s always in the back of your mind.
In her own words, Cathy was trying to voice her concern for the future, and was very adept in expressing herself. Like Cathy, most participants worried about their future, as well as the treatment itself, but despite the fear of the unknown, the majority of the women also felt thankful that the cancer was found and that they were being treated and would be cured. They were also thankful to have the wonderful support systems that helped to get them through treatment, such as family, friends, and coworkers. Regarding her coworkers, Tina said: “They help me a lot.
They make sure I get to my appointments on time. "Oh Tina, it's 02:00, you have an appointment at 03:00; you've got to go." To this, Julie added: “My husband was super supportive. Really was. I would say my other family members were but my husband was a dream, was an angel.” Sherry, for example found it difficult to give up control, but realized how important it was to her journey that she relinquish some of her responsibilities. She explained: I also had my husband more involved in helping me remember stuff you know cuz he would go with me to a lot of appointments um, but the times I was well, I would go to the appointments by myself. So I needed…I think it’s important to let your loved one know kinda what you’re going through, that you are having trouble and ask for help. And for me, I think a part of this journey was that too. That was not easy for me.
In regards to the diagnosis and prognosis, all participants accepted their diagnosis and believed that they were cured and despite having a cancer diagnosis and knowing that the cancer could return, each one found a positive outcome from having gone through the experience. This helped them to set priorities in life and understand how fragile life can be. Although Cathy had a difficult time with side effects, she felt a sense of security while on chemotherapy and became nervous when she completed chemotherapy. She reflected:
It was interesting um during chemo I would see Dr. D every two weeks…you know when somebody is watching you, monitoring you and then when I stopped seeing her… I would go to her every four months, then every six months it made me so nervous because I am not being monitored the way I was you know what I mean? …What’s happening over those six months that I am not having bloods drawn…it was just so….I mean I think it will always be at the back of my mind, you know to have that thought of oh what if it comes back. I know I will never not feel that way, but I mean at the beginning it was there. You know when you finish your treatment it’s like you have to get back to a normal life. You were so used to going to the doctor and having her check me…
Cathy was able to articulate both negative as well as positive experiences about her cancer journey. Despite the difficulties, participants connected with their emotions in the past as well as the present. They were fearful and angry about their diagnosis and concerned for their future, but eventually came to believe that they would be cured of cancer. They were able to describe a transformation in their worldview due to their experience with cancer. Still, some of the participants expressed anger about having the experience of chemo brain during the cancer experience. Julie indicated manifestations of denial and fear when she first began to experience cognitive changes and explained that she did not want to admit that she was having the experience of chemo brain even though she knew in her heart that it was chemo brain. She was already dealing with so much in her own life that the chemo brain was more than she could deal with. She reflected, “I was in denial that that would be anything. I realize now that I think I definitely had chemo brain”. She said that she knew that she was experiencing chemo brain right away but was angry about it. Thus, the cancer/chemotherapy experience triggered a variety of emotions from denial to acceptance, often happening concurrently, in the women in this study.
Coping and support during cancer
All participants found effective ways to compensate for their chemo brain. They used technology, as well as more conventional ways, including writing notes and setting alarms to help them navigate through their daily routines, responsibilities, and unanticipated events. All of them mentioned the use of smartphones with alarms and reminders, calendars, sticky notes, and lists as effective ways to aid them with daily life activities. Julie explained: “I make lists and carry them in my pocket so I can add to them.” Also, Sheila said: “I write everything down so I don’t go off on a tangent.”
Each participating woman used a combination of techniques to cope with the cognitive deficits they were experiencing. As Sherry described: “my phone has an alarm thing in it and it can alarm not just on time but events. So if I put an event in my phone; it’s a smart phone. So my phone alerts me.” All of them questioned how they would have coped if they had had the experience of chemo brain before technology existed. Carol commented: “I put all of the phone numbers in the phone now, but I used to remember them all before chemo brain.”
