
A Comparison of Prophylactic Use of Intravenous Lidocaine versus Vecuronium in Preventing Suxamethonium - Induced Fasciculation and Postoperative Myalgia among Surgical Patients at Hawassa University Specialized Hospital, Ethiopia: Prospective Cohort Study
*Corresponding Author(s):
Bekele BuliDepartment Of Anesthesia, College Of Medicine And Health Sciences, Hawassa University, Ethiopia
Email:bikila444@gmail.com
Abstract
Background
Succinylcholine is the preferred muscle relaxant used for rapid sequence induction with a minor adverse effect that leads to an unpleasant experience for the patients. Administration of IV lidocaine or Vecuronium before succinylcholine has been shown to decrease the incidence and severity of succinylcholine-induced fasciculation and postoperative myalgia.
Objectives
This study aims to compare the efficacy of prophylactic use of intravenous Lidocaine and a low dose of vecuronium in the prevention of Succinylcholine induced fasciculation and postoperative myalgia among surgical patients at Hawassa University Specialized Hospital, 2022.
Methodology
This was a prospective observational cohort study conducted among 124 participants at Hawassa referral Hospital. Patients were randomly assigned to (Group L) and (Group V) based on those who received pretreatment with lidocaine, and vecuronium respectively at the decision of the anesthetist in charge. The Fasciculation, Postoperative myalgia, vital sign, total analgesic consumption after surgery, and adverse effects were recorded. Descriptive data were summarized using descriptive statistics. Categorical and continuous data were analyzed using the chi-square statistics and independent sample t-test respectively. The occurrence of fasciculation and myalgia between groups was compared using the Fischer exact test. A p-value
Results
The results of our study revealed that, the incidence of fasciculation was 28.3% and 40% in the Vecuronium groups and Lidocaine group respectively (p-value <0.05). Furthermore the postoperative myalgia were significantly lower in the Lidocaine group where only 11/ 60 (18.3%) of participants developed postoperative myalgia when compared with vecuronium group in which 22/ 60 (36%) experienced myalgia at 24 hours after surgery at (p-values 0.001).
Conclusion
Based on the results of this study, pretreatment with intravenous lidocaine is more effective than vecuronium in reducing succinylcholine-related postoperative myalgia than after surgery. It was effective in reducing postoperative rescue analgesic requirements.
Keywords
Fasciculation; Lidocaine; Myalgia; Postoperative; Succinylcholine; Vecuronium
Abbreviations
ASA: American Society of Anesthesiologists
BMI: Body Mass Index
SD: Standard Deviation
HUCSH: Hawassa University Comprehensive and Specialized Hospital
MAP:Mean Arterial Pressure
HR: Heart Rate
POM: Postoperative Myalgia
SIF: Succinylcholine induced Fasciculation
SPSS: Statistical Package for Social Science
Introduction
Succinylcholine (Suxamethonium) is still the best choice agent for rapidly providing ideal surgical procedures requiring endotracheal intubation [1]. Unfortunately, its use is associated with muscular fasciculation and postoperative myalgia (muscle pain) in 41–92% of patients [2] although a more recent meta-analysis reports an incidence of succinylcholine-induced fasciculation and postoperative myalgia were between 5 and 83% [3]. The fasciculation occurs almost immediately after the administration of Succinylcholine and is observed as uncoordinated, uncontrollable, vigorous twitching of single muscle groups innervated by single motor nerve fibers. This causes shearing forces and biochemical damage to occur to the muscle cells and tissue which leads to postoperative muscle pain [4].
Postoperative myalgia associated with the administration of succinylcholine is a common clinical problem. Its incidence and severity are very variable, from mild to severe [5]. Postoperative myalgia after suxamethonium administration is a frequent and troublesome complication. The pains most commonly affect the neck, shoulders, chest, and subcostal region and are manifest usually during the first and second postoperative days, particularly in ambulant patients which prolong hospital stay and increase the cost of treatment of postop surgery [6]. Several prophylactic measures have been employed to reduce this incidence, the most commonly used and successful of which had been pretreatment with a small dose of non-depolarizing muscle relaxants before Succinylcholine administration [6-8]. This technique is not without its problems, like difficulties with tracheal intubation and prolonged muscle relaxation may be encountered. The management of this complication remains a challenge for surgical patients and costs a huge burden on the country's economy.
