
White Eyed Blow Out Fracture - A Case Report
*Corresponding Author(s):
Aniana Katherine S NicanorDepartment Of Ophthalmology, Rizal Medical Center, Pasig Boulevard, Pasig City, Philippines
Email:ania.nicanor@yahoo.com
Abstract
“White-Eyed Blow Out Fracture (WEBOF)" is a term used for children who had periorbital trauma with mild signs of soft tissue damage. WEBOF can be easily missed, resulting in a lost opportunity for surgical intervention. A pediatric patient presented with vomiting and diplopia after sustaining trauma, she was referred to our institution 2 weeks after a suspected head injury. Examination showed marked limitation on upgaze and downgaze on the right eye with accompanying diplopia. CT scan of the orbits revealed a right orbital floor fracture, with herniation of orbital fat and a mildly thickened right inferior rectus muscle. Patient underwent repair of orbital floor fracture and release of muscle entrapment with silicone implant under general anesthesia. Although release of muscle entrapment and repair of floor fracture was achieved, EOM underaction on vertical gaze and diplopia persisted. Timely diagnosis and intervention of WEBOF is important, not only to reverse the oculocardiac reflex but also to minimize the possibility of permanent ischemic injury and contracture of the involved extraocular muscle, which could lead to long-term strabismus and diplopia.Because the first clinical presentation is similar to that of a head injury, it is often overlooked, resulting in a delay in diagnosis and permanent morbidity.
Keywords
White-eyed blow out fracture; Pediatric facial fractures; Oculocardiac reflex; Orbital floor repair
Introduction
Pediatric facial fractures constitute less than 15% of all facial fractures encountered in the hospital setting. Orbital blowout fractures comprise approximately 20% of all pediatric facial fractures [1]. Specifically, a “white-eyed blow out fracture (WEBOF)’ is even more uncommon and was first described by Jordan et al in 1998 as a term used for pediatric patients sustaining trauma to the periorbital area with minimal external signs of soft tissue trauma (white-eye), ocular motility dysfunction (usually limitation in upgaze), diplopia, lack of enophtalmos, and with radiologic signs of minimal fracture [2].
Usually, these patients present at the emergency room with marked nausea, vomiting, and headache. These are symptoms of the oculocardiac reflex, which may mimic an intracranial injury that commonly distracts from the true etiology, which is the orbital blow out fracture [3]. When this occurs, physicians often mistakenly opt for neurologic monitoring instead of a complete ophthalmologic evaluation. This further leads to a delay in diagnosis and properly timed intervention, resulting in incomplete recovery. In this report, we describe a pediatric patient who was referred to our institution for management of blowout fracture two weeks after her initial injury.
Case Report
A 5-year old female sustained a closed head trauma after she accidentally hit the right side of her face against her sibling’s head. The patient had no external signs of soft tissue injury, but had doubling of vision (binocular and vertical) and pain on eye movement. There was also note of one episode of non-projectile vomiting. No reported loss of consciousness or blurring of vision at that time. Consult was done with a private physician, wherein Magnetic Resonance Imaging (MRI) was requested, but was not done due to financial constraint. Patient was given unrecalled pain medications and was advised observation for five days. In the interim, there was development and subsequent persistence of doubling of vision.
The patient was eventually brought in for consult at our institution two weeks post injury due to persistence of vision symptoms. Visual acuity at presentation was 6/12, improving to 6/10 for both eyes. On gross examination, the patient had no periorbitalhematoma, enophthalmos, dystopia, or subconjunctival ecchymosis (Figure 1). On extraocular muscle examination, there was marked limitation on upgaze and downgaze, with accompanying diplopia and pain of the right eye. Other than the aforementioned Extraocular Movement (EOM) underaction, the patient had no other focal neurological deficits. Coronal Computed Tomography (CT) scanning revealed a right-sided orbital floor fracture with associated minimal intramaxillary sinus herniation of orbital fat, and a mildly thickened right inferior rectus muscle with minimal surrounding fat stranding (Figure 2).
 Figure 1: Raccoon photograph of the patient, as seen on the day of first presentation, day 14 post-injury, with right-sided white-eyed blowout fracture and with no soft tissue clinical signs of injury. Photograph was taken on primary gaze.
