
Music Therapy for Non-Alzheimer’s Disease Dementia: A Systematic Review
*Corresponding Author(s):
Melissa Mercadal-BrotonsMt Bc, SMTAE, Escola Superior De Música De Catalunya, Barcelona, Spain
Tel:+93 5868028,
Email:brotons@compuserve.com
Abstract
Background
It is estimated that 6% of the population aged 65 or older has dementia. Although dementia is a syndromic entity, there are distinct subtypes that differ in their etiology, presentation form, and clinical course and associated disorders. Studies in music and or music therapy have mainly focused on Alzheimer’s disease.
Objective
A systematic review of published scientific articles was performed on the existent research studies on music therapy with non-Alzheimer disease dementia patients in order to provide clinical recommendations regarding music therapy interventions.
Methods
The search sources included Scopus; PubMed and Science direct electronic data bases in order to identify potential articles to be included. The keywords used were music or music therapy and dementia, Vascular dementia, Lewy bodies dementia, Mixed dementia, dementia in Parkinson’s Disease, Frontotemporal dementia, and Huntington’s disease. The criteria for inclusion included: (1) The articles had to be published in scientific journals; (2) Only scientific articles in English, Portuguese and Spanish languages; (3) Results had to be reported in quantitative and qualitative data; and (4) Participants had to include people diagnosed with non-Alzheimer’s type dementias.
Results
The database search was carried out in April 2017. A total of 151 sources were identified of which six were included in the review comprising three case studies, two Randomized Control Trials (RCT) and one with in subjects design study. The total number of participants was 136. Active music therapy techniques were used in all studies and included singing songs and playing instruments with live music, improvisation and music listening accompanied by musical instruments. Five of the six interventions were led by professional music therapists. The studies reported positive results in relation to their interventions.
Conclusion
Due to the limited number of articles on music therapy with non-Alzheimer’s types of dementia, it is not possible to make specific recommendations for music therapy interventions. The results of the sources analyzed show that active music therapy seems to be a safe and effective treatment for all types of dementia. However, it is recommended that future studies contemplate and highlight the diversity of symptoms and course of the disease of the different types of dementias in order to identify and better understand the music therapy interventions best suited for each of them.
INTRODUCTION
Natural aging is a complex and continuous process that begins with conception and ends with death. It involves an interaction of physical, psychosocial, and cognitive factors, among them memory alteration. However, when these changes begin to evolve rapidly, we may face a dementia process [1].
Dementia is an acquired, progressive neurological syndrome which is common after age 65. It is characterized by a persistent deterioration of the superior mental functions that provoke alteration of the capacity of the individual to carry out the activities of the daily life as well as social and/or occupational commitment. However, there is no alteration of the level of consciousness. In addition, dementias may be associated with other diseases [2,3].
It is estimated that 6% of the population aged 65 years or older have dementia and this number increases to 45% in people aged 85 years or over [3,4]. By 2015, there were about 47 million people with dementia worldwide and according to population projections, if the prevalence of current dementia remains constant, by 2050 there will be approximately 130 million people affected by the disease [5]. Alzheimer's disease is the most common type of dementia, with a prevalence of 60% to 70% of cases. Dementia represents a high cost to society. According to estimates by Alzheimer's disease International, in 2010 the global cost of the disease surpassed 604 million dollars and in 2015 increased by 35% to 818 million dollars [4].
Although dementia is a syndromic entity, there are distinct subtypes that differ in their etiology, presentation form clinical course and associated disorders (Table 1). Alzheimer's Disease (AD), Vascular Dementia (VD) and mixed forms of AD with components of cerebrovascular alteration represent the most frequent subtypes. Other forms of neurodegenerative dementias, caused by brain injuries or use of toxins among others, are much less frequent [6].
|
Degenerative Disorders |
Alzheimer’s Disease |
|
Dementia of Vascular Causes |
Vascular Dementia |
|
Other Causes of Dementia |
Traumas |
Table 1: Causes and types of dementia.
In spite of the existence of numerous subtypes of dementias, only six will be described, due to the fact that they are better known, present similar characteristics in regards to the time of evolution (between 10 and 20 years) and that music therapy is a possibility as a non-pharmacological intervention.
