
Journal of Anesthesia & Clinical Care Category: Clinical
Type: Case Report
A New Approach for Procedural Sedation in Children: The Intramuscular Dextroketamine and Dexmedetomidine Association
*Corresponding Author(s):
Renato Lucas Passos De SouzaHospital Das Clinicas Da Faculdade De Medicina De Ribeirao Preto, USP, HCFMRP-USP, Brazil
Tel:+55 16996367912,
Email:contato@renatolucasmd.com
Received Date: Jun 26, 2019
Accepted Date: Jun 28, 2019
Published Date: Jun 05, 2019
Abstract
Studies show that Dextroketamine combined with Dexmedetomidine allows safe and effective sedation for children in several anesthesia procedures. In this association already recognized in the literature as Ketodex, Ketamine not only balances the sympatholytic effects of Dexmedetomidine, but also attenuates the sialorrhea and undesirable effects caused by ketamine in the central nervous system, with the advantage of no respiratory depression or bronchial hyper reactivity. We present a challenging case of a child with not feasible vascular access, due to multiple punctures and consequently thrombosis of the venous bed, in which the intramuscular Ketodex option was safe, painless and an excellent alternative for sedation.
Keywords
Children; Intramuscularly; Ketodex; Procedural sedation
INTRODUCTION
Invasive and noninvasive procedures remain a common and necessary component in the management of children with acute and chronic diseases. Although procedural sedation is generally safe and effective, patients with underlying co-morbid conditions are at increased risk for complications during and after procedures [1].
Ketamine, an NMDA receptor antagonist, is an effective drug for sedation, analgesia, and amnesia and has been widely used as an alternative to the use of inhalational agents in order to reduce the incidence of Sevoflurane agitation and with the advantage of not causing respiratory depression [2]. Dexmedetomidine, a highly specific alpha-2 agonist, also has sedative, analgesic and anxiolytic effects, without significant respiratory depression at clinical doses [3]. Even used by non-anesthesiologists, Ketamine and dexmedetomidine have been proven safe and effective to ensure successful sedation [4].
Intramuscular route provides rapid systemic action, with near 80% of biodisponibility and plasma concentration peak in about 15 minutes, and is indicated for uncooperative patients or for those who cannot take oral medications. Then, the intramuscular route of both Ketamin and Dexmedetomidine can be an interesting option for procedural sedation in children, usually non-cooperatives, who do not calmly accept the mask for inhaled anesthesia, are agitated or have difficult venous accesses.
We present the use of an intramuscular Ketamine-Dexmedetomidine combination for procedural sedation in a thirteen-year-old child with acute ventriculitis that had to be submitted to a transhepatic central venous access for parenteral antibiotic therapy.
Ketamine, an NMDA receptor antagonist, is an effective drug for sedation, analgesia, and amnesia and has been widely used as an alternative to the use of inhalational agents in order to reduce the incidence of Sevoflurane agitation and with the advantage of not causing respiratory depression [2]. Dexmedetomidine, a highly specific alpha-2 agonist, also has sedative, analgesic and anxiolytic effects, without significant respiratory depression at clinical doses [3]. Even used by non-anesthesiologists, Ketamine and dexmedetomidine have been proven safe and effective to ensure successful sedation [4].
Intramuscular route provides rapid systemic action, with near 80% of biodisponibility and plasma concentration peak in about 15 minutes, and is indicated for uncooperative patients or for those who cannot take oral medications. Then, the intramuscular route of both Ketamin and Dexmedetomidine can be an interesting option for procedural sedation in children, usually non-cooperatives, who do not calmly accept the mask for inhaled anesthesia, are agitated or have difficult venous accesses.
We present the use of an intramuscular Ketamine-Dexmedetomidine combination for procedural sedation in a thirteen-year-old child with acute ventriculitis that had to be submitted to a transhepatic central venous access for parenteral antibiotic therapy.