Lidocaine has been an easily available feasible and effective drug for preventing pain. Pretreatment with lidocaine before administration of succinylcholine, in the prevention of postoperative myalgia among surgical patients, may result in reduced anesthetic and opioid use in managing both acute postoperative pain. it avoids many of the complications associated with pretreatment with non-depolarizing agents especially if a non-depolarizing neuromuscular blocking agent is used as pretreatment in a patient with emergency and expected difficult intubation [9-10].
It has been shown that both lidocaine and vecuronium were effective in decreasing succinylcholine-induced fasciculations and postoperative myalgia, but no comparative analysis has been performed to determine which pretreatment is more effective for the prevention of succinylcholine-induced fasciculation and postoperative myalgia. So, it is highly recommended to conduct such research to see their efficacy. Hence, the purpose of this investigation was to measure and compare the incidence and severity of fasciculations and postoperative myalgia in patients who had received pretreatment with either lidocaine or vecuronium before succinylcholine administration among surgical patients.
Methods
Study design, setting, and population
An institutional-based prospective cohort study was conducted at Hawassa University Comprehensive Specialized Hospital from February 01 to April 30, 2022. All ASA I or II adult patients scheduled for elective surgeries under general anesthesia with endotracheal intubation were recruited after informed consent was included in the study. The patient who had an allergy to the study drugs, preexisting neurologic and generalized pains, a history of difficult intubation, potential difficulties in airways, patients with concurrent severe medical illnesses, and pregnant patients were excluded. The study was reported by making it in line with STROCCS guidelines [12]. In addition, we registered this study on the research registry with the unique number of research registry8422, and with a hyperlink of https://www.researchregistry.com/browse-the-registry#home/
Sample size and sampling technique
The sample size for the study was calculated by considering an effect size of 0.5, power (1-β) of 0.80, and a 5% level of significance, the calculated total sample size was 124, which is 62 in each group. Patients were allocated randomly to one of the two groups. Patients in group "V" received 0.01 mg/kg of Vecuronium and group "L" received 1.5 mg/kg, of lidocaine following succinylcholine as the decision of the anesthetist in charge as local protocol [13].
Study variables
- Succinylcholine-induced fasciculation and post-operative myalgia were outcome variables.
- Demographic data (like age, sex, BMI, ASA physical status), premedication, type of surgery, induction agents, analgesics, perioperative vital signs, and complications were the independent variables.
Data collection procedure
Data were collected using structured questionnaires by trained four data collectors. Pre-operatively the patients' socio-demographic, and perioperative clinical conditions were recorded. The data collectors observed and graded fasciculation immediately after the administration of succinylcholine and all patients were visited 24 hours postoperatively in the respective wards and were asked about the presence and severity of myalgia. The severity of fasciculation’s and myalgia was assessed and graded on a four-point scale.
Anesthesia techniques
On arrival in the operating room, each patient had a standard monitor attached, and Baseline pulse rate, temperature, Mean Arterial Pressure (MAP), oxygen saturation, ECG, and respiratory rate were obtained and recorded at 5 min before succinylcholine, one and five min after succinylcholine administration. One minute after pretreatment administration, anesthesia was induced with 2.5 mg/ kg propofol and 1.5 mg/kg pethidine in all groups. In the study hospital, most Anesthetists tried to prevent Succinylcholine-Induced Fasciculation and POM by administering a low dose of IV vecuronium or Lidocaine as induction of anesthesia is given depending on the decision of the anesthetist in charge as local protocol [13-14]. The study participants were grouped into (Lidocaine, and Vecuronium groups); based on their exposure to 1mg/kg Lidocaine, and 0.01mg/kg Vecuronium, pretreatment respectively). After administration of induction, suxamethonium 1.5mg/kg was given intravenously thereafter and each patient will be observed for the occurrence and severity of SIF and POM using a numeric rating scale (see Appendix) in both groups [15]. Standardized postoperative care was given to all patients. Pain related to the surgical procedure was managed with IV tramadol as required regularly.