Use of technology was an important coping resource for all six participants. Julie and Cathy used their smartphones as part of their daily routines to remember important information like appointments and taking their medications. Julie said, “I keep notes; I keep my cell phone, a lot of reminders in my cell phone. I set the alarm clock so I know that it’s going to happen.” While Cathy used the alarm to remember to take her Tamoxifen saying, “so I’d set my alarm every day at the same time”. Sherry too used her smartphone to remind herself to do important tasks. She explained: “yeah, I got a new phone that’s helpful because I use a daily task reminder and it alerts me with different tasks.” She found this to be very helpful to keep her on track.
Despite having an abundance of computer assisted technologies available to aid with cognitive decline, some participants chose to use written notes and to exercise the brain to prevent further decline, as well as to continue their effort to function as well as they did before the chemotherapy. For example, Sheila explained:
At work I wrote a lot of post-it notes, even everything I was going to do that day teaching in class because I would just get distracted and forget. I would just go off on a tangent on something else.
Tina tried to make mental notes, but she also used her outlook calendar as a backup. She wanted to maintain as much of her brain power as possible without relying on technological support, and believed that using her brain would help to strengthen her memory, but used her Outlook calendar as a backup to assure that she had not forgotten anything. Tina commented:
I'll make a mental note of it. And the first thing I do when I come in the morning is just see what it is, how much I remember. Instead of me making a note, I just look on my email, on Outlook. I just mark everything that I didn't get to process in red.
Compensating for chemo brain was important to all women who participated in this study. They wanted to continue on with normal life and the responsibilities associated with it asthey did prior to chemotherapy and were willing to use any means possible whether post it notes, smartphones, or the help of others in order to function.
In relation to feeling supported during the cancer experience, all participating women expressed their gratitude towards family, friends, and sometimes co-workers for their support and understanding throughout their cancer diagnosis and treatment. They thought that they would not have made it through the experience of cancer, chemotherapy, and chemo brain without a strong support system. Julie explained that her husband and family were really there for her throughout treatment, and commented: “yeah, my husband was super supportive. Really was. I would say my other family members were, but my husband was a dream, was an angel.” Sherry also had a strong network available to support her in the process and indicated: “you have resources and you like use them, especially a support network. You know, let people know on the days I’m not having a good day.” In regards to family support during cancer treatment, Cathy too expressed thankfulness of her family and friends and even had the assistance of her young daughter, saying “sometimes even Emily (young daughter) helps remind me of things”. She also relied on her sister for activities of daily living. She explained: “I couldn’t even, like literally, my sister was like feeding me”. Her sister and her husband were also present for chemotherapy appointments which Cathy really appreciated. She said:” We made like a day of it though, like my sister Cookie would come with me and my husband for chemo day”. Thus, research findings in this study indicate that family support played a significant role in helping participants cope with their cancer experience both emotionally and to aid with everyday activities like taking them to appointments, preparing meals and reminding them to take medication. Cancer patients are in a vulnerable situation and having the support of family was crucial to the recovery of the six participants.
Just as family support was important to the recovery of the women in this study, so was the support of friends and colleagues. All of the women agreed that their friends and coworkers were instrumental in helping them cope with their poor memory. They reminded them of appointments and meetings and supported them throughout the chemotherapy. Sheila, for example, relied on the teachers at work for help and support stating: “I have tons of friends at work”. Tina had her coworkers reminding her to leave to go to her chemotherapy appointment.
All participants considered their friends and coworkers to be a part of their extended family outside of the home. Support outside of the home, particularly in the work environment was so important to the participants of this study. These support systems made such an important impact and helped them to maintain some normalcy while going through a stressful period in their lives.
Feeling grateful
In the grand scheme of things, I’m here, I’m healthy, I’m well, I’m blessed, I’m healed. So in the grand scheme of things, it really isn’t like the end of the life. You’re gonna get over it; get through it, you know. So that’s probably the messages that in the grand scheme of things focus on getting well, focus on being fully available to your family, your friends, your life and then the details and stuff will come, you know.
Because these women felt so grateful about their experience, many of them also expressed learning not to take anything for granted and wanted to give back to others who were newly diagnosed and just beginning the cancer journey. Sherry, for example, made it a goal to spread the word about the importance of self-breast exam, clinical breast exams and getting yearly mammograms. Some of the women she spoke to also ended up with a diagnosis of early breast cancer because she encouraged them to have a mammogram. Another participant, Cathy, helped to raise awareness of breast cancer by participating in a breast cancer fashion show.
