
Anesthesia with Peribulbar Block: Lidocaine-Bupivacaine vs Lidocaine-Bupivacaine-Fentanyl
*Corresponding Author(s):
Leopoldo WulffAnesthesiologists Staff, Ambulatory Surgery Unit, Centro Médico Docente La Trinidad, Caracas, Venezuela
Tel:+58 4143264549,
Email:leowulff@yahoo.com
Abstract
Introduction: Ophthalmological procedures such as cataract extraction can be carried out with a Peribulbar Block (PBB). The advantages of this anesthetic technique include a lower incidence of coughing, unwanted movements and emesis during awakening, in addition to providing adequate postoperative analgesia.
We observed that the use of fentanyl citrate by peribulbar route, when administered with a local anesthetic, shortens the anesthetic latency, does not interfere with the degree of akinesia and provides greater postoperative analgesia. The combined use of local anesthetics and fentanyl citrate in ophthalmic surgery offers great benefits for the patient, also allowing the surgeon an adequate surgical field. We observed in ophthalmic surgery with regional anesthesia that the peribulbar use of fentanyl citrate is an alternative that provides a greater intraoperative and postoperative analgesia when combined with local anesthetics.
Objective: Demonstrate that the lidocaine-bupivacaine-fentanyl combination is better than the lidocaine-bupivacaine combination, since the former shortens the latency time of Peribulbar Block (PBB), produces the same degree of akinesia of the eyeball and provides longer postoperative analgesia time.
Material and Methods: A total of 70 patients from the Ophthalmology Service of the Centro Docente La Trinidad were studied. Patients with physical condition ASA I and II electively programmed for Extracapsular Cataract Extraction (ECCE) under Peribulbar Block (PBB) were included. They were randomly divided into 2 groups of 35 patients each. The Blood Pressure (BP), Heart Rate (HR), Respiratory Frequency (RF) and O2 saturation (SpO2) were monitored at the time of surgery. A Peribulbar Block (PBB) was performed in both groups. Group 1 (LB) received 100 mg of lidocaine 5% and 15 mg of bupivacaine 0.5% for a total volume of the anesthetic mixture of 5 ml. while group 2 (LBF) received 100 mg of lidocaine 5%, 15 mg of 0.5% bupivacaine and 50 mcg of fentanyl citrate for a total volume of the anesthetic mixture of 6 ml. Completed the Peribulbar Block (PBB) the latency time, the reached degree of ocular akinesia was measured and postoperative analgesia evaluated.
Results: There were no statistically significant differences with respect to age in both groups. Among the pathologies added to each of the groups under treatment, in Group I (LB) Diabetes Mellitus was present in 12 patients (34.2%), while in Group II (LBF) was found in 8 patients (22.8%). High Blood Pressure (HBP) was present in 15 patients (42.8%) of group I (LB) while in group II (LBF) there were 18 patients (51.4%). Regarding the latency period, statistically significant differences were observed since group I (LB) had a greater average time of 3.17 ± 1.09 minutes and group II (LBF) an average time of 1.82 ± 0.66 minutes (t = 6.19 and p = 0.0001). There were no statistically significant differences in the degree of ocular akinesia achieved by both groups. Likewise, group II (LBF) had better postoperative analgesia. In group I (LB) there was mild conjunctival chemosis and residual hematoma in 3 patients, whereas in group II (LBF) there was mild conjunctival chemosis and residual hematoma in 1 patient.
Conclusion: The use of fentanyl citrate peribulbar shortens the latency time, does not interfere with the degree of ocular akinesia and provides better postoperative analgesia, so this combination of anesthetics may be a good alternative for cataract ophthalmic surgery under regional anesthesia.
Keywords
SCIENTIFIC BACKGROUND
In the daily practice of ophthalmologic surgery, locoregional anesthesia is predominantly used for cataract surgery. The use of retrobulbar lidocaine was first described in 1885 by Herman Knapp [1] to perform the enucleation of a patient wounded in war; is not until the mid-1950 [2] when retrobulbar block is popularized.