Data quality control
Data was collected using a pretested self-administered questionnaire with multiple choices and open-ended questions on respondents' socio-demographic characteristics. A pretest was done for 5% of the sample population. Then, possible amendments will be made. During data collection; regular supervision and follow-up were made.
Statistical analysis and interpretation
Data were entered into SPSS version 26 for analysis. Descriptive data were summarized using descriptive statistics. Frequency and percentage were used to describe qualitative variables. Categorical and continuous data were analyzed using the chi-square statistics and independent sample t-test respectively. The presence or absence of fasciculation and post-operative myalgia were compared between groups using the Fischer exact test. A p-value <0.05 was considered significant.
Operational definitions
De-fasciculation dose: administration of 0.01mg/kg of Vecuronium one minute before induction of anesthesia.
Fasciculation; involuntary rapid muscle twitches that can/not move limbs and trunks but are easily felt by patients immediately after succinylcholine administration.
Postoperative Myalgia: Generalized aches and pains at the non-surgical site that commonly occur until 48 hours after succinylcholine administration.
Mild myalgia: -muscle pain or muscle stiffness at one site but not causing disability or limiting activities.
Moderate myalgia: -muscle pain or muscle stiffness at more than one site but not causing disability or limiting activities.
Severe myalgia: -muscle pain at one or more sites and causes limited daily activity
Results
Socio-demographic and clinical characteristics of participants
A total of 124 participants were enrolled in this study, and four of them were not enrolled due to incomplete data leaving 120 for data analysis. No significant differences were revealed in participant’s age, BMI, sex, ASA classification, surgical length, or total tramadol use as shown in (Table 1).
|
Socio-demographics
|
Lidocaine group (n=60) |
Vecuronium group (n=60) |
P-value |
|
Age, years, mean ±SD |
34.45 ± 13.85 |
35.59 ± 13.38
|
0.63 |
|
BMI kg/m2, mean ± SD |
17.94 ± 3.76
|
18.4 ± 4.23 |
0.45 |
|
Male/female ratio |
28:32 |
26:34 |
0.06 |
|
ASA I:ASA II ratio |
40:20 |
33:27 |
0.057 |
|
Surgery length (min) |
129 ± 47(10-190) |
109 ± 65(43-220) |
0.086 |
|
Tramadol total (mg) |
120 ± 47(70-190) |
158 ± 38(97-210) |
0.042* |
Table 1: Demographics and Study Variables of the Participants.
BMI= Body Mass Index, SD= Standard Deviation
In this study, following the administration of succinylcholine, patients in both groups showed a slight rise in the MAP and the heart rate value from the baseline value at 1 minute and up to 5 minutes. However, when we compare their MAP and heart rate before and after administration of succinylcholine, there are also no significant differences between the two groups (P > 0.05) [Figure1].
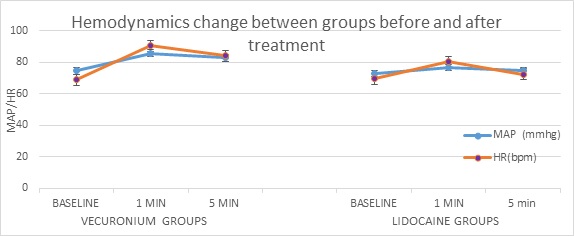 Figure 1: Trend of Hemodynamic Parameters during the Study.
Figure 1: Trend of Hemodynamic Parameters during the Study.