Carol joined the breast cancer walks to celebrate her cure and to raise consciousness about breast cancer. Julie shared her experience and offered encouragement and support to the patients she worked with at the cancer center. Tina encouraged her coworkers to have yearly mammograms and to do monthly self-breast exams, and Sheila became a constant support for her sister who was newly diagnosed with breast cancer. She commented: “she was there for me and now I want to help her get through it too.”
Regarding putting things in proper perspective, Sherry was able to prioritize aspects in life through her cancer and treatment journey and felt that she came out a changed person because of it. She explained learning what was important to her and made time for the things that mattered just as the other participants had. In relation to prioritizing aspects in life, Cathy believed that it was critical to help other women that were having difficulty facing breast cancer because she had experienced and survived breast cancer at a young age. She was grateful that she could be there for them, and said: “I try to help women that have been diagnosed…I just spoke to a woman that was just diagnosed and after speaking to her she said she felt better”.
Giving back because they felt grateful was important to each of the six participating women in this study and was evident in their comments, reactions, and actions.
DISCUSSION, IMPLICATIONS AND RECOMMENDATIONS
The intention of this study was to describe the lived experience of women 50 and under who experienced chemo brain while completing chemotherapy or within 6 months prior to participation. Six women chose to participate in this phenomenological study and were asked to describe their lived experience of chemo brain. Interview sessions were recorded and data was analyzed, and five main themes emerged, (1) struggles with day to day life, (2) fatigue (3) emotions related to diagnosis and treatment, (4) coping and support, and (5) feeling grateful.
Within the theme of struggles with day to day life, four sub-themes were identified: (1) memory loss, (2) difficulty with concentration, (3) inability to communicate using writing skills/disorganization of thoughts and words, and (4) keeping track of and management of time. These four sub-themes were related to daily struggles. Participants also described effective resources and coping mechanisms that helped with the struggles day to day that they experienced. The women described their support system through cancer treatment, which in most cases, included family, friends, and co-workers.
Discussion
Furthermore, despite the inability to recognize who will get chemo brain or trying to find out how to prevent it, studies have verified that chemo brain is a real phenomenon [14,28] and needs to be addressed by oncology healthcare providers in order to fully treat those affected by it[33].discussed the importance of acknowledging the existence of chemo brain to breast cancer survivors who often felt humiliated in social situations because they could not remember important details explaining that although it was difficult to mitigate symptoms of chemo brain, it was important to validate the manifestations of it [33]. In this study, research findings corroborate the [33] study as it was found that as in other studies, participants were not told about chemo brain. They heard about it from friends, coworkers or read articles about it. They expressed a desire to have heard about the commonly occurring symptoms of chemo brain from their oncology healthcare provider prior to having it happen to them. They stated that they would have been better able to deal with the consequences of chemotherapy as it related to cognitive decline if they were prepared for it.
The literature supports descriptions of chemo brain as well as symptoms of cognitive dysfunction. The studies of [2,5] substantiate the existence of cognitive dysfunction as a result of chemotherapy in breast cancer. Symptoms associated with chemo brain include: complaints of short term memory loss, difficulty concentrating, struggling to make simple decisions, difficulty finding the right words, trouble multi-tasking and feelings of mental dullness [2,14,28].Findings in this study support these previous results. In relation to difficulty finding the right words, this study found that participants often had difficulty finding words and had to describe a situation to someone in order to help them find the right word. Regarding struggling to make simple decisions, participants in this study mentioned that even simple decisions like whether to have rice or mashed potatoes for dinner was a difficult decision at times. Thus, it is inferred from the amount of information gathered in this investigation that chemo brain is a phenomenon that has considerable impact on the lives of women with early stage breast cancer who have received chemotherapy.