Figure 1: Raccoon photograph of the patient, as seen on the day of first presentation, day 14 post-injury, with right-sided white-eyed blowout fracture and with no soft tissue clinical signs of injury. Photograph was taken on primary gaze.
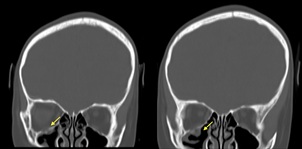 Figure 2: Cranial CT scan, coronal cuts. A complete fracture is noted involving the right orbital floor, with herniation of orbital fat.
Figure 2: Cranial CT scan, coronal cuts. A complete fracture is noted involving the right orbital floor, with herniation of orbital fat.
The patient immediately underwent orbital floor repair with silicone implant and release of muscle entrapment (Figure 3). Forced Duction Test (FDT) was performed before making the initial muscleincision, which showed restriction on upgaze. FDT was then repeated before closing, which revealed no restriction, confirming that the preoperative tissue entrapment was released completely.
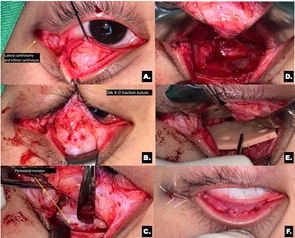 Figure 3: Illustration of surgical technique. A) Transconjunctival approach with lateral skin extension B) Plane of dissection created anterior to the orbital septum C) Periosteum is incised on the orbital rim commencing medially towards the lateral portion D) Release of prolapsed and entrapped tissue. E) The implant is placed over the fracture site F) Conjunctiva is closed and lateral canthus is reconstructed.
Figure 3: Illustration of surgical technique. A) Transconjunctival approach with lateral skin extension B) Plane of dissection created anterior to the orbital septum C) Periosteum is incised on the orbital rim commencing medially towards the lateral portion D) Release of prolapsed and entrapped tissue. E) The implant is placed over the fracture site F) Conjunctiva is closed and lateral canthus is reconstructed.
On day three post op, the visual acuity of the patient was still 6/12, improving to 6/10 on both eyes, and still with marked limitation on upgaze and downgaze with associated diplopia (Figure 4). The patient was discharged and was started on Prednisone 10mg once a day for seven days (0.5mg/ kg/day).
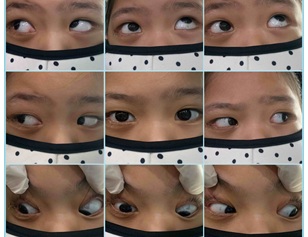 Figure 4: Day 3 post-surgical intervention. Extra-ocular movement testing showed under action of right globe motility on superior and inferior gazes.
Figure 4: Day 3 post-surgical intervention. Extra-ocular movement testing showed under action of right globe motility on superior and inferior gazes.
On Day 20 post op, no change in VA was noted and patient still had EOM underaction on vertical gazes with associated diplopia (Figure 5). Forced duction test was again performed which revealed no restriction. Patient was then referred to Pedia-Ophtha service and was given a refraction of OD: +1.50sph () -1.00cyl × 180; OS: +2.50sph () -1.50cyl × 180. The plan was to observe and to reassess after six months to determine if there will be a need to do corrective strabismus surgery.
 Figure 5: Day 20 post-surgical intervention. Extra-ocular movement testing showed underaction of the right globe motility on superior and inferior gazes.
Figure 5: Day 20 post-surgical intervention. Extra-ocular movement testing showed underaction of the right globe motility on superior and inferior gazes.
Discussion
The pathophysiology of orbital blowout fracture is the subject of two theories; According to the buckling hypothesis, a fracture is caused by a force that is applied to the orbital rim and is then sufficiently transmitted towards the orbital floor. In contrast, a blowout fracture functions as a pressure release valve according to the hydraulic theory. The impact force raises the intraorbital pressure, which is then passed towards the orbital bones nearby and causes a fracture at the point of least resistance [4].
