
Trabeculectomy vs. Express P-200 Shunt Surgery in Post Cataract Patients
*Corresponding Author(s):
Ofri RimoniDepartment Of Ophthalmology, Kaplan Medical Center, Rehovot, Pasternak St., Israel
Tel:+972 545858401,
Fax:+972 39540770
Email:ofririmoni@gmail.com
Abstract
Purpose: The aim of this paper is to explore the clinical outcomes of pseudophakic eyes undergoing the Ex-PRESS shunt P-200 implantation compared to trabeculectomy.
Methods: A retrospective analysis of the records of 44 eyes of 35 pseudophakic patients who had undergone trabeculectomy or Ex-PRESS shunt implantation was conducted. This included records of other information such as demographics, type of glaucoma, surgical details, preoperative and postoperative data including: Intraocular Pressure (IOP), number of medications, the need for additional surgery, and any relevant complications.
Results: Thirteen (30%) eyes underwent trabeculectomy and 31 (70%) underwent Ex-PRESS shunt implantation. No significant difference in IOP reduction or the number of postoperative IOP-lowering medications was found. Success rates were 92.3% for trabeculectomy and 88.9% for Ex-PRESS shunt. Complications rate was almost twice as high after trabeculectomy (46.2% vs. 19.3%), though this was not statistically significant (p=0.135).
Conclusion: There was no difference found in the efficacy of trabeculectomy when compared with Ex-PRESS shunt in pseudophakic eyes. Ex-PRESS shunt was generally found to be a safer procedure, though this difference didn’t reach statistical significance.
Keywords
Trabeculectomy; Ex-PRESS shunt; Glaucoma; pseudophakia
Introduction
Trabeculectomy is still considered the gold standard procedure, for the reduction of intraocular pressure in glaucoma patients [1]. However, it is usually thought to be less successful in pseudophakic patients [2], possibly due to alterations in the nature of aqueous humor, resulting in augmented failure rates of trabeculectomy [3]. Other mechanisms have been proposed for this higher failure rate including conjunctival scarring after superior sclerocorneal incisions for extra capsular surgery or phacoemulsification [4]. The Ex-PRESS shunt (Alcon, Forth Worth, Texas, USA) was invented as a modification for trabeculectomy with the theoretical advantage of a shorter learning curve, reduced disruption of the ocular tissues, faster visual recovery, and more predictable results [5-9].
Most trials comparing the efficacy of both procedures, showed equivalent efficacy in heterogeneous groups consisting of phakic and pseudophakic patients [6,7,10-15]. Several meta-analyses comparing Ex-PRESS surgery to standard trabeculectomy showed that the Ex-PRESS surgery is more likely to achieve complete success, with fewer postoperative interventions and possibly a lower frequency of complications such as hypotony [4,16,17].
None of the studies addressed specifically pseudophakic patients, who comprise a significant proportion of the population suffering from glaucoma.
The purpose of this study is to evaluate the efficacy of the Ex-PRESS shunt compared to trabeculectomy in a group of pseudophakic patients.
Materials and Methods
All research was conducted in accordance with the Declaration of Helsinki and with approvals by the Institutional Review Board of Kaplan Medical Center. Records of pseudophakic patients from 2010 to 2019 who had undergone Ex-PRESS shunt implantation or trabeculectomy were collected. Patients under the age of 18 and those with a less than 3 months of follow up after the surgery were excluded. Eyes with previous ocular trauma or other surgeries besides cataract extraction and laser trabeculoplasty, were also excluded from the study.
Data was extracted from surgical notes, reports, and both in-patient and outpatient charts. Parameters included demographics, glaucoma type, previous treatments, number of antiglaucoma medications, any post-operation complications, and any other post-surgical interventions that were necessary during the follow-up period. IOP measurements were obtained by Goldmann applanation tonometry preoperatively, and postoperatively at 6 and 12 months, together with the number of pressure-lowering medications. Combination medications, such as Cosopt (Dorzolamide hydrochloride and Timolol maleate) were counted as 2 separate medications.
Complete success was defined by a 20% reduction in IOP from the preoperative value and IOP being less than 18 mmHg under no medications. Qualified success was set when additional medications were needed. A repeat glaucoma surgery, persistent IOP less than 5 mmHg, or over 20mmHg despite medical therapy, were the criteria for failure. Needling was not considered as a failure.