Vascular Dementia (VD)
This is the second most common type, has an earlier onset in relation to AD, affects more men than women and can coexist with AD. The onset of cognitive deficits is temporally related to one or more cerebrovascular events and it can often be abrupt with a gradual or fluctuating course. The diagnostic criteria includes: a) A documented history of stroke (CVA), with cognitive decline temporally associated with the event; b) Physical signs consistent with stroke and c) Evidence of decline regarding the speed of information processing, attention and/or frontal executive functioning. The cognitive domains evaluated include attention and speed of processing, frontal executive functions (planning, decision making, working memory, mental flexibility (judgment), learning and memory, language, oculo-constructive and perceptual abilities, praxia, gnosia, body schema and social cognition [7]. Vascular cognitive impairment is the result of a vascular pathology of any severity, and can range from mild cognitive impairment to dementia. The dementia must only be caused by vascular pathology and is uncommon [8,9].
Mixed Dementia (MD)
The concept of mixed dementia encompasses a broad spectrum between AD and vascular pathology including at one extreme case with minimal AD-related pathology and small macrovascular and microvascular changes and, at the other extreme, cases with severe AD changes and slight vascular involvement. Although the most common association is between vascular disease and AD, it may coexist with Lewy Body disease and other neurodegenerative or inflammatory disorders [10-15].
Frontotemporal Dementia (FTD)
This has an insidious onset and slow progression. Its main characteristics are: behavioral disorders (early loss of personal care, social criticism, disinhibition, cognitive rigidity and inflexibility, hyper-reality such as eating eccentricities, binge eating, alcohol consumption, cigarettes, oral exploration of objects, stereotyped and perseverative behaviors; affective symptoms (depression, anxiety, excessive sensitivity, suicidal ideation, delirium, hypochondria, affective indifference, amimia); language impairment (progressive reduction of discourses and vocabulary, echolalia and perseveration, and late mutism); physical signs (early onset of early reflexes, early incontinence, trisomy appearance of akinesia, stiffness and tremor). Space guidance and praxis are preserved. Although behavioral changes are clinically dominant, some cognitive changes are important and are associated with behavioral changes. The main cognitive alteration in FTD is executive dysfunction, characterized by deficiency in judgment, decision-making and problem-solving, in planning, organization, attention, abstraction and mental flexibility. In contrast, the primary instrumental abilities of language, elemental visual perception, spatial abilities, and memory are well preserved, especially in the early stages of the disease. This characteristic contrasts with most of the other dementias, since they present primary amnesia [16-19].
Huntington Disease (HD)
Huntington disease is a here do degenerative central nervous system disorder characterized by a combination of motor, cognitive and psychiatric symptoms, and eventually, severe hypokinesia and dementia [20]. The initial symptoms are insidious. The average age of onset varies between 35 and 45 years, and can manifest at any age. The average survival time in HD ranges from 14 to 17 years, but can be as long as 40 years. At the cognitive level, dementia is considered one of the cardinal signs of HD. The most affected cognitive functions are recent memory and remote memory, procedural memory for motor tasks, learning, flexibility and attention. Language disorders are not common. However, if present, they are usually related to naming and paraphrasias. Change in verbal fluency is common. They present impairment in oculo-spatial functions, difficulties in planning, organization and program of activities, functions attributed to the frontal lobe. Due to the peculiarities of the cognitive impairment (slowness of thought, abnormalities in problem- solving, judgment, abstraction, attention, concentration and motivation, besides the presence of psychopathological symptoms (especially apathy and irritability) in addition to lesions in the basal ganglia, the HD is considered as one of the sub cortical dementias [17-20].
Lewy Body Dementia (LBD)
Lewy body dementia is a primary degenerative neuropsychiatric syndrome, which begins at an advanced age and is insidious. It presents cognitive, motor and psychiatric symptoms. LBD accounts for 20% to 30% of autopsies from pathological clinical studies of dementias. Clinical and pathological features are very similar to dementia in PD (DPD). It presents cortical alterations (memory, language, executive and visuospatial functions) as well as sub cortical ones (attention, speed of cognitive processing and visuo-constructive functions) [22,23].