Literature describes some of the disruptions of life caused by chemo brain such as how cancer and cancer treatment affected participants’ ability to work, as well as returning to work after chemotherapy[21].Reported a decrease in overall work productivity and feelings of disappointment for not being able to perform as before cancer treatment in their companies. Similarly, [22] found that all 13 breast cancer survivors reported cognitive deficiencies affecting work performance and their ability to return to work. [23,33] found similar results in that participants were reluctant to return to work because of the cognitive problems they faced.
Findings in these studies support the idea that returning to work after experiencing chemo brain is difficult. Participants expressed feelings of inadequacy and were reluctant to return to work due to the fear of not being able to perform to the company’s standards. Participants also agreed on the importance of returning to a normal life after treatment, but found it difficult to do. The findings of this study are consistent with these studies on 2 major points. Women who have experienced chemo brain struggle emotionally between their desire to return to normalcy in work and a fear of how they will perform on returning to work.
Regarding social aspects and support from others, studies of cancer patients indicate the importance of a support system in which patients could temporarily relinquish responsibilities and allow family and friends to take over until they are able [14,28]. There are however few qualitative studies on socioemotional aspects and coping or emotional compensation of patients due to chemo brain. In this respect, this research study contributes to the limited literature on both cognitive and socioemotional aspects affecting women with cancer and chemo brain. The findings of this study emphasize the need to provide important information on the type of support and specific needs of the participants, which included emotional as well as physical support. Women with cognitive dysfunction as a result of chemotherapy need guidance about what to expect and how to cope with chemo brain. Main themes and subthemes that emerged from this study support previous literature on participants needing guidance which leads to improvement of quality of life. The women in this study offered great examples of all the little ways they coped with chemo brain, which can be shared with other women with the same experience. The excellent strategies used by the women in this study can be offered as a guideline for other women with breast cancer who experience chemo brain. This information is not in the literature and is an important contribution of this study.
Although chemo brain has been reported as neurocognitive changes and cognitive impairment [14,28], the women in this study reported it as more than a change in brain function and therefore cannot be separated from the complete illness experience. These women reported anxiety, fear and overwhelming fatigue along with cognitive decline. When telling their stories, the 6 women included these aspects as part of their experience. One of the women in the study said that she was too tired to take her medication after setting an alarm to remind her to take it.
Limitations
The participants in this study included only women since women are more likely to get breast cancer; however, men can also experience breast cancer and have experienced chemo brain. How would their experience be similar or different? Thus, men should be considered in future studies on cognitive impairment as a result of chemotherapy.
Implications for Nursing
In this study, participants wished that healthcare providers had provided more recognition and understanding of cognitive dysfunction as a result of cancer treatment. Therefore, the counseling and education of women about the side effect of chemo brain should begin during the initial teaching session and should be assessed for throughout each chemotherapy cycle and follow up visit (Table 2).
|
1. Memory loss |
|
2. Difficulty with concentration |
|
3. Inability to communicate using writing skills/disorganization of thoughts & words |
|
4. Difficulty keeping track of and managing of time |
|
1. Post it (sticky) notes |
|
2. Smart phone reminders (calendars, alarms, apps) |
|
3. Support from family & friends |
|
4. Outlook calendars/email |
|
5. Written notes in plain sight (refrigerator, bathroom mirror) |
|
1. Chemo brain exists. It is a real phenomenon. |
|
2. Cognitive effects of chemotherapy and how will it change my daily life. |
|
3. What can I do for it? |
|
4. How long will it last? |
Table 4: What women wanted to know about chemo brain before beginning chemotherapy.
Recommendations for future research
Final thoughts
Although the goal of this research was to describe the lived experience of chemo brain in early stage breast cancer, the rich descriptions of the symptoms of chemo brain shared by the participating women can help to improve the identification of chemo brain in breast cancer. It is beneficial to identify cognitive impairment as a result of chemotherapy treatment earlier rather than later, and although evidence-based interventions remain limited, without proper assessment, interventions that could alleviate symptoms cannot be tried or provided. This has the potential to improve the quality of life for women with chemo brain.
ACKNOWLEDGEMENT
I would like to take this opportunity to thank the six women who agreed to participate in this study. I am so grateful to them for being so candid about their experiences with chemo brain. Because I gave them a forum to speak about their experiences, I was able to gain a deeper understanding of what chemo brain meant to them. I will be forever thankful for their bravery and willingness to share their time and veracity with me.