CASE REPORT
A 13 year old child with post–natal neuropathy, weighing 36 kg and in 8 hours fast was admitted to the Emergency Unit with fever (39oC) and headache and diagnosed with ventriculitis after cranial tomography and lumbar puncture. Urgent antibiotic therapy was mandatory. He presented a history of multiple failures of peripheral and deep venous access (thrombosis of jugular, subclavian and femoral veins) and arrived anxious in the radio intervention room, without tracheostomy, gastrostomy or a venous access. In need of anesthesia, to perform suprahepatic central venous access, guided by ultrasound and radioscopy, it was decided to administer intramuscularly a mixture of Dextroketamine and Dexmedetomidine. Prior local anesthesia was done, with 3 ml of 1% lidocaine, using a 30G 13x4.5 mm needle, in vastus medialis muscle, and a dilution in a 5 ml syringe containing 20 mg/ml Dextroketamine associated with 10 mcg/ml Dexmedetomidine was prepared. We choose to use a dose of 1 mcg/kg Dexmedetomidine associated with 2 mg/kg Dextroketamine (3.6 ml solution) with a 22G needle. In less than 5 minutes, the child was sedated, acquiring state 2 on the Pediatric Sedation State Scale (PSSS) [5] (Figure 1).
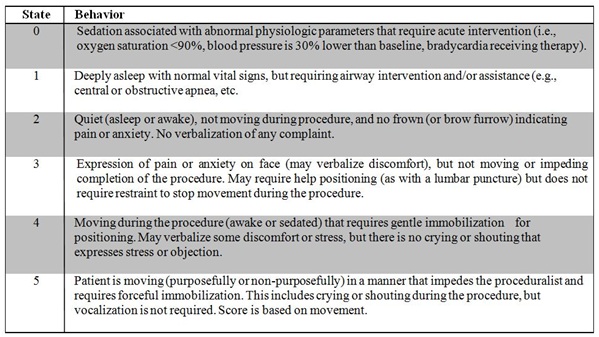 Figure 1: PSSS (Pediatric Sedation State Scale).
Figure 1: PSSS (Pediatric Sedation State Scale).The child did not respond to the infiltration of lidocaine by the radiologist, and remained immobile throughout the process, which lasted 35 minutes (Figure 2). Eupneic, hemodynamically stable, heart rate between 80 and 90 beats per minute, non-invasive arterial pressure ranged from 100x60 to 110x70 mmHg, peripheral oxygen saturation of 98%, supplemental oxygen was not necessary and the procedure was successfully done (Figure 3). The child was referred to the post-anesthetic room and after 20 minutes of spontaneous breathing, was discharged to the room.
 Figure 2: Suprahepatic central venous access, guided by ultrasound and radioscopy.
Figure 2: Suprahepatic central venous access, guided by ultrasound and radioscopy. Figure 3: Suprahepatic vein puncture.
Figure 3: Suprahepatic vein puncture.DISCUSSION
Dexmedetomidine is an alpha-2-adrenergic agonist, which received initial approval from the Food & Drug Administration (FDA) in the United States in 1999, for the sedation of adults during mechanical ventilation and subsequently in 2009 for Monitored Anesthesia Care (MAC) of adults. Despite lacking a specific FDA-approved indication in infants and children, it has been used successfully in several different clinical scenarios including sedation during mechanical ventilation, procedural sedation, postoperative analgesia, prevention of emergence delirium, post anesthesia shivering control, and the treatment of withdrawal from various substances including opioids and benzodiazepines [5].
In our patient anesthetic management, concerns included the need to provide effective sedation to perform a potencial painful procedure without ventilatory or hemodynamic compromise.
The use of ketamine provides several benefits as the provision of analgesia, which is not present dexmedetomidine, an increase in Heart Rate (HR) and Blood Pressure (BP) to offset the bradycardia of dexmedetomidine, and a more rapid onset when compared to dexmedetomidine alone. Dexmedetomidine prevents several of the potentially deleterious effects of ketamine including emergence agitation, excessive salivation, and stimulation of the cardiovascular system (increased HR and BP) [6].
Clinical experience with the combination of dexmedetomidine and ketamine continues to increase showing its efficacy in prospective trials, case series, and isolated case reports [7-11]. However, despite its efficacy as the sole agent for sedation during non-painful radiologic imaging, dexmedetomidine may fail when used as the sole agent for painful procedures [12-14]. In our patient, effective sedation was provided by a single intramuscular dose of ketamine and dexmedetomidine.