Dementia in Parkinson’s disease (DPD)
Parkinson's Disease (PD) is a progressive and degenerative disorder of the Central Nervous System (CNS). It presents motor symptoms (bradykinesia, tremor, stiffness, postural and gait alterations) and non-motor symptoms that may appear in the pre-motor phase such as: sleep disorders, depression and cognitive alterations that progress with the evolution of the disease [24,25]. About 50% of patients with PD without dementia has some form of cognitive impairment since some cognitive domains may be affected, without, however, forming a dementia picture. Mild Cognitive Impairment (MCI) occurs in 20% to 50% of patients with PD and is recognized as a risk factor for further development of dementia in PD [26]. About 10% of people with PD per year develop dementia [27]. Dementia in PD is mainly characterized by memory deficits, attention, executive dysfunctions such as difficulty in problem solving, concept formation, elaboration of strategies, reduction of capacity for changes in patterns, slowing of thinking (bradifrenia) due to bradykinesia, secondary memory impairment. The storage of new information remains relatively preserved [28,29]. Changes in behavior tend to be manifested in various ways and may be due to the side effects of the use of various medications for the treatment of PD, and even cognitive symptoms [30].
Table 2 presents a summary of the area’s most affected by the different types of non AD dementias.
|
|
Motor |
Psychological/Psychiatric |
Behavior |
Cognitive |
Social |
|
Vascular |
x |
? |
|
X |
|
|
Mixed |
? |
? |
|
X |
|
|
Frontotemporal |
x |
x |
x |
X |
X |
|
Huntington |
x |
x |
|
X |
|
|
Lewy Body |
x |
x |
|
X |
|
|
Parkinson |
x |
x |
|
X |
|
Table 2: Aspects most frequently altered in the different dementias.
TREATMENT
Treatment for dementia should include a combination of medication and non-pharmacological strategies. In the latter category we can include music therapy which has shown positive effects especially with AD. Music therapy intervention in dementia has a long history. There is a growing body of empirical evidence suggesting that music may be a useful intervention for the treatment of a variety of dementia symptoms in the different stages of the disease. The benefits of music therapy and music-based interventions in dementia have included improvements in cognitive functioning, social engagement, behavioral and psychological symptoms, and quality of life [31]. One of the explanations for these positive effects may be the fact that musical memory is considered independent of other memory systems. A study by showed that musical memory is closely related to the caudal anterior cingulate cortex and the pre-supplementary motor area [32]. The authors showed that these regions in patients with AD suffered minimal cortical atrophy, decreased deposition of beta-amyloid biomarker and hypo metabolism. The conjunction of these three factors was important to define that musical memory is well preserved even in advanced stages of Alzheimer's disease.
King et al. studied the effect of music therapy on the improvement of agitation, anxiety and behavioral symptoms of individuals with AD [33]. They used the technique of music listening of familiar songs and were evaluated by functional magnetic resonance. The results showed that music with special meaning for a person activates the supplemental motor area and enlarges the functional connection in the cortico-cortical and cortico-cerebellar networks. The personalized songs, according to the authors, can activate the brain, especially of those at an advanced stage who are losing contact with their environment.
The purpose of this study is to present a systematic review of the scientific literature published in English, Portuguese and Spanish concerning the use of music and music therapy with people with non-AD types of dementia focusing on the following types: VD, DLB MD, DPD, FTD and HD. The specific research questions of this systematic review are:
• What are the areas of treatment most often addressed in music therapy with non-Alzheimer type dementias?
• What are the methodologic aspects of music therapy intervention? (number, frequency and duration of sessions, types of professionals leading the
interventions, group vs. individual setting, areas addressed in the music therapy interventions, music therapy techniques)
• What are the effects (outcomes) of music therapy interventions on the different domains affected by a non-Alzheimer type dementia?
Based on the results of the literature review, a list of criteria and recommendations will be provided to guide music therapists in the selection of appropriate music therapy interventions and assist caregivers to make informed choices about appropriate music techniques and resources to use with patients with the different diseases.