I would also like to acknowledge the local ONS chapters who allowed me to speak at their monthly meetings in hopes of gaining participants. Although I was not able to obtain any participants, I am still grateful for the opportunity. I was able to secure participants through colleagues and friends who helped to spread the word about my research. Without their help I would still be looking for participants.
I would be remiss if I did not mention my coworkers as well as two people who also helped to make this dissertation possible. Both Valentina Kloosterman and Julie Schantz provided me with support to make this happen. Valentina helped to keep me on track when I did not know how to proceed while Julie lit a fire under me during the final process. Both kept me from losing steam and I will be forever grateful.
I am so grateful to my committee members, Dr. Bonnie Sturm and Dr. Munira Wells and especially to my chairperson, Dr. Judith Lothian who was always so supportive and caring. She helped me to believe that I could achieve my goals when I was struggling along. She gave me strength and motivation when I needed it most and I am so thankful to have had her as my advisor and mentor.
REFERENCES
- vanManen M (1990) Researching lived experiences. Ontario, Canada: Althouse Press.
- Staat K, Segatore M (2005) The phenomenon of chemo brain. Clin J OncolNurs 9: 713-721.
- Pullens MJ, De Vries J, Roukema JA (2010) Subjective cognitive dysfunction in breast cancer patients: A systematic review. Psychooncology 19: 1127-1138.
- Hess LM, Insel KC (2007) Chemotherapy-related change in cognitive function: A conceptual model. OncolNurs Forum 34: 981-994.
- Jenkins V, Shilling V, Deutsch G, Bloomfield D, Morris R, et al. (2006) A 3-year prospective study of the effects of adjuvant. Br J Cancer 94: 828-834.
- Harvard Health Publications (2002) Cognitive problems after chemotherapy for breast cancer. Harvard Women's Health Watch 10: 5-6.
- Paraska K, Bender C (2003) Cognitive dysfunction following adjuvant chemotherapy for breast cancer: Two case studies. OncolNurs Forum 30: 473-478.
- http://http://www.ons.org/research/information/documents/pdfs/agenda05.pdf
- U. S. Department of Health and Human Services (2017) Healthy people 2020: What are the goals.
- Frank JS, Vance DE, Jukkala A, Meneses KM (2014) Attention and memory deficits in breast cancer survivors: Implications for nursing practice and research. J NeurosciNurs 46: 274-284.
- Grober S (2002) Resources for treatment of chemotherapy-related cognitive difficulty. Cancer Pract 10: 216-218.
- van Dam FS, Schagen SB, Muller MJ, Boogerd W, vd Wall E, et al. (1998) Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: High-dose versus standard-dose chemotherapy. J Natl Cancer Inst 90: 210-218.
- Giorgi A (1985) Phenomenology and psychological research. Pittsburgh, PA: Duquesne University.
- Thielen J (2008) The experience of neurocognitive changes in women undergoing chemotherapy for breast cancer (Doctoral dissertation).
- Rust C, Davis C (2013) Chemobrain in underserved African American breast cancer survivors: A qualitative study. Clin J OncolNurs 17: 29-34.
- http://memory.ucsf.edu/Education/Topics/normalaging.html
- American Cancer Society (2015) All about breast cancer.
- Meyers C (2013) Cognitive complaints after breast cancer treatments: Patient report and objective evidence. J Natl Cancer Inst 105: 761-762.
- Olin J (2001) Cognitive function after systemic therapy for breast cancer. Oncology15: 613- 618.
- Dowling M (2007) From Husserl to van Manen. A review of different phenomenological approaches. Int J Nurs Stud 44: 131-142.
- Kennedy F, Haslam C, Munir F, Pryce J (2007) Returning to work following cancer: A qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl)16: 17-25.
- Munir F, Burrows J, Yarker J, Kalawsky K, Bains M (2010) Women’s perceptions of chemotherapy-induced side affects on work ability: A focus group study. J ClinNurs 19: 1362-1370.