Mester et al retrospectively reviewed this combination for sedation during cardiac catheterization in children with heart disease [7]. An intravenous bolus dose of ketamine (2mg/kg) and dexmedetomidine (1mg/kg) was administered over 3 minutes followed by a continuous infusion of dexmedetomidine. No patient reacted to the infiltration of the groin and placement of the arterial and venous cannula. Two patients developed upper airway obstruction resolved with the airway repositioning. No central apnea was noted and the maximum value of PaCo2 was 48 mmHg.
McVey and Tobias described the successful use of dexmedetomidine and ketamine for procedural sedation during lumbar puncture for spinal anesthesia in 12 pediatric patients [8]. The dosing regimen for the ketamine and dexmedetomidine was similar to that reported by Mester et al. Other studies have also shown that the association of ketamine and dexmedetomidine even at low doses, allows safe and effective sedation for children in various surgical procedures [15,16].
Joseph Tobias has consistently demonstrated the utility of dexmedetomidine in conjunction with ketamine for procedures in which a deep level of sedation is required while maintaining spontaneous breathing [16]. Several reports have included patients with significant co-morbid conditions, including pulmonary hypertension, sleep apnea, tracheal compression from a mediastinal mass, congenital heart disease, as well as compromised cardiac and respiratory function. These reports demonstrate that a dexmedetomidine-ketamine combination effectively achieves the desired level of sedation while minimizing the potential for adverse effects. Tobias also concluded that the most effective regimen for procedural sedation seems to be the use of an intravenous bolus dose of both agents, dexmedetomidine (1 μg/kg) and ketamine (1-2 mg/kg), to initiate sedation and, used in such a scenario, the two agents can be co-administered from a single syringe [16].
Due to Ketamine’s unique properties and versatility, it has gained increasing popularity in pre hospital and emergency medicine, throughout the world. When intravenous access is difficult, the use of intramuscular, oral or intranasal ketamine has been described with good effect [17]. Dexmedetomidine can also be used intravenous and intramuscular; the suggested dose for premedication is 0, 33-0, 67 mcg/kg IV or 2, 5 mcg/kg IM, an injection given 15minutes before procedure [18]. Thus, the use of the intramuscular mixture of both drugs would be something natural to happen.
To the best of our knowledge, we have not found publications regarding the use of dexmedetomidine and Dextroketamine by the intramuscular route in humans. There is a publication of a study that associates both drugs intramuscularly in swine, showing the safety of the combination and the efficient sedation [19]. It this case report it was observed that both the association of the drugs in the same syringe and the application intramuscularly in bolus, at the recommended doses, showed to be extremely painless, effective and conferred safety for the accomplishment of a procedure free from agitation, guaranteeing hypnosis, analgesia, preventing hypoventilation or any change in respiratory pattern, being an excellent alternative for sedation in children with co-morbidities. Ketodex is a very versatile mixture in anesthesia practice, finding a place in an increasing number of clinical procedures. We demonstrated that the use of the mixture, intramuscularly in a single syringe is a viable alternative in sedation for surgical procedures in children.
In our patient anesthetic management, concerns included the need to provide effective sedation to perform a potencial painful procedure without ventilatory or hemodynamic compromise.
The use of ketamine provides several benefits as the provision of analgesia, which is not present dexmedetomidine, an increase in Heart Rate (HR) and Blood Pressure (BP) to offset the bradycardia of dexmedetomidine, and a more rapid onset when compared to dexmedetomidine alone. Dexmedetomidine prevents several of the potentially deleterious effects of ketamine including emergence agitation, excessive salivation, and stimulation of the cardiovascular system (increased HR and BP) [6].
Clinical experience with the combination of dexmedetomidine and ketamine continues to increase showing its efficacy in prospective trials, case series, and isolated case reports [7-11]. However, despite its efficacy as the sole agent for sedation during non-painful radiologic imaging, dexmedetomidine may fail when used as the sole agent for painful procedures [12-14]. In our patient, effective sedation was provided by a single intramuscular dose of ketamine and dexmedetomidine.
Mester et al retrospectively reviewed this combination for sedation during cardiac catheterization in children with heart disease [7]. An intravenous bolus dose of ketamine (2mg/kg) and dexmedetomidine (1mg/kg) was administered over 3 minutes followed by a continuous infusion of dexmedetomidine. No patient reacted to the infiltration of the groin and placement of the arterial and venous cannula. Two patients developed upper airway obstruction resolved with the airway repositioning. No central apnea was noted and the maximum value of PaCo2 was 48 mmHg.