A thorough review to verify that surgical techniques were documented utilizing a single method to ensure uniformity of the study was done. The availability of the Ex-PRESS shunt, which was only sporadically available throughout the period, was influential in the decision of which procedure to execute. Aside from this consideration, there was no other bias in the selection of procedures. All patients’ records were kept private and anonymous.
Surgical techniques
All surgeries were performed by 1 of the 2 glaucoma surgeons (Z.M, K.R). Surgical technique for both procedures included creating a fornix-based peritomy, dissection of a scleral flap, followed by subconjunctival application of mitomycin C (MMC) 0.2 mg/mL for 2 to 3 minutes, and thorough irrigation. In trabeculectomy, the anterior chamber was then entered using a1 mm stylet, and a peripheral punch was performed, followed by peripheral iridectomy. In Ex-PRESS, the anterior chamber was entered using a 25 G needle, followed by the insertion of P-200 Ex-PRESS shunt using the designated applicator. The scleral flap was then sutured in both procedures by two 10-0 nylon sutures, and closure of the conjunctiva was conceived by suturing it to the limbus using multiple 10-0 nylon sutures as needed. Postoperative regimen included treatment with topical ofloxacin 0.3% 6 times a day and dexamethasone sulfate 0.1% 4 times a day with a slow tapering over 3 months, with cessation of all previous topical IOP-lowering medications.
Statistical analysis
Data presents as means ± standard deviations or percentages. Continuous variables between the various study groups were tested for normality by Shapiro-Wilk test and when abnormal distribution was found, non-parametric tests were performed. The Mann-Whitney test was performed to compare between the two groups- Trabeculectomy and Ex-PRESS. The t test was used to compare variables with normal distribution. In order to understand the correlation between two categorical variables, Chi square test was used. A P-value of 0.05 was used to declare statistically significant difference between the groups for all analyses. Data were analyzed using SPSS for windows version 25.
Results
44 eyes of 35 patients fulfilled the inclusion criteria and were included in the study. The demographic and ocular characteristics of the study patients are listed in table 1. In total, 13 eyes underwent trabeculectomy, and 31 underwent Ex-PRESS shunt implantation. The baseline demographic and clinical characteristics were similar in the two groups. Mean follow up time was 3.3±3.6 years. Twenty-three (74%) and 12 eyes (92%) had a minimum 1 year follow up in the Ex-PRESS vs. Trabeculectomy group, respectively. Five (11.4%) eyes previously undergone argon laser trabeculoplasty, 2 from trabeculectomy group and 3 from the Ex-PRESS group. One (2.2%) eye from the trabeculectomy group had undergone selective laser trabeculoplasty.
|
|
Trabeculectomy (N=13) |
Ex-PRESS (N=31) |
P |
|
Age |
78.8 |
75.4 |
0.389 |
|
Male Sex |
8 (61.5%) |
24 (77.4%) |
0.295 |
|
Mean preoperative IOP (mmHg) |
22.15 |
21.55 |
0.642 |
|
Mean preoperative no. IOP-lowering medications |
4.09 |
4.42 |
0.135 |
|
Previous laser treatment forglaucoma |
3 |
3 |
0.339 |
Table 1: Patients demographics and characteristics.
Glaucoma diagnosis was classified into Primary Open-Angle Glaucoma (POAG) 26 (59.1%), Pseudoexfoliative Glaucoma (PEXG) 9 (20.5%) and others including uveitic glaucoma, Chronic Angle-Closure Glaucoma (CACG) and Neovascular Glaucoma (NVG) 9 (20.5%), which were grouped together in a separate group due to the relatively low proportion of patients. Most patients undergoing Ex-PRESS belonged to the first group (71%), while the majority of the patients who underwent trabeculectomy belonged to the third group (38.5%). The distribution of glaucoma types between the two groups is provided in table 2.
|
Glaucoma type |
Total (N=44) |
Trabeculetomy (N=13) |
Ex-PRESS (N=31) |
|
POAG |
26 (59.1%) |
4 (30.8%) |
22 (71%) |
|
PEXG |
9 (20.5%) |
4 (30.8%) |
5 (16.1%) |
|
Complex |
9 (20.5%) |
5 (38.5%) |
4 (12.9%) |
|
Primary open angle glaucoma (POAG), Pseudoexfoliation glaucoma (PEXG). Comlex group included patients who had uveitic glaucoma, chronic angle-closure glaucoma (CACG), and neovascular glaucoma (NVG). |
|||
Table 2: Distribution of glaucoma types between patients who underwent trabeculectomy and Ex-PRESS shunt implantation.