METHOD
Search strategy and inclusion criteria
Study selection
Critical appraisal
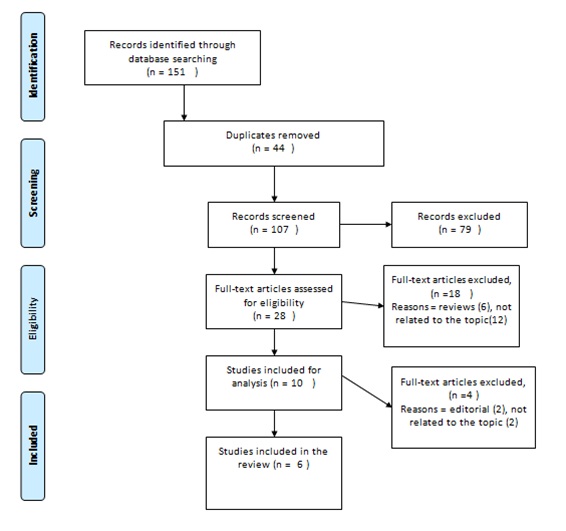 Figure 1: Prisma flow chart.
Figure 1: Prisma flow chart.This systematic review has included the following phases:
• Article search in databases
• Exclusion due to duplication and other criteria
• Reading of all the eligible articles and new exclusion of sources
• Reading and information/data extraction of included sources
• Analysis of the results
Data extraction and management
Two reviewers independently extracted relevant data from publications using a standardized form. The fields included in this form were: article information [author(s), year, country where the study was conducted], participant details (dementia type and severity, number of participants recruited, clinical context, areas addressed in music therapy intervention, group vs. individual intervention, music therapy techniques, total number of sessions, duration and frequency of sessions, study design, outcome measures, results and type of professional conducting the intervention. Qualitative data were also collated.
RESULTS
|
Author |
Year |
Country |
N/Type and Stage of Dementia |
Areas addressed |
Clinical Context |
Music Intervention |
Individual /group |
# Sessions |
Frequency of sessions |
Length of sessions |
Professional |
Study Design |
Outcomemeasures |
Mainfindings |
|
Suzuki et al. |
2004 |
Japan |
N= 10
Stageofdementia NS
|
|
Dementiaunit in a geriatric hospital |
-Singingsongs |
Group |
16 |
2/w |
60 min. |
MTx |
Case studies |
MMSE |
Positive, but not significant, changes in MMSE and N-ADL for MT group |
|
Raglio et al. |
2008 |
Italy |
N=50
Moderate-severedementia
|
BPSD |
NS |
-Non-verbal approach using rhythmic and melodic instruments |
NS |
30 |
NS |
30 min. |
MTx |
RCT |
MMSE |
NPI score significantly decreased for the MT group at 8th, 16th and 20th weeks. |
|
Ridder et al. |
2009 |
Denmark |
N = 2 Severedementia |
|
Psychiatric Nursing Home |
|
Individual |
16 |
4/week |
20-30 min. |
MTx |
Mixedmethod |
ADRQL |
Case A: Participación activa en MT; improvement in QoLDecrease in agitation; increase in BPSD |
|
Raglio et al. |
2012 |
Italy |
N= 1 FTD Severe |
BPSD |
Alzheimer’sunit in a nursing home |
Active MT: Sonorous music relationship |
Individual |
50 |
2/week |
30 min. |
MTx |
Case study |
NPI |
NPI, CMAI and CSDD scores drecreased noticeably and behavioral disturbances (persisten vocalizations, crying, wandering, and purposeless movements greatly improved |
|
Narme et al. |
2014 |
France |
N=48
- Mixed (NS) Moderate-severedementia |
-Emotionalstate. |
Nursing home |
Singing and/or playing instruments while music was played on a CD |
Group |
8 |
2/week. |
60 min. |
Psychologist |
RCT |
SIB |
Significant improvements in emotional facial expressions for the music group. |
|
Cheong et al. |
2016 |
Singapore |
N=25
Withorwithout Delirium
Severestage |
-Mood |
Acutecareunit in a hospital |
CMT:
|
Individual |
2 |
NS |
30 min. |
MTx |
WSD |
MPES |
Engagement: |
Table 3: Studies Characteristics.
