
Bone Marrow Aspirate for Delayed Union due to Severe Thoracic Rib Trauma
*Corresponding Author(s):
Gabriel Silva SantosBiomedical Scientist, IOC – Instituto Do Osso E Da Cartilagem / The Bone And Cartilage Institute 1386 Presidente Kennedy Avenue – 2nd Floor, Room #29 – Zip Code 13334-170, Indaiatuba – São Paulo, Brazil
Tel:+55 1930174366/19989283863,
Email:gabriel1_silva@hotmail.com
Abstract
Study Design: Case report
Objectives: The objective is report a case of delayed union due to severe thoracic rib trauma involving multiple fractures by evaluation, interventional strategy and follow-up.
Background: Delayed union due to severe trauma is an impactful condition responsible for progressive deformity and pain where surgical intervention may still prove to be challenging in terms of success rates. Rib fracture is the most common form of blunt thoracic injury, affecting multiple costal structures in all types of thoracic trauma. Typical conservative treatments are usually limited to brace application and only for the control of pain in acute circumstances. Rib fracture is still an important communicator of trauma severity, as morbidity and mortality can increase according to the number of fractured ribs.
Materials and Methods: Computed tomography (CT) of the costal arches was performed in both diagnosis and follow-up. The patient received Bone Marrow Aspirate (BMA) infiltration treatment to treat the delayed union of fractured bones.
Results: All of the fractured ribs (from the 2nd to the 12th) with multiple affected regions were apparently consolidated. The bone overlaps on the 5th, 6th, 7th, 8th, 9th and 10th ribs, were also consolidated. There was no evidence of chest wall collapse or instability, and there was no evidence of anomalous joints or even pseudoarthrosis. The sternum showed no evidence of abnormalities. Patient exhibited significant pain improvement with BMA treatment.
Conclusion: In this peculiar setting, the infiltrations with BMA proved to be an efficient alternative tool for the treatment of severe thoracic rib trauma and delayed union. The patient returned with no complaints and CT evidence indicated that all of the fractured ribs had complete consolidation. Pain and functional outcome of the chest wall in terms of stability improved with the help of this orthobiologic alternative.
Keywords
Bone marrow aspirate; Delayed union; Fracture; Orthobiologics; Thoracic trauma
Key Points
- A 48-year-old man with a history of epilepsy fell off the roof of his house and suffered severe thoracic trauma, multiple rib fractures on the right rib cage, from the 2nd to the 12th ribs, affecting multiple points in the same costal arch.
- The condition was also associated with hemopneumothorax and unstable chest, as of September 2019. Signs of pain were detected in the right hemithorax. After 3 months, with no sign of consolidation of these fractures (Figure 1) a conclusion was found, characterizing it as possible pseudoarthrosis.
- The patient was submitted to two sessions of BMA injections for the management of delayed union. The first session occurred in February 2020, and the second one in June 2020.
- Delayed union was significantly improved with just two sessions with BMA administration. Three months after the first infiltration procedure the patient returned to the office and showed expressive improvements in pain and significant consolidation of fractured areas.
Introduction
The ribs are vital structures of the thoracic cage. Rib trauma can affect the lungs, mediastinum and other thoracoabdominal structures that rely on the integrity of the ribs for adequate protection [1]. Thoracic traumas usually arise from blunt or penetrating forces and can be broadly classified as chest wall, pulmonary or cardiovascular injury. Rib fractures are the most common form of blunt thoracic injuries affecting multiple points of these structures in all types of thoracic trauma [2]. Depending on the severity of traumatic rib injuries, key complications can encompass acute pain, hemothorax, pneumothorax, extrapleural hematoma, acute vascular injury and pulmonary contusion and laceration. Conservative management strategies are mostly limited to pain attenuation, prevention of further life-threatening complications such as damage to vital thoracoabdominal organs, and stabilization of post-traumatic deformity [1]. The importance of adequately diagnosing and managing thoracic trauma lies in the fact that rib fractures reflect trauma severity in a way that morbidity and mortality increase in equal proportion to the number of fractured ribs [3]. Therefore, the medical expert must be able to accurately identify and report the imaging findings, adding value to the care of patients with thoracic trauma.
There are many studies in the literature which review BMA as a feasible orthobiologic due to its regenerative potential, especially when it comes to the treatment of musculoskeletal disorders. BMA is known to contain Mesenchymal Stem Cells (MSC) and Hematopoietic Stem Cells (HSC), the two major adult stem cell types present in this tissue [4]. These specialized cells secrete a wide variety of cytokines and growth factors which allow them to modulate neighboring cells via paracrine signaling effects. Additionally, they are also highly appreciated for their capacity to renew themselves and differentiate into specific mature cell lineages, which further enhance tissue repair mechanisms [4].