Preoperative IOP was a little higher among patients who underwent trabeculectomy (22.15 vs. 21.55 mmHg), but this difference was not statistically significant (P = 0.642). Preoperative number of antiglaucoma medications was lower among patients who underwent trabeculectomy (4.09 vs. 4.42). This difference was not statistically significant (P = 0.135).
Outcome measures
No significant difference in the postoperative IOP at 6 and 12 months was demonstrated (P= 0.401 and 0.701) (Figure 1). Postoperative number of antiglaucoma medications was higher among patients who underwent trabeculectomy (1.08 vs. 0.85). This difference was not statistically significant (P = 0.962) (Figure 2).
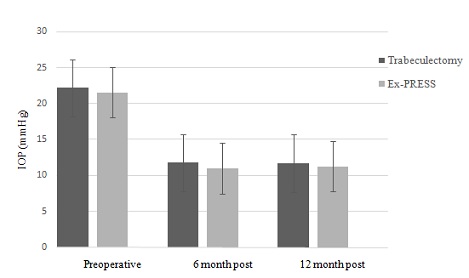 Figure 1: Intra ocular pressure (IOP) preoperative, 6 and 12 month postoperative.
Figure 1: Intra ocular pressure (IOP) preoperative, 6 and 12 month postoperative.
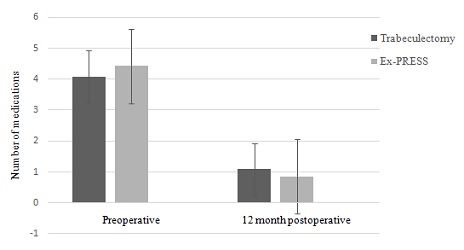 Figure 2: Preoperative and 12 month postoperative number of antiglaucoma medications.
Figure 2: Preoperative and 12 month postoperative number of antiglaucoma medications.
Among patients who underwent trabeculectomy, success was achieved in 12 (92.3%) eyes. Complete success was achieved in 7 (53.8%) eyes and qualified success was achieved in 5 (38.5%) eyes.
Among patients who underwent Ex-PRESS shunt implantation, success was achieved in 24 (88.9%) eyes. Complete success was achieved in 12 (44.4%) eyes and qualified success was achieved in 12 (44.4%) eyes. No significant differences were found between the groups in the rates of overall, complete or qualified success.
Complications, failure analysis and the rate of reoperations
The complications found in the study varied widely and ranged from one case of ciliary block, to encapsulation, uveitis and bleb leakage. There were 3 with high IOP, 2 with low anterior chamber and 3 with hypotony – within which 2 were complicated by choroidal detachment. There was no endophthalmitis. However, while there were more post-operative complications recognized in trabeculectomy patients (46.2% and 19.3% respectively), there was no statistical significance to this finding (P = 0.135). In 13.6% (6 eyes) there was a need for a reoperation for uncontrolled glaucoma. In that group, 2 eyes had been treated with a trabeculectomy and 4 with the Ex-Press shunt.
Failures were recorded in 4 eyes (9%), of which 1 was from the group that underwent trabeculectomy and 3 had the Ex-PRESS procedure. There was no correlation between patients and their surgical data. Complications data and the need for another surgery can be found in table 3.
|
|
Total (N=44) |
Trabeculectomy (N=13) |
Ex-PRESS (N=31) |
|
No Complications |
32 (72.7) |
7 (53.8%) |
25 (80.6%) |
|
Complications |
12 (27.2%) |
6 (46.2%) |
6 (19.3%) |
|
|
High IOP |
2 (33%) |
1 (16%) |
|
|
Ciliary block |
1 (16%) |
0 |
|
|
Encapsulation |
1 (16%) |
0 |
|
|
Anterior Uveitis |
1 (16%) |
0 |
|
|
Low ACD |
0 |
2 (33%) |
|
|
Hypotony |
1 (16%) |
2 (33%) |
|
|
Bleb leakage |
0 |
1 (16%) |
|
Need for another surgery |
6 (13.6%) |
2 (15.3%) |
4 (12.9%) |
|
|
Needling |
2 (66%) |
0 |
|
|
Trabeculectomy |
1 (33%) |
0 |
|
|
Anterior chamber gas injection |
0 |
2 (50%) |
|
|
DMEK |
0 |
1 (25%) |
|
|
Revision of bleb |
0 |
1 (25%) |
|
|
PKP and Ex-PRESS |
1 (33%) |
0 |
|
Intra ocular pressure (IOP), Anterior chamber depth (ACD), Descemet Membrane Endothelial Keratoplasty (DMEK), Penetrating Keratoplasty (PKP) |
|||
Table 3: Distribution of complications post-operative and need for another surgery.