The practice of ophthalmological surgery has gained followers and in recent years ophthalmological surgery interventions such as cataract extraction, lacrimal duct surgeries, correction of strabismus, radial keratotomy, etc., are more frequently done thanks to the emergence of new drugs, sedatives, anesthetics and analgesics of shorter duration, as well as the development of new surgical techniques together with the rebirth of locoregional anesthesia techniques [3]. Many of the ophthalmological procedures derived in surgery are in patients suffering from systemic diseases, angina, COPD, Parkinson’s, arthritis [2,4,5] etc., so it is essential to perform a preoperative evaluation whose main objective is to reduce the surgical risk and the perioperative morbidity and adjust the anesthetic plan to the conditions of each of the patients [5,6].
Among the great variety of drugs used for peribulbar block we can mention the combination of lidocaine and bupivacaine with or without vasoconstrictor (epinephrine). Ropivacaine has been popularized with excellent results. Other drugs, such as hyaluronidase, have been added to these combinations to prolong the effect and improve its diffusion and of the narcotics having in mind the receptors shared by the eyeball and the peripheral nervous system, hoping that the effect is similar to when the narcotic is used epidural [7-9] to shorten the latency time of the local anesthetic, increase its analgesic potency and provide a certain degree of postoperative analgesia.
Peribulbar anesthesia offers periorbital anesthesia, of the eyeball and ocular conjunctiva, ocular hypotonia, akinesia of the ocular muscles and an acceptable level of sedation to the patient [10].
It is evident that the first five points depend fundamentally on the anesthetic technique where an adequate balance between the concentration and the volume of the local anesthetics used is necessary. There must be a balance between the anesthetic quality that is provided with the peribulbar block and the level of sedation, since when there is not a good quality of ocular block, it is necessary to use anxiolytics such as benzodiazepines that induce a decrease in oxygen saturation, increase in PaCO2 that can result in respiratory depression [11]; it is important to remember that 95% of patients admitted for cataract surgery are senile [2,5,6,11] with lower tolerance to medications. From the above we can conclude that it is vital to achieve an anesthetic quality with peribulbar block that can be facilitated when adding to the local anesthetic a narcotic.
There are studies that support the use of narcotic in the epidural, retrobulbar and/or peribulbar space [8,9] and by this, shorten the latency period providing a better anesthetic quality for cataract surgery decreasing the requirements of narcotics and endovenous anxiolytics. With this, the incidence of complications due to oversedation shall be lower in senile patients in whom we do not have immediate airway access because their faces are covered and the only support provided is supplemental oxygen through nasal tips. The incidence of oversedation reported in the literature that warrants orotracheal intubation during the operative period of cataract surgery is 85% with the risks implied by urgent orotracheal intubation as well as any maneuver with the eyeball open [12].
Retrobulbar block is one of the most used anesthetic techniques in recent years but complications such as blindness due to optic nerve injury, accidental eye perforation, retinal detachment, retrobulbar hemorrhage, respiratory depression, CNS depression, arterial and venous thrombosis and venous [5,13-17] have been reported. With high spinal anesthesia, it has been described loss of consciousness and cardio respiratory failure [16,18,19]. That is why the technique that causes the lowest complication rate and used by us in the study was peribulbar blockade [19]. Finally, it is necessary to obtain absolute tranquility in the postoperative period, especially in the elderly, since in them the pain can cause a state of agitation that can endanger the result of the intervention [20-22].
MATERIAL AND METHODS
Three different types of analysis will be used. The first is the descriptive analysis in which position measurements are calculated. The second is the graphic analysis, the same is based on bar graphs, sector diagrams, frequency histograms; the third analysis is that of statistical significance or validation where parametric and non-parametric statistics are proposed, as the case may be. All hypothesis tests will be carried out with α = 0.05, that is, 95% confidence. The contrasts will be significant when p < 0.05.