MT: Music Therapy; MTx: Music Therapist; BPSD: Behavioral and Psychological Symptoms of Dementia; QoL: Quality of Life; NS: Not Specified; SIB: Severe Impairment Battery; CMAI: Cohen-Mansfield Agitation Inventory; EFE: Emotional Facial Expression; STAI-A: State Trait Anxiety Inventory for Adults; FTD: Frontotemporal Dementia; ADRQL: Alzheimer Disease Related Quality of Life; SI: Social Interaction; AS: Awareness of Self; FM: Feelings and Mood; EA: Enjoyment of Activities; RS: Response to Surroundings; MPES: Menorah Park Engagement Scale; OERS: Observed Emotion Rating Scale; WSD: Within Subject Design; CMT: Creative Music Therapy; MOSES: Multidimensional Observation Scale for Elderly Subjects; CgA: Salivary chromogranin A; NM: N type Mental States Scale; N-ADL: N type Activities of Daily Living; CG: Control group (non-randomized); RCT: Randomised Control Trial; WSD: Within Subjects Design)
Participants
From the data available (N= 88), the mean age of participants was 81 and included 56 females and 32 males. Measures of patients’ cognition and dementia severity were available from the majority of reports, and the participants were classified in the moderate-severe stages of the dementia. Of the six studies, five of them recruited participants from nursing homes or units from a geriatric hospital. The other study does not include this information.
Interventions
Methodological aspects of interventions
The number of music therapy sessions in the six studies analyzed ranged from 2-50, with a mean of 10 sessions. The frequency of sessions was twice a week in all studies except for one in which sessions took place four times a week. Regarding the length of the sessions, in four of the studies the duration was of 30 min., and in two, 60 min. In three of the studies, the music therapy interventions took place individually (case studies), in two in a group setting, and in one study it is not specified. As outcome measures, all studies used standardized tests.
Professionals conducting interventions
Effectiveness of interventions
DISCUSSION
This review examined published research studies on the effect of music therapy on people with non-Alzheimer's dementia. Keeping the focus on the proposed objective, the quality and level of evidence of the articles were not evaluated. It was revealing to observe that there is a dearth of publications specific on the topic of music therapy with non-Alzheimer dementias. Considering the case ranking, it can be said that there is still a disproportion regarding the amount of publications on the other dementias, which are not AD. If we are looking for evidence, of the six articles included, only two were RCTs.
It is clear that AD is the most frequent type of dementia followed by vascular dementia [6]. However, given that clinical manifestations are different for each one of them, and that all treatment should be patient-centered, it is necessary to increase the number of investigations with non-AD patients to evaluate specific and specialized music-therapeutic interventions to support the evidence-based music therapy practice with this population.
Regarding the number of participants, in the studies reviewed in this paper, for which the total was 136, it is worth remembering that there is great difficulty in recruiting patients for research due to their clinical conditions (physical, psychological, cognitive and behavioral) which may pose difficulties with their daily life. Apathy is one of the most frequent neuropsychiatric symptoms these patients present, which negatively interferes with treatment outcomes and reduces daily activities [41]. Moreover, this data seems to be in agreement with reports from clinical practice which show that the patient with dementia usually seeks non-drug treatment only in more advanced phases, and in the initial stages they rely more on medication and medical follow up. Another aggravating factor is that many professionals in some countries have not yet adhered to the multidisciplinary treatment and therefore do not guide patients in this sense. Thus, the music therapist along with other professionals, are rarely sought for follow-up in the early stages of the disease, when patients have better clinical conditions to move to other sites. Moreover, drug costs are high, and it can be difficult for some persons with dementia to access other forms of treatment apart from medical and/or drug treatment [4].