McVey and Tobias described the successful use of dexmedetomidine and ketamine for procedural sedation during lumbar puncture for spinal anesthesia in 12 pediatric patients [8]. The dosing regimen for the ketamine and dexmedetomidine was similar to that reported by Mester et al. Other studies have also shown that the association of ketamine and dexmedetomidine even at low doses, allows safe and effective sedation for children in various surgical procedures [15,16].
Joseph Tobias has consistently demonstrated the utility of dexmedetomidine in conjunction with ketamine for procedures in which a deep level of sedation is required while maintaining spontaneous breathing [16]. Several reports have included patients with significant co-morbid conditions, including pulmonary hypertension, sleep apnea, tracheal compression from a mediastinal mass, congenital heart disease, as well as compromised cardiac and respiratory function. These reports demonstrate that a dexmedetomidine-ketamine combination effectively achieves the desired level of sedation while minimizing the potential for adverse effects. Tobias also concluded that the most effective regimen for procedural sedation seems to be the use of an intravenous bolus dose of both agents, dexmedetomidine (1 μg/kg) and ketamine (1-2 mg/kg), to initiate sedation and, used in such a scenario, the two agents can be co-administered from a single syringe [16].
Due to Ketamine’s unique properties and versatility, it has gained increasing popularity in pre hospital and emergency medicine, throughout the world. When intravenous access is difficult, the use of intramuscular, oral or intranasal ketamine has been described with good effect [17]. Dexmedetomidine can also be used intravenous and intramuscular; the suggested dose for premedication is 0, 33-0, 67 mcg/kg IV or 2, 5 mcg/kg IM, an injection given 15minutes before procedure [18]. Thus, the use of the intramuscular mixture of both drugs would be something natural to happen.
To the best of our knowledge, we have not found publications regarding the use of dexmedetomidine and Dextroketamine by the intramuscular route in humans. There is a publication of a study that associates both drugs intramuscularly in swine, showing the safety of the combination and the efficient sedation [19]. It this case report it was observed that both the association of the drugs in the same syringe and the application intramuscularly in bolus, at the recommended doses, showed to be extremely painless, effective and conferred safety for the accomplishment of a procedure free from agitation, guaranteeing hypnosis, analgesia, preventing hypoventilation or any change in respiratory pattern, being an excellent alternative for sedation in children with co-morbidities. Ketodex is a very versatile mixture in anesthesia practice, finding a place in an increasing number of clinical procedures. We demonstrated that the use of the mixture, intramuscularly in a single syringe is a viable alternative in sedation for surgical procedures in children.
CONCLUSION
A single dose of intramuscular Dextroketamine and dexmedetomidine provided effective sedation for transhepatic central venous access in a thirteen-year-old with acute ventriculitis. This combination of agents was chosen, given the absence of venous access and the need to maintain spontaneous ventilation without Sevoflurane agitation and environmental pollution.
Regardless of the agents used for procedural sedation, there is a potential for not only hemodynamic, but also respiratory depression. Given these concerns, appropriate monitoring and access to resuscitation medications plus airway equipment are mandatory during procedural sedation. With these caveats in mind, we believe that the use of combined Dextroketamine and Dexmedetomidine (Ketodex) Intramuscular should be considered as an interesting choice for procedural sedation in children, even with co-morbidities, as it has been proved in the described case and in other clinical scenarios.
Future clinical trials comparing different sedation regimens with other sedatives and routes of administration may provide valid information about safety, time of awakening, and cost effectiveness.
Regardless of the agents used for procedural sedation, there is a potential for not only hemodynamic, but also respiratory depression. Given these concerns, appropriate monitoring and access to resuscitation medications plus airway equipment are mandatory during procedural sedation. With these caveats in mind, we believe that the use of combined Dextroketamine and Dexmedetomidine (Ketodex) Intramuscular should be considered as an interesting choice for procedural sedation in children, even with co-morbidities, as it has been proved in the described case and in other clinical scenarios.
Future clinical trials comparing different sedation regimens with other sedatives and routes of administration may provide valid information about safety, time of awakening, and cost effectiveness.
REFERENCES
- Malviya S, Voepel-Lewis T, Eldevik OP, Rockwell DT, Wong JH, et al. (2000) Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth 84: 743-748.