All patients scheduled for cataract surgery who received anesthetic treatment under peribulbar blocking technique were studied. The study was conducted in the Ambulatory Surgery unit of the Centro Médico Docente La Trinidad, during the period between October and November 2009. We included 70 random elective patients scheduled for Cataract Extracapsular Extraction (CEE) with indication of regional anesthesia with peribulbar block and physical status ASA I and II, between 45 and under 90 years of age. Those patients who reported being allergic to amide-type anesthetics and fentanyl citrate, patients with a history of woody thorax and patients with uncompensated systemic diseases (DM, HAS) were not included. We excluded patients in whom it was necessary to change the anesthetic technique due to insufficient analgesia or those in which the administration of intravenous analgesics was required during the operative period.
Group I (cases) composed of 35 patients were subjected to peribulbar block with Lidocaine-Bupivacaine (group LB) and group II (controls) designated experimental group composed of 35 patients who received peribulbar block with Lidocaine Bupivacaine Fentanyl (group LBF). Patients were monitored with Blood Pressure, Heart Rate, Respiratory Rate and Partial Oxygen Saturation (BP, HR, RR, and SpO2). All patients were medicated with intravenous midazolam with a dose at the discretion of the anesthesiologist. The peribulbar block was placed with 25 G 5/8 needle. Group I received a mixture of 100 mg of lidocaine and 15 mg of 0.5% bupivacaine for a total volume of 5 ml. Group II received a mixture of 100 mg of lidocaine, 15 mg of 0.5% bupivacaine and 50 mcg of fentanyl citrate for a total volume of 6 ml. Latency was evaluated by touching the conjunctiva with a sterile swab taking the time when the corneal reflex was lost.
The akinesia achieved was evaluated until the moment previous to surgery began (Grade I-total akinesia, grade II- limited eye movements, and grade III- preserved eye movements). Postoperative analgesia was evaluated by means of the analogous visual scale at the end of the surgery, and the time elapsed from the end of the surgery until the patient reported discomfort for the first time after discharge was recorded. At that time, an analgesic was prescribed orally.
RESULTS
We studied 70 patients divided randomly into two groups, applying peribulbar block with Lidocaine-Bupivacaine (LB group) and Lidocaine-Bupivacaine-Fentanyl citrate (LBF group), both composed of 35 patients.
The average age for group I was 62.57 ± 7.89 years and for group II it was 64.48 ± 6.92 years. No statistically significant differences were observed (t = 0.327 and p = 0.721).
In group I that received LB, 92% of patients were classified as ASA II and 8% as ASA I; group II that received LBF the patients were classified 7% ASA I and 93% ASA II (Table 1).
|
Variables |
Group |
Descriptive Statistic |
P Value |
|
Age |
LB |
62.57 ± 7.89 |
NS |
|
LBF |
64.48 ± 6.92 |
||
|
ASA |
LB |
8% ASA I y 92% ASA II |
NS |
|
LBF |
7% ASA I y 93% ASA II |
Table 1: General characteristics.Expressed In means value and percentage frequency.
Among the pathologies associated with each of the treatment groups, in the LB group was DM in 12 patients (34.2%) while in the LBF group DM in 8 patients (22.8%). Likewise, in the LB group hypertension (HBP) was present in 15 patients (42.8%) while in the LBF group the war present in 18 patients (51.4%) (Graph 1).
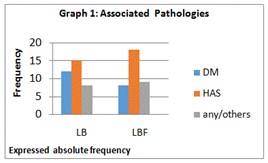
Graph 1: Associated pathologies.
With regard to the latency period, statistically significant differences were observed since the LB group had an average time greater than 4.18 ± 1.14 minutes than the LBF group with 2.06 ± 0.82 minutes (t = 6.38 and p = 0.0001) (Graph 2).
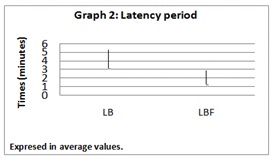
Graph 2: Latency period
In relation to the degree of akinesia, both groups achieved a grade II without finding significant differences for the group LB (Q25 = 2, Md = 2 and Q75 = 2), group LBF (Q25 = 1, Md = 2 and Q75 = 2), Mann-Whitney U = 491 and p = 0.100.