Regarding specific music therapy interventions, it was observed that the music therapy interventions proposed in the studies have not reported the results separately for the different types of dementia. Considering the clinical and evolutionary peculiarities and the phases in which each patient was, we question if the participants responded in the same way to music therapy and if generalization of music therapy interventions for any type of dementia is appropriate. Despite the type of dementia, the results of the studies analyzed showed that active and interactive music therapy, conducted by a certified professional music therapist, was the most used in all studies included in this review. An average of two 30-minute sessions per week for individual sessions, and60-minutes sessions for group ones, were observed. In addition, the use of familiar songs, playing percussion instruments, live music, recorded music, music listening accompanied by percussion instruments, all showed positive results on the analyzed variables (cognition, behavioral-psychological symptoms of dementia, stress and quality of life. These results do not appear to differ much from those obtained in other studies with people with dementia in the moderate-severe stages of the disease (Mercadal-Brotons, in press).Contrary to our results, a meta-analysis by Kelvin et al. showed that receptive music therapy was more effective than active music therapy in reducing agitation, anxiety problems and behavioral symptoms in older adults with dementia and defended its application since it is ideal for use in nursing care homes and in the home of the patient besides being low cost [42]. However, other RCTs, systematic reviews and meta-analysis show that interactive music therapy seems to be more effective in the treatment of disruptive behaviors and anxiety and a positive trend to treat cognitive function, language and communication, depression, and quality of life of elderly patients with dementia [43,44].
We want to highlight the Frontotemporal dementia which presents some special characteristics, among them musical ability. Patients, after the onset of the disease, may present artistic abilities not previously present. The explanation for this feature may be that FTD occurs predominantly in the frontal and/or temporal lobe, and that the inferior frontal gyrus plays an important role in the generation of spontaneous actions. If inhibition of the activity of this region occurs, it may result in a possible "release" effect of the neural network associated with greater creativity [45]. Also, there are anatomical correlates for musical ability in FTD, when patients show predominant dysfunction in the left anterior temporal lobe. This information is important in order to reflect on the role of music therapy in the treatment of FTD patients.
CONCLUSION
This systematic review identified very little research on music interventions/music therapy with people with non-AD dementia. It is therefore difficult to provide recommendations for music therapists as well as caregivers regarding the types of interventions which are most suited to address the different needs of non-AD patients. The results of this review show that the current music therapy interventions with people with non-AD dementias are not different from those with AD in spite of the difference in the clinical manifestations, stage and course of the different types of dementia. In fact, those studies that include several types of dementias, do not report results separately for each type of dementia, so it is hard to know if non-AD patients respond any differently from AD patients to specific music therapy interventions. For future studies, it is recommended that the music therapy techniques used in the interventions should be described in detail and that standardized intervention protocols should be used, so that the results are more methodologically reliable. It is also recommended that the outcome evaluations follow some type of protocol in regard to the number of sessions after which data is collected.
The analysis of individual data (case studies) and non-randomized studies are important as beginning stages to promote higher scientific level studies with more powerful designs such as randomized controlled trials. Research with people with non-AD dementias is at the beginning stages. Altogether, the review highlights the clear and urgent need for research in this area so that music therapy professionals can have evidence-based protocols to manage the specific needs and peculiarities of the different types of dementia.
REFERENCES
- Karr JE, Graham RB, Hofer SM, Muniz-Terrera G (2018) When does cognitive decline begin? A systematic review of change point studies on accelerated decline in cognitive and neurological outcomes preceding mild cognitive impairment, dementia, and death. Psychol Aging 33: 195-218.
- Nitrini R (2012) Conceito de Demência. In Miotto EC, Lucia MCS, Scaff M, Neuropsicologia Clínica São Paulo: Roca 243-255.
- Prince M, Ali GC, Guerchet M, Prina AM, Albanese E, et al. (2016) Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimers Res Ther 8: 23.
- Wimo A, Guerchet M, Ali GC, Wu YT, Prina AM, et al. (2017) The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimers Dement 13: 1-7.
- Prince M, Wimo A, Guerchet M, Ali GC, Wu YT, et al. (2015) World Alzheimer Report 2015: The global impact of dementia an analysis of prevalence, incidence, cost and trends.
- Garre-Olmo J (2018) Epidemiology of Alzheimer’s disease and other dementias. Rev Neurol 66: 377 -386.
- Sachdev P, Kalaria R, O’Brien J, Skoog I, Alladi S, et al. (2014) Diagnostic criteria for vascular cognitive disorders: a VASCOG statement. Alzheimer Dis Assoc Disord 28: 206-218.