MAP= Mean arterial pressure, HR= Heart Rate, bpm= beat per minute
The Comparison of incidence and severity of fasciculation
The Participants in group "L"(40%) experienced mild to moderate fasciculation, compared to Group “V” where only 28.3% of patients’ experienced mild fasciculation (p < 0.05). The incidence and severity of fasciculation were significantly higher in patients who were pretreated with IV lidocaine as compared with the vecuronium groups. None of the vecuronium group developed moderate or severe fasciculation. Only 10 (16.7%) participants in the lidocaine groups had moderate fasciculation as shown in (Table 2).
|
Fasciculation Grading |
|
Vecuronium Group (n=60) |
Lidocaine Group( n=60) |
P value |
|
Nil |
43(71.7%) |
36 (60%) |
<0.05
|
|
|
Mild |
17(28.3%) |
14(23.3%) |
||
|
Moderate |
0 |
10(16.7%) |
||
|
Postoperative Myalgia Grading |
Nil |
38(63%) |
49(81.7%) |
0.001 |
|
Mild |
14(23%) |
9(15%) |
||
|
Moderate |
8(13%) |
2(3.3%) |
Table 2: Comparison of Incidence and Severity of Fasciculation and Myalgia between the Groups.
Nil= No fasciculation and/or postoperative myalgia
The Comparison of incidence and severity of myalgia
There was a statistically significant difference in the incidence and severity of succinylcholine-induced postoperative myalgia between the two groups at 24 hours. In group "L' 11(18.3%) patients developed mild to moderate myalgia 24 hours after surgery. The statistical analysis showed the postoperative myalgia with lignocaine pretreatment (18.3%) to be significantly less than pretreatment with vecuronium (36%) p < 0.001) as shown in (table 2).
Discussion
Succinylcholine is a popular drug because it rapidly provides the ideal conditions for short procedures requiring endotracheal intubation [16]. However, it is associated with muscular injury manifested in the form of fasciculation’s and postoperative myalgia. These unwanted effects of succinylcholine have limited its usefulness and present distressing consequences for patients after minor surgeries [17].
In our study, participants who received vecuronium had a lower incidence of muscle fasciculation 17/60 (28.3%) when compared to those who had lidocaine, where 24/60 (40%) of patients had fasciculation’s. Furthermore, the overall incidence of myalgia was 18.3% (11/60) in the lidocaine group and 36% (22/60) in the vecuronium group. This shows the incidence and severity of myalgia were significantly decreased in lidocaine pretreatment, compared with vecuronium groups (p=0.01). This shows that there is no relationship between the occurrence of fasciculation’s and the severity of postoperative myalgia. This is consistent with previous research findings [18-20].
Our finding is consistent with other studies in India and California by Senapati LK, et.al, and Al. HR et.al, have shown an overall decrease in the incidence and severity of postoperative myalgia with IV pretreatment of lidocaine and low dose of vecuronium. This intensity of myalgia with succinylcholine has also been observed in other studies too that vary from 20 -80% [15-22]. A meta-analysis done by Schreiber et al concluded that pretreatment with non-depolarizing muscle relaxant or local anesthetic decreased the incidence of fasciculation’s and postoperative myalgia by about 20 to 30 percent on the first postoperative day [17]. This study was designed to compare myalgia after succinylcholine with rocuronium and lidocaine pretreatment. Another study, done by Spence et.al, concluded that lidocaine was significantly better than rocuronium at decreasing the severity of postoperative myalgia, indicating that lidocaine provided better attenuation of postoperative myalgia [5]. In line with our study, a study done in India by Shital Hardin, et.al stated that moderate and severe postoperative myalgia was reported only in (10%, 2.5%) and (5%, 0%) patients at 24hrs respectively that shows a significant decrease in myalgia. They concluded that there is a significant reduction in Post-Operative Myalgia over time within the two groups and lidocaine pretreatment is the more effective in preventing succinylcholine-induced myalgia postoperatively [23].
In contrast to this study, Findlay et.al did not find a statistically significant difference in myalgia between the groups. When they evaluated myalgia on 2nd postoperative day their analysis showed that there is no significant difference in the myalgia between the two groups on the first and second day postoperative days [24].