Regarding complications, they were presented in 3 patients (8.5%) of group I (LB) with mild conjunctival chemosis and residual hematoma while in group II (LBF) 1 patient (2.8%) had the same complication (Graph 3).
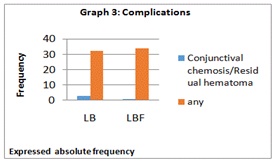
Graph 3: Complications.
There was better control of postoperative pain with the LBF combination compared to the group that only received peribulbar LB. Valuation that was performed using the visual analogue scale (Graph 4).
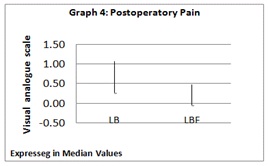
Graph 4: Postoperatory pain.
Once discharged from the ambulatory center, for both groups we prescribed acetaminophen 500 mg orally for the control of postoperative pain which the patients described as “eye discomfort”.
DISCUSSION
Anesthetic treatment can contribute to the success or failure of ophthalmologic surgery. Gild et al., in one study found that 30% of eye injury complaints associated with anesthesia was caused by movements of the patient during ophthalmologic surgery. Clinical strategies to guarantee the immobility of the patient during eye surgery are essential.
In ophthalmological procedures such as cataract extraction or anterior chamber surgery among others can be carried out with a peribulbar block. The cooperation of the patient is very important for the success of this technique. The advantages of peribulbar block include a lower incidence of cough, effort and emesis during the immediate postoperative period. This technique is useful for patients who are to stay for a short time in the hospital area; also provides adequate postoperative analgesia.
With this study, we observed that the use of fentanyl citrate peribulbar, when administered with a local anesthetic, shortens the latency of the anesthetic, does not interfere with the degree of akinesia and provides greater postoperative analgesia, due to its characteristics which include high liposolubility, rapid onset of action, moderate duration of 1.5 to 3.0 hours and reduced incidence of adverse effects; its combined use with local anesthetics in ophthalmologic surgery offers great benefits to the patient as allowing the surgeon a suitable surgical field.
The patients showed only discomfort in both the LB and LBF groups in the postoperative period, that is, after the outpatient center was discharged and acetaminophen was prescribed 1 tablet 500 mg orally.
Opioid analgesics have long been the treatment of choice along with other medications for postoperative pain. It is essential that the route of administration and dosage be planned to control pain quickly and safely.
Peribulbar blockade provides excellent intraoperative and immediate postoperative analgesia, which is why we recommend the use of fentanyl in combination with local anesthetics for regional anesthesia in ophthalmic surgery.
CONCLUSION
We observed that peribulbar use of the combination of Lidocaine-Bupivacaine-Fentanyl (LBF) significantly shortened the latency time compared to the combination Lidocaine-Bupivacaine (LB) not interfering with the degree of akinesia of the eyeball and also providing a longer postoperative analgesia.
REFERENCES
- Hamilton RC (1995) Techniques of orbital regional anaesthesia. Br J Anaesth 75: 88-92.
- Donlow JV (1988) Anesthesia for Ophthalmic Surgery. In: Barash P (ed.). ASA Refresher Course Lectures, JB Lippincott, Philadelphia, USA. 16: 81.
- Carrasco-Jiménez MS, Pestaña C, Rodríguez H, White PF (1997) Ambulatory anesthesia and surgery in Spain and Portugal. Saunders, WB, London. Pg no: 735-739.
- Donlow JV (1994) Anesthesia for eyes, nose, ear and throat surgery. In: Miller RD (ed.). Anestesia 4ª (Vol 2). Churchil Livigstone Inc., New York, USA. Pg no: 2175-2196.
- Pastor JC (1990) Anesthesia in ophthalmology/JC Pastor Jimeno; with the collaboration \\\ on A. García Layana, JI Gómez Herreras. Catalog of the CAO Library 75.