- Gold G, Giannakopoulos P, Herrmann FR, Bouras C, Kövari E (2007) Identification of Alzheimer and vascular lesion thresholds for mixed dementia. Brain 130: 2830-2836.
- van der Flier WM, Skoog I, Schneider JA, Pantoni L, Mok V, et al. (2018) Vascular cognitive impairment. Nat Rev Dis Primers 4: 18003.
- Ahtiluoto S, Polvikoski T, Peltonen M, Solomon A, Tuomilehto J, et al. (2010) Diabetes, Alzheimer disease, and vascular dementia: a population-based neuropathologic study. Neurology 75: 1195-1202.
- Attems J, Jellinger KA (2014) The overlap between vascular disease and Alzheimer's disease--lessons from pathology. BMC Med 12: 206.
- Jellinger KA, Attems J (2007) Neuropathological evaluation of mixed dementia. J Neurol Sci 257: 80-87.
- Jellinger KA, Attems J (2010) Prevalence of dementia disorders in the oldest-old: an autopsy study. Acta Neuropathol 119:421-433.
- Nelson PT, Head E, Schmitt FA, Davis PR, Neltner JH, et al. (2011) Alzheimer's disease is not "brain aging": neuropathological, genetic, and epidemiological human studies. Acta Neuropathol 121: 571-587.
- Zheng L, Vinters HV, Mack WJ, Weiner MW, Chui HC (2016) Differential effects of ischemic vascular disease and Alzheimer’s disease on brain atrophy and cognition. J Cereb Blood Flow Metab 36: 204-215.
- Caixeta L (2006) Demência Frontotemporal. In L. Caixeta, Demência: Abordagem muldisciplinar (pp.245-263). São Paulo: Editora Atheneur.
- Piguet O, Kumfor F, Hodges J (2018) Diagnosing, monitoring and managing behavioural variant frontotemporal dementia. Med J Aust 207: 303-308.
- Marshall CR, Hardy CJD, Russell LL, Clark CN, Bond RL, et al. (2018) Motor signatures of emotional reactivity in frontotemporal dementia. Sci Rep 8: 1030.
- Seo SW, Thibodeau MP, Perry DC, Hua A, Sidhu M, et al. (2018) Early vs late age at onset frontotemporal dementia and frontotemporal lobar degeneration. Neurology 90: 1047-1056.
- Paulsen JS, Ready RE, Hamilton JM, Mega MS, Cummings JL (2001) Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry 71: 310-314.
- Haddad MS (2006) Doença de Huntington . In L. Caixeta, Demência: Abordagem muldisciplinar. São Paulo: Editora Atheneu 315-331.
- Machado JCB, Castro LR (2006) Demência com Corpo de Lewy In L. Caixeta, Demência: Abordagem muldisciplinar. São Paulo: Editora Atheneur 297-314.
- Thomas AJ, Mahin-Babaei F, Saidi M, Lett D, Taylor JP, et al. (2018) Improving the identification of dementia with Lewy Bodies in the context of an Alzheimer’s-type dementia. Alzheimers Res Ther 10: 27.
- Janvin CC, Larsen JP, Aarsland D, Hugdahl K (2006) Subtypes of mild cognitive impairment in Parkinson’s disease: progression to dementia. Mov Disord 21: 1343-1349.
- Silva DJ (2016) Etiopatogenia da doença de Parkinson. In Silva DJ, Fen CH, & Colleta MVD (edn.), Transtornos do movimento: Diagnóstico e tratamento (pp.39-47). São Paulo. Ed Omnifarma.
- Litvan I, Aarsland D, Adler CH, Goldman JG, Kulisevsky J, et al. (2011) MDS Task Force on mild cognitive impairment in Parkinson's disease: critical review of PD-MCI. Mov Disord 26: 1814-1824.
- Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, et al. (2007) Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 22: 1689-1707.
- Alves G, Larsen JP, Emre M, Wentzel-Larsen T, Aarsland D (2006) Changes in motor subtype and risk for incident dementia in Parkinson’s disease. Mov Disord 21: 1123-1130.