Discussion
In this study, there was no difference found in the efficacy of trabeculectomy vs. Ex-PRESS P-200 shunt in glaucomatous pseudophakic eyes. Although a higher rate of complications was encountered after trabeculectomy, this difference was not found to be statistically significant.
Pseudophakia, has been found by several studies to be a risk factor for failure of trabeculectomy. Takihara et al., showed in a prospective study, that among patients with open-angle glaucoma, trabeculectomy with MMC in pseudophakic eyes after phacoemulsification was less successful compared with that in phakic eyes [2]. The exact mechanism is not clear, possible explanations include-variations in the nature of the aqueous humor, ocular inflammation and breakdown of the blood-aqueous barrier, which may cause bleb failure [3]. The aqueous humor of pseudophakic eyes with glaucoma have also been shown to have high concentration of inflammatory cytokines [18].
Most of the past studies examining the differential efficacy and safety of both procedures, included heterogenous population of phakic and pseudophakic patients [5,9,10,14]. No past studies have addressed directly the efficacy and safety of these procedures in pseudophakic eyes. Most of these studies, had pseudophakic patients as a subgroup analyzed en-bloc as part of the whole study population.
One study that examined this indirectly, was a study by Moisseiev at al., which found no significant differences in the efficacy or safety between the Ex-PRESS shunt and trabeculectomy in IOP reduction. The study arms had an unequal amount of pseudophakic patients, in favor of the Ex-PRESS group- 22 (56%) Ex-PRESS and 17 (28%) trabeculectomy subjects were pseudophakic at baseline. During follow-up, a significantly greater proportion of eyes that underwent Ex-PRESS shunt implantation were pseudophakic (94.9% vs. 67.2% of the eyes that underwent trabeculectomy, P = 0.001). Their secondary sub-analysis demonstrated no significant differences in the results between phakic and pseudophakic eyes. None of the preoperative patient characteristics or surgical details has proven to be associated with the success or failure of any procedure [14].
Regarding the safety profile of the procedures compared, Express P-200 was found to be safer in our study analysis, although the difference was not significant, possibly due to the small sample size in the trabeculectomy group. Another possible explanation for this difference, is the heterogeneity of the baseline glaucoma diagnosis, as the majority of trabeculectomy patients belonged to the complex groups opposed to the Express arm, where most of the patients had POAG at baseline. It is noteworthy, that in spite of this apparently more complex nature of the cases in the trabeculectomy arm, the efficacy was yet similar between the groups, a possible point to add in advantage of the trabeculectomy group in this specific study.
Cost is an important driver when considering the right procedure for patients. One study by Johanna GR at al., has shown Ex-PRESS to have an incremental cost-effectiveness ratio in comparison to the trabeculectomy [15]. Another study by Valentine J at al., concluded that trabeculectomy was “the ‘best buy’ for a glaucoma patient’s health care dollar when the necessary indications are met” [19].
This retrospective study design had some limitations, one of which is potential sources to selection bias. In addition, no age matching was performed between groups. Another limitation was that the study did not evaluate whether clear corneal incision cataract surgery was effective for improving surgical success in pseudophakic eyes.
It is important to note that the preferred surgical technique for pseudophakic patients was Ex-PRESS shunt implantation. Trabeculectomy was performed mainly on eyes that were assumed to be at risk under Ex-PRESS implants, such as closed angle glaucoma, rigid or weak conjunctiva.
In conclusion, this study suggests there is no significant difference between the Ex-PRESS shunt and trabeculectomy in pseudophakic patients, given the same efficacy and higher cost of the former. Nevertheless, a mild trend towards a safer procedure with less complication was found in the Ex-PRESS group. This remains to be approved by RCT’s addressing specifically this subset of pseudophakic patients.
References
- Coleman AL (2012) Advances in glaucoma treatment and management: surgery. Invest Ophthalmol Vis Sci 53: 2491-2494.