Other similar studies by [25-26] reported in their study, using lignocaine as a pretreatment agent for the prevention of POM found that 12.8% to 30% of patients experienced postoperative myalgia on the first and second postoperative days. Our study result is in between these two studies. Only 18.3% versus 36%; P<0.001) patients experienced postoperative myalgia after operation in the lignocaine group compare with the vecuronium group, which is nearer to these two studies. The limitation of our study is that fasciculation and myalgia were scored subjectively instead of objective measurements due to the laboratory in the study area having problems procuring the test kits used in measuring these parameters. The second limitation is that we could have included a placebo group as a control and compared both agents with it. But we felt that it would be unethical to use placebo instead of proven agents in participants and so put them in risk of the potential complications of succinylcholine alone.
Conclusion
In conclusion, this study revealed that pre-treatment with Lidocaine demonstrates a better effect on reducing the incidence or severity of succinylcholine-induced myalgia. Pretreatment of Lidocaine is more effective than vecuronium in decreasing the occurrence and severity of myalgia induced by succinylcholine. It decreased postoperative analgesic consumption during the study period, but it failed to demonstrate an association between the intensity of fasciculation and myalgia. Considering this, we suggest using Lignocaine pretreatment to minimize the incidence and severity of succinylcholine-induced myalgia. Furthermore, the use of vecuronium before succinylcholine administration decreased the incidence of severe fasciculation and myalgia. Hemodynamic parameters remained stable after the administration of both drugs.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
References
- Hillier K (2007) Succinylcholine. xPharm Compr Pharmacol Ref 1-5.
- Hossain MS, Sanjowal L, Rashid MM, Babu MAR, Saha D (2020) Prevention of Succinylcholine Induced Postoperative Myalgia by Pretreatment with Lignocaine: A Randomized Controlled Study. Faridpur Med Coll J 14: 13-15.
- Schreiber JU, Lysakowski C, Fuchs-Buder T, Tramèr MR (2005) Prevention of succinylcholine-induced fasciculation and myalgia: A meta-analysis of randomized trials. Anesthesiology 103: 877-884.
- Wong SF, Chung F (2000) Succinylcholine-associated postoperative myalgia. Anaesthesia 55: 144-152.
- Spence D, Domen-Herbert R, Boulette E, Olson RL, Vacchiano C, et al. (2002) comparison of rocuronium and lidocaine for the prevention of postoperative myalgia after succinylcholine administration. AANA J 70: 367-372.
- Farhat K, Waheed A, Bakhtiar S, Pasha AK (2011) Comparative Study of Succinylcholine and Precurarization With Rocuronium on Muscular Effects in Patients Undergoing Surgery Under General Anaesthesia. Clinical Pharmacology 28: 33-41.
- Fatemeh H, Mojgan R (2010) Comparison of atracurium and “mini-dose” succinylcholine for preventing succinylcholine-induced muscle fasciculations: A randomized, double-blind, placebo-controlled study. Acta Anaesthesiol Taiwanica 48: 28-32.
- Senapati LK, Battini KP, Padhi PP, Samanta P (2021) Effect of Non-depolarizing Muscle Relaxants Rocuronium Versus Vecuronium in the Assessment of Post-Succinylcholine Complications in Surgeries Under General Anesthesia: A Randomized Double-Blind Study at a Tertiary Care Hospital. Cureus 13: 1-11.
- Zhong J, Hu J, Mao L, Ye G, Qiu K, et al. (2022) Efficacy of Intravenous Lidocaine for Pain Relief in the Emergency Department: A Systematic Review and Meta-Analysis. Front Med 8:1-11.
- University of Wisconsin Hospitals and Clinics Authority. Systemic Lidocaine for the Treatment of Pain - Adult / Pediatric - Inpatient / Ambulatory / Emergency Department Clinical Practice Guideline (2019) 1-22.