- Abu-Shahwan I, Chowdary K (2007) Ketamine is effective in decreasing the incidence of emergence agitation in children undergoing dental repair under sevoflurane general anesthesia. Paediatr Anaesth 17: 846-850.
- Kamibayashi T, Maze M (2000) Clinical uses of alpha2-adrenergic agonists. Anesthesiology 93: 1345-1349.
- Corcuera-Flores JR, Silvestre-Rangil J, Cutando-Soriano A, López-Jiménez J (2016) Current methods of sedation in dental patients - a systematic review of the literature. Med Oral Patol Oral Cir Bucal 21: 579-586.
- Cravero JP, Askins N, Sriswasdi P, Tsze DS, Zurakowski D, et al. (2017) Validation of the Pediatric Sedation State Scale. Pediatric 139: 20162897.
- Tobias JD (2007) Dexmedetomidine: applications in pediatric critical care and pediatric anesthesiology. Pediatr Crit Care Med 8: 115-131.
- Levanen J, Makela ML, Scheinin H (1995) Dexmedetomidine premedication attenuates ketamine-induced cardiostimulatory effects and postanesthetic delirium. Anesthesiology 82: 1117-1125.
- Mester R, Easley RB, Brady KM, Chilson K, Tobias JD (2008) Monitored anesthesia care with a combination of ketamine and dexmedetomidine during cardiac catheterization. Am J Ther 15: 24-30.
- McVey JD, Tobias JD (2010) Dexmedetomidine and ketamine for sedation during spinal anesthesia in children. J Clin Anesth 22: 538-545.
- Bozdogan N, Sener M, Caliskan E, Kocum A, Aribogan A (2008) A combination of ketamine and dexmedetomidine sedation with caudal anesthesia during incarcerated inguinal hernia repair in three high-risk infants. Pediatr Anesth 18: 1009-1011.
- Barton KP, Munoz R, Morell VO, Chrysostomou C (2008) Dexmedetomidine as the primary sedative during invasive procedures in infants and toddlers with congenital heart disease. Pediatr Criti Care Med 9: 612-615.
- Luscri N, Tobias JD (2006) Monitored anesthesia care with a combination of ketamine and dexmedetomidine during magnetic resonance imaging in three children with trisomy 21 and obstructive sleep apnea. Peadiatr Anaesth 16: 782-786.
- Mason KP, Zurakowski D, Zgleszewski SE, Robson CD, Carrier M, et al. (2008) High dose dexmedetomidine as the sole sedative for pediatric MRI. Paediatr Anaesth18 :403-411.
- Tobias JD, Berkenbosch JW (2002) Initial experience with dexmedetomidine in paediatric-aged patients. Paediatr Anaesth 12: 171-175.
- Jalowiecki P, Rudner R, Gonciarz M, Kawecki P, Petelenz M, et al. (2005) Sole use of dexmedetomidine has limited utility for conscious sedation during outpatient colonoscopy. Anesthesiology 103: 269-273.
- Goyal R, Singh S, Shukla RN, Patra AK, Bhargava DV (2013) Ketodex a combination of dexmedetomidine and ketamine for upper gastrointestinal endoscopy in children: a preliminar report. J Anesth 27: 461-463.
- Tobias JD (2012) Dexmedetomidine and ketamine: an effective alternative for procedural sedation. Pediatr Crit Care Med 13: 423-427.
- Gales A, Maxwell S (2018) Ketamine: Recent Evidence and Current Uses. ATOTW 381: 1-7.
- Naaz S, Ozair E (2014) Dexmedetomidine in Current Anaesthesia Practice-A review. J Clin Diagn Res 8: 01-04.
- Santos M, Bertrán de Lis BT, Tendillo FJ (2016) Effects of intramuscular dexmedetomidine in combination with ketamine or alfaxalone in swine. Vet Anaesth Analg 43: 81-85.
Citation: Lucas RPS, Paula-Garcia WN, Melo WAL, Garcia LV, Klamt JG, et al. (2019) A New Approach for Procedural Sedation in Children: The Intramuscular Dextroketamine and Dexmedetomidine Association. J Anesth Clin Care 6: 38.
Copyright: © 2019 Renato Lucas Passos de Souza, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!