- Takihara Y, Inatani M, Ogata-Iwao M, Kawai M, Inoue T, et al. (2014) Trabeculectomy for open-angle glaucoma in phakic eyes vs in pseudophakic eyes after phacoemulsification: A prospective clinical cohort study. JAMA Ophthalmol 132: 69-76.
- Joseph JP, Grierson I, Hitchings RA (1986) Chemotactic activity of aqueous humor: a cause offailure of trabeculectomies? Arch Ophthalmol 107: 69-74.
- Broadway DC, Chang LP (2001) Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma 10: 237-249.
- Wagschal LD, Trope GE, Jinapriya D, Jin YP, Buys YM (2015) Prospective randomized study comparing ex-press to trabeculectomy: 1-year results. J Glaucoma 24: 624-629.
- Good TJ, Kahook MY (2011) Assessment of bleb morphologic features and postoperative outcomes after Ex-PRESS drainage device implantation versus trabeculectomy. Am J Ophthalmol 151: 507-513.
- Sugiyama T, Shibata M, Kojima S, Ueki M, Ikeda T (2011) The first report on intermediate-term outcome of Ex-PRESS glaucoma filtration device implanted under scleral flap in Japanese patients. Clin Ophthalmol 5: 1063-1066.
- Beltran-Agullo L, Trope GE, Jin Y, Wagschal LD, Jinapriya D, et al. (2015) Comparison of visual recovery following Ex-PRESS versus trabeculectomy: results of a prospective randomized controlled trial. J Glaucoma 24: 181-186.
- Netland PA, Sarkisian SR Jr, Moster MR, Ahmed II, Condon G, et al. (2014) Randomized, prospective, comparative trial of EX-PRESS glaucoma filtration device versus trabeculectomy (XVT study). Am J Ophthalmol 157: 433-440.
- Maris PJG, Ishida K, Netland PA (2007) Comparison of trabeculectomy with Ex-PRESS miniature glaucoma device implanted under scleral flap. J Glaucoma 16: 14-19.
- Dahan E, Ben Simon GJ, Lafuma A (2012) Comparison of trabeculectomy and Ex-PRESS implantation in fellow eyes of the same patient: A prospective, randomised study. Eye 26: 703-710.
- de Jong L, Lafuma A, Aguadé AS, Berdeaux G (2011) Five-year extension of a clinical trialcomparing the EX-PRESS glaucoma filtration device and trabeculectomy in primaryopen-angle glaucoma. Clin Ophthalmol 5: 527-533.
- Marzette L, Herndon LW (2011) A Comparison of the Ex-PRESS TM Mini Glaucoma Shunt With Standard Trabeculectomy in the Surgical Treatment of Glaucoma. Ophthalmic Surg Lasers Imaging 42: 453-459.
- Moisseiev E, Zunz E, Tzur R, Kurtz S, Shemesh G (2015) Standard Trabeculectomy and Ex-PRESS Miniature Glaucoma Shunt: A Comparative Study and Literature Review. J Glaucoma 24: 410-416.
- Gonzalez-Rodriguez JM, Trope GE, Drori-Wagschal L, Jinapriya D, Buys YM (2015) Comparison of trabeculectomy versus Ex-PRESS:3-year follow-up. Br J Ophthalmol 100: 1269-1273.
- Chen G, Li W, Jiang F, Mao S, Tong Y (2014) Ex-PRESS implantation versus trabeculectomy in open-angle glaucoma: a meta-analysis of randomized controlled clinical trials. PLoS One 9: 86045.
- Sun Y, Zhang B, Zhou R, Wang T, Deng J (2019) Trabeculectomy and EX-PRESS Implantation in Open-Angle Glaucoma: An Updated Meta-Analysis of Randomized Controlled Trials. Journal of Ophthalmology 2019: 2071506.
- Inoue T, Kawaji T, Inatani M, Kameda T, Yoshimura N, et al. (2012) Simultaneous increases in multiple proinflammatory cytokines in the aqueous humor in pseudophakic glaucomatous eyes. J Cataract Refract Surg 38: 1389-1397.
- Valentine J, Zurakowski D, Ayyala RS (2014) Comparison of acquisition costs of surgical supplies in different health care systems for cataract and glaucoma procedures. J Glaucoma 23: 355-359.
Citation: Rimoni O, Kassem R, Zalish M (2022) Trabeculectomy vs. Express P-200 Shunt Surgery in Post Cataract Patients. J Ophthalmic Clin Res 9: 107.
Copyright: © 2022 Ofri Rimoni, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