- Hede K (2008) Chemobrain is real but may need new name. J Natl Cancer Inst 100: 162-169.
- Inagaki M, Yoshikawa E, Matsuoka Y, Sugawara Y, Nakano T, et al. (2007) Smaller regional volumes of brain gray and white matter demonstrated in breast cancer survivors exposed to adjuvant chemotherapy. Cancer 109: 146-156.
- Jansen C, Miaskowski C, Dodd M, Dowling G, Kramer J (2005) Potential mechanisms for chemotherapy-induced impairments in cognitive function. OncolNurs Forum 32: 1151-1163.
- Silberfarb PM, Philibert D, Levine PM (1980) Psychosocial aspects of neoplastic disease: II. Affective and cognitive effects of chemotherapy in cancer patients. Am J Psychiatry 137: 597-601.
- Weineke MH, Dienst ER (1995) Neuropsychological assessment of cognitive functioning following chemotherapy for breast cancer. Psycho-Oncology 4: 61-66.
- Mulrooney T (2007) The lived experience of cognitive impairment in women treated with chemotherapy for breast cancer (Doctoral dissertation).
- Brezden CB, Phillips KA, Abdolell M, Bunston T, Tannock IF (2000) Cognitive function in breast cancer patients receiving adjuvant chemotherapy. J ClinOncol 18: 695-701.
- Janelsins MC, Heckler CE, Peppone LJ, Kamen C, Mustian KM, et al. (2017) Cognitive complaints in survivors of breast cancer after chemotherapy compared with age-matched controls: An analysis from a nationwide, multicenter, prospective longitudinal study. J ClinOncol 35: 506-514.
- Von Ah D, Jansen CE, Allen DH (2014) Evidence-based interventions for cancer-related and treatment-related cognitive impairment. Clin J OncolNurs 18: 17-25.
- Von Ah D, Habermann B, Carpenter JS, Schneider BL (2013) Impact of perceived cognitive impairment in breast cancer survivors. Eur J OncolNurs 17: 236-241.
- Von Ah D (2015) Cognitive changes associated with cancer and cancer treatment: State of the science. Clin J OncolNurs 19: 1-10.
- Munhall P (2007) Nursing research: A qualitative perspective (4th ed.). Boston, MA: Jones and Bartlett.
- Heidegger M (1962) Being and time. San Francisco, CA: Harper and Row.
- Higginbottom G (2004) Sampling issues is qualitative research. Nurse Res 12: 7-19.
- Husserl E (1965) Phenomenology and the crisis of philosophy. Philadelphia, PA: Harper and Row.
- Merlau-Ponty M (1962) Phenomenology perception. London,UK
- vanManen M (2002) Writing in the dark: Phenomenological studies in interpretive inquiry. London, UK: Althouse Press.
- Crist JD, Tanner CA (2003) Interpretation/analysis methods in hermeneutic. Nurs Res 52: 202-205.
- vanManen M (1997) Researching lived experience: Human science for an action sensitive pedagogy (2nd Ed.). Ontario, Canada: Althouse Press.
- Jansen CE, Miaskowski CA, Dodd MJ, Dowling GA (2007) A meta-analysis of the sensitivity of various neuropsychological tests used to detect chemotherapy. OncolNurs Forum 34: 997-1005.
- Lincoln Y, Guba E (1985) Naturalistic Inquiry. Newbury Park, CA: Sage.
- Sandelowski M (1986) The problem of rigor in qualitative research. ANS AdvNursSci 8: 27-32.
- Sandelowski M (1993) Rigor or rigor mortis: The problem of rigor in qualitative research. ANS AdvNursSci 16: 1-8.
- National Institutes of Health (1979)Thebelmont report. Ethical principles for the protection of human.
- Bender C, Merriman J (2014) Cancer and treatment-related cognitive changes: What can we do now? What lies ahead? Oncology 28: 201379.
Citation: Gibbons PA (2019) The Lived Experience of Chemo Brain in Early Stage Breast Cancer in Women 50 and Under. J AlzheimersNeurodegenerDis 5: 020.
Copyright: © 2019 Patricia A Gibbons, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