- González JL, Toro MJ. (1996) Evaluación preoperatoría. In: Machado G (ed.). Premedicación y profilaxis en anestesiología. Roche, Barcelona, Spain. Pg no: 17-30.
- Nathan N, Benrhaiem M, Lotfi H, Debord J, Rigaud G, et al. (1996) The role of hyaluronidase on lidocaine and bupivacaine pharmacokinetics after peribulbar blockade. Anesth Analg 82: 1060-1064.
- Barr J, Kirkpatrick N, Dick A, Leonard L, Hawksworth G, et al. (1995) Effects of adrenaline and hyaluronidase on plasma concentrations of lidocaine and bupivacaine after peribulbar anaesthesia. Br J Anaesth 75: 692-697.
- Ready LB, Loper KA, Nessly M, Wild L (1991) Postoperative epidural morphine is safe on surgical wards. Anesthesiology 75: 452-456.
- Kumar CM, Fanning GL. (2002) Orbital regional anesthesia. In: Kumar CM, Dodds C, Fanning GL, (eds.). Ophthalmic anaesthesia. Swets and Zeitlinger, Netherlands. Pg no: 61-88.
- Barash PG (1993) Clinical Anesthesia. In: Cullen BF, Stoelting RK (eds.). Macgrawhill Interamericana, Colombia. Pg no: 418- 423.
- Miller DR (1997) Anestesia. In: Cuchiara F, Miler E Jr., Reves J, Savarese JJ (eds.). Limpergraff, España, Spain. 2: 947-952.
- McGoldrick KE (1995) Challenges in anesthesia for ophthalmic surgery. ASA Annual Refresher Corse Lectures. October 21-25, 172.
- Ramírez-Sánchez A, Palacio MA, García-Sánchez MJ, Imaz Torres MS, Galdo JR, et al. (1993) [Propofol and retrobulbar anesthesia for cataract extraction]. Rev Esp Anestesiol Reanim 40: 307-309.
- Gurtubay JM, Obregozo J, Del Val E, Intxaurraga K, Martínez A (1994) Topical local anestesia and sedation during cataract surgery. The International Monitorition Regional Anestesia (resumen Issue) 203.
- Manrique J, Carmona J, Escarpa A, Vaquero M (1994) Anestesia espinal alta: una complicación poco frecuente del bloqueo retrobulbar. Rev Esp Anestesiol Reanim 33: 199.
- Kumar CM, Dowd TC (2006) Complications of ophthalmic regional blocks: their treatment and prevention. Ophthalmologica 220: 73-82.
- Voyd BF (1993) Atlas de cirugía ocular World Atlas Series (Vol 1). Highlights of Ophtalmology, Panama, 39.
- Ripatt J, Lefrant JY, de La Coussaye JE, Prat-Pradal D, Vivien B, et al. (2001) Peribulbar versus retrobulbar anesthesia for ophthalmic surgery: an anatomical comparison of extraconal and intraconal injections. Anesthesiology 94: 56-62.
- García Guasch R, Doria Martínez de Salinas AM (1984) Anestesia en la cirugía de la catarata. Rev Esp Anestesio Reanim 31: 129.
- Friedman DS, Reeves SW, Bass EB, Lubomski LH, Fleisher LA, et al. (2004) Patient preferences for anaesthesia management during cataract surgery. Br J Ophthalmol 88: 333-335.
- Tan CS, Au Eong KG, Kumar CM (2005) Visual experiences during cataract surgery: what anaethesia providers should know. Eur J Anaesthesiol 22: 413-419.
Citation: Wulff L, Salazar A, Villegas T, Alfonzo A, Fuentes A (2018) Anesthesia with Peribulbar Block: Lidocaine-Bupivacaine vs Lidocaine-Bupivacaine-Fentanyl. J Anesth Clin Care 5: 29
Copyright: © 2018 Leopoldo Wulff, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