- Amornyotin S, Santawat U, Rachatamukayanant P, Nilsuwankosit P, Pipatnaraphong H (2002) Can lidocaine reduce succinylcholine induced post-operative Myalgia? J Med Assoc Thail 85: 969-974
- Mathew G, Agha R, STROCSS Group (2021) STROCSS 2021: Strengthening the Reporting of cohort, cross-sectional and case-control studies in Surgery. Int J Surg 96:106-165.
- Goshu EM, Emirie YA, Woldemariam LG, Taye MG (2021) A small dose of succinylcholine versus de-fasciculating dose of pancuronium for the prevention of succinylcholine-induced side effects in surgical patients: A prospective cohort study. Perioper Care Oper Room Manag 25:100208.
- FMOH (2016) Ethiopian Hospital Services. Guideline 1:133.
- Abraham V, Kumar AR, Afzal L (2008) Evaluation of Post Succinylcholine Myalgia and Intubation Conditions with Rocuronium Pretreatment?: A Comparison with Vecuronium. Indian J Anaesth 52: 551-555.
- Abbas N, Tariq S, Khan AW, Murtaza G, Naqvi N, et al. (2009) To asses the effects of Rocuronium pretreatment on Succinylcholine induced fasciculations and postoperative Myalgias. J Pak Med Assoc 59: 847-850.
- Schreiber JU, Mencke T, Biedler A, Fürst O, Kleinschmidt S, et al. (2003) Postoperative myalgia after succinylcholine: No evidence for an inflammatory origin. Anesth Analg 96: 1640-1644.
- Spence D, Domen-Herbert R, Boulette E, Olson RL, Olson L, et al. (2002) SDd-HRbE et. A comparison of rocuronium and lidocaine for the prevention of postoperative myalgia after succinylcholine administration. AANA J 70: 367-372
- Pandey CK, Tripathi M, Joshi G, Karna ST, Singh N (2012) Prophylactic use of gabapentin for prevention of succinylcholine-induced fasciculation and myalgia: A randomized, double-blinded, placebo-controlled study. J Postgrad Med 58: 19-22.
- DeWitt L Campbell T, Lynn DeWitt T (2003) A comparison of the differential effects of atracurium and/or A comparison of the differential effects of atracurium and/or lidocaine on succinylcholine-induced postoperative myalgia lidocaine on succinylcholine-induced postoperative myalgia Recommended Citation Recommended Citation.
- Schreiber JU, Lysakowski C, Fuchs-Buder T, Tramèr MR (2006) Prevention of Succinylcholine-Induced Fasciculation and Myalgia. Surv Anesthesiol 50: 198-199.
- Senapati LK, Battini KP, Padhi PP, Samanta P (2021) Effect of Non-depolarizing Muscle Relaxants Rocuronium Versus Vecuronium in the Assessment of Post-Succinylcholine Complications in Surgeries Under General Anesthesia: A Randomized Double-Blind Study at a Tertiary Care Hospital. Cureus 13: e19793.
- Hardik S, Halvadia E (2020) Reduction in the succinylcholine induced myalgia with lidocaine 3: 189-191.
- Findlay GP, Spittal MJ (1996) Rocuronium pretreatment reduces suxamethonium-induced myalgia: Comparison with vecuronium. Br J Anaesth 76: 526-529.
- Pandey AK (2014) Effect of iv Lidocaine in postoperative myalgia treatment.pdf. Vol. 1 VEMS.
- Lee TL, Aw TC (1991) Prevention of succinylcholine-induced myalgia with lidocaine pretreatment. J Anesth 5: 239-246.
Citation: Buli B, Gashew A, Abebe M, Gerbessa B (2022) A Comparison Of Prophylactic Use Of Intravenous Lidocaine Versus Vecuronium In Preventing Suxamethonium - Induced Fasciculation And Postoperative Myalgia Among Surgical Patients At Hawassa University Specialized Hospital, Ethiopia: Prospective Cohort Study. J Anesth Clin Care 9: 075
Copyright: © 2022 Bekele Buli, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