- Goldman JG, Weis H, Stebbins G, Bernard B, Goetz CG (2012) Clinical differences among mild cognitive impairment subtypes in Parkinson’s disease. Mov Disord 27:1129-1136.
- Bocanegra Y, García AM2, Pineda D, Buriticá O, Villegas A, et al. (2015) Syntax, action verbs, action semantics, and object semantics in Parkinson’s disease: Dissociability, progression, and executive influences. Cortex 69: 237-254.
- van der Steen JT, van Soest-Poortvliet MC, van der Wouden JC, Bruinsma MS, Scholten RJPM, et al. (2017) Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev 5.
- Jacobsen JH, Stelzer J, Fritz TH, Chételat G, La Joie R, et al. (2005) Why musical memory can be preserved in advanced Alzheimer’s disease. Brain 138: 2438-2450.
- King JB, Jones KG, Goldberg E, Rollins M, MacNamee K, et al. (2019) Increased Functional Connectivity After Listening to Favored Music in Adults With Alzheimer Dementia. J Prev Alzheimers Dis 6: 56-62.
- Mendeley Ltd., (2018) Elsevier Mercadal-Brotons M (in press). Music therapy for advanced dementia: Needs and clinical interventions. In Tamplin J, Baird A, Garrido S (edn.), Music and dementia: From cognition to therapy, Oxford University Press, Oxford, UK.
- Raglio MA, Maugeri S, Bellandi D, Gianotti M, Ubezio MC, et al. (2012) Music therapy in Frontal Temporal Dementia: A case report. J Am Geriatr Soc 60: 1578-1579.
- Ridder HM, Wigram T, Ottesen AM (2009) A pilot study on the effects of music therapy on frontotemporal dementia - developing a research protocol. Nordic Journal of Music Therapy 18: 103-132.
- Suzuki M, Kanamori M, Watanabe M, Nagasawa S, Kojima E, et al. (2004) Behavioral and endocrinological evaluation of music therapy for elderly patients with dementia. Nurs Health Sci 6: 11-18.
- Narme P, Clément S, Ehrlé N, Schiaratura L, Vachez S, et al. (2014) Efficacy of musical interventions in dementia: evidence from a randomized controlled trial. J Alzheimers Dis 38: 359-369.
- Raglio A, Bellelli G, Traficante D, Gianotti M, Ubezio MC, et al. (2008) Efficacy of music therapy in the treatment of behavioral and psychiatric symptoms of dementia. Alzheimer Dis Assoc Disord 22: 158-162.
- Cheong CY, Tan JA, Foong YL, Koh HM, Chen DZ, et al. (2016) Creative Music Therapy in an Acute Care Setting for Older Patients with Delirium and Dementia. Dement Geriatr Cogn Dis Extra 25: 268-275.
- Theleritis C, Siarkos K, Politis AA, Katirtzoglou E, Politis A (2017) A systematic review of non?pharmacological treatments for apathy in dementia. Int J Geriatr Psychiatry 33: 177-192.
- Tsoi KKF, Chan JYC, Ng YM, Lee MMY, Kwok TCY, et al. (2018) Receptive Music Therapy Is More Effective than Interactive Music Therapy to Relieve Behavioral and Psychological Symptoms of Dementia: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc 4: 1-9.
- Giovagnoli AR, Manfredi V, Schifano L, Paterlini C, Parente A, et al. (2018) Combining drug and music therapy in patients with moderate Alzheimer's disease: a randomized study. Neurol Sci 39: 1021-1028.
- Zhang Y, Cai J, An L, Hui F, Ren T, et al. (2017) Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Res Rev 35: 1-11.
- Kleinmintz OM, Abecasis D, Tauber A, Geva A, Chistyakov AV, et al. (2018) Participation of the left inferior frontal gyrus in human originality. Brain Struct Funct 223: 329-341.
Citation: Mercadal-Brotons M, Alcântara-Silva TR (2019) Music Therapy for Non-Alzheimer’s Disease Dementia: A Systematic Review. J Alzheimers Neurodegener Dis 5: 019.
Copyright: © 2019 Melissa Mercadal-Brotons, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