Children and adults tend to incur different types of orbital wall fracture. Children's bones have a weak cortex and a thick cancellous component, making them more pliable. A thicker overlaying orbital floor and incomplete pneumatization of the maxillary sinuses in children often result in a trapdoor mechanism when there is a fracture. However, in adults, their bones are more brittle, with well-aerated maxillary bones, which means that their orbital floorsare thinner and wider spanning. Hence, a fracture usually occurs with a spacious orbital floor defect and without a snapping trapdoor mechanism. This reduces the risk of muscle incarceration and ischemia [5].
Children's more flexible facial buttresses often bend rather than break, resulting in trapdoor injuries. Soft tissue is forced into the defect as the trapdoor opens, and when it snaps shut, becomes effectively entrapped within the linear fracture. Moreover, the inferior rectus muscle is frequently confined inside the bony boundaries of the fracture together with the orbital fat, leading to the classic clinical symptoms of WEBOF and possibly also causing ischemic damage to the muscle [5,6].
It is important to recognize and treat orbital floor fractures in children because orbital soft tissue entrapment may generate the oculocardiac reflex. This constitutes a triad of symptoms: bradycardia, nausea, and faintness. Although the risk of oculocardiac reflex is very rare, these symptoms may be fatal and thus warrant urgent surgical intervention [4,7].
In a 2018 research, Yamanaka et al. examined patients with orbital-floor blowout fractures who had surgery after being injured. According to their findings, individuals who had surgical repair within eight days of the damage fared much better in terms of postoperative diplopia than those who waited longer [8]. Reduced perfusion and consequent fibrosis are caused by the prolonged incarceration of the inferior rectus. This results in marked restriction of superior movement of the eye and hence persistent diplopia on upgaze [2]. In addition, Yew et al suggested that persistent diplopia is the most common complication of those sustaining white-eyed blowout fractures. The recovery time for post-operative persistent diplopia ranges from 25 days up to 18 months, with a longer recovery time in a younger age group [6].
Given that surgical intervention was done on our patient on Day 14 and recovery was not optimal, this supports the study of Yamanaka et al. It is also important to point out that our patient had persistent diplopia on upgaze, much like what was reported by Yew et al.
Conclusion
It is important to arrive at a correct diagnosis when encountering a white-eyed blow out fracture (WEBOF) because it is commonly mistaken for an intracranial injury. When presented with a patient sustaining a trauma to their periocular area with ocular motility dysfuction and with minimal soft tissue signs of trauma, it is pertinent to request for a coronal CT scan and do a complete ophthalmologic exam. Timely diagnosis and intervention of WEBOF is important, not only to reverse the oculocardiac reflex, but also to minimize the possibility of permanent ischemic injury and contracture of the involved extraocular muscle, which could lead to permanent strabismus and diplopia in the long term.
References
- Zimmermann CE, Troulis MJ, Kaban LB (2006) Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg 35: 2-13.
- Balaraman K, Patnaik JSS, Ramani V, Bhat K, Thomas D, et al. (2020) Management of White-Eyed Blowout Fracture in the Pediatric Population. Journal J Maxillofac Oral Surg 20: 37-41.
- Mehanna P, Mehanna D, Cronin A (2009)White-eyed blowout fracture: another look. Emerg Med Australas 21: 229-232.
- Nikolaenko VP, Astakhov YS (2015) Orbital Floor Fractures. In: Nikolaenko VP, Astakhov YP. (eds) Orbital Fractures. Springer, Berlin, Heidelberg.
- Black E, Nesi F, Gladstone G, Levine MR (2020) Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery, Springer New York, NY.
- Yew CC, Shaari R, Rahman SA, Alam MK (2022) White-eyed blowout fracture: Diagnostic pitfalls and review of literature. Injury 46: 1859-1859.
- Burnstine MA (2002)Clinical recommendations for repair of isolated orbital floor fractures. Ophthalmology 109: 1207-1210.
- Yamanaka Y, Watanabe A, Sotozono C, Kinoshita S (2018) Impact of surgical timing of postoperative ocular motility in orbital blowout fractures. Br J Ophthalmol 102: 398-403.
Citation: Nicanor AKS, Valencia MRPI (2022) White Eyed Blow Out Fracture - A Case Report. J Ophthalmic Clin Res 9: 102.
Copyright: © 2022 Aniana Katherine S Nicanor, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