Here, we present the administration of bone marrow aspirate as a feasible orthobiologic alternative in a case of delayed union due to severe thoracic rib trauma with multiple fractures. To our knowledge, this is the first case report that utilizes this specific treatment for such orthopedic conditions.
Materials And Methods
A 48-year-old man with a history epilepsy arrived at the emergency department after losing consciousness and falling off a house roof on his back. He expressed a lot of complaints about excruciating pain which was intensified in the right hemithorax. Immediate physical examination revealed severe thoracic trauma due to multiple fractured ribs (from the 2nd to the 12th) affecting more than one area in the same costal arch. The condition was also associated with hemopneumothorax and unstable chest wall.
No signs of consolidation of these fractures were detected 3 months after the sequence of events (Figure 1) which led us to characterize the condition as possible pseudoarthrosis. Two thoracic surgery teams ruled out surgical treatment, prolonging length of hospital stay. The patient was then referred to our medical services for evaluation, 4 months after trauma. We then decided to attempt treatment with BMA. An anticipated blood panel (Table 1) was also requested to rule out any other lurking variables which could have influenced the patient’s condition.
 Figure 1: CT scans show evidence of rib fracture non-union.
Figure 1: CT scans show evidence of rib fracture non-union.
|
Biomarker |
Value |
|
Erythrocytes (x106/mm3) |
5,470,000 |
|
Hemoglobin (g/dL) |
17 |
|
Leukocytes (%) Total Leukocyte number (x103/mm3) |
50.6 3,600 |
|
Platelets (x103/µL) |
212,000 |
|
Hemosedimentation Speed (mm/hour) |
4 |
|
Rheumatoid Factor |
Negative |
|
Amylase (IU/L) |
60 |
|
C-reactive Protein (mg/L) |
3 |
|
Glucose (mg/dL) |
74 |
|
Urea (mg/dL) |
30 |
|
Creatinine (mg/dL) |
0.93 |
|
Uric Acid (mg/dL) |
5.8 |
|
Glutamic Oxaloacetic Transaminase (IU/L) |
16 |
|
Glutamic Pyruvate Transaminase (IU/L) |
20 |
|
Gamma-glutamyl Transferase (IU/L) |
58 |
|
Prothrombin Time (%) |
100% |
|
International Normalized Ratio |
1.0 |
|
Activated Partial Thromboplastin Time (seconds) |
28 |
|
Creatine Phosphokinase (IU/L) |
195 |
|
Vitamin D (ng/mL) |
46.3 |
|
Carcinoembryonic Antigen (ng/mL) |
0.81 |
|
Cortisol (µg/dL) |
7.8 |
|
Antinuclear Antibody |
Negative |
|
Ferritin (µg/L) |
73.2 |
|
Folic Acid (ng/mL) |
7.97 |
|
Glycated Hemoglobin (%) |
5.2% |
|
Estimated Average Glucose (mg/dL) |
103 |
|
Homocysteine (µmol/L) |
12.02 |
|
Insulin (µIU/mL) |
3.7 |
|
Free Thyroxine (ng/dL) |
0.64 |
|
Vitamin C (mg/L) |
6.2 |
|
Thyroid-stimulating Hormone (µIU/mL) |
1.03 |
|
Vitamin B12 (pg/mL) |
311 |
Table 1: Blood analysis results.
Utilizing a 20 mL syringe, BMA was collected from the posterior iliac crest. The syringe was repositioned after every 5 mL in order to penetrate the deeper layers of bone to collect higher quantities of cells, totaling a volume of 40 mL per session. Each of the target points displaying signs of delayed union received one injection of 3 mL of BMA.
Results
Blood panel (Table 1) showed no alarming irregularities. Therefore we were able to rule out any lurking variables that could have affected the patient’s condition propose any potential contraindications to the treatment with BMA.
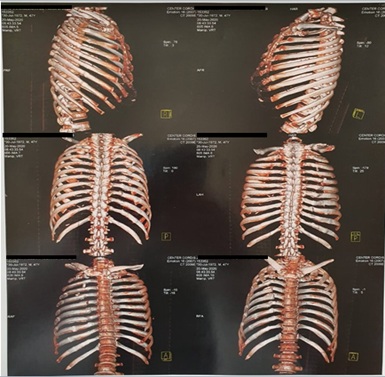 Figure 2: CT scans taken three months after first session of BMA infiltration showing partial fracture consolidation.
Figure 2: CT scans taken three months after first session of BMA infiltration showing partial fracture consolidation.
A new round of CT scans (Figure 2) was taken on 2020-05-20, precisely3 months after the first session of BMA infiltration. The patient expressed positive behavior, reporting significant improvements in nociception. The CT scans (Figure 2) indicate that, although still present, the majority of fractures show signs of consolidation, including the right clavicle. This is observation is less significant in some of the posterior arches on the right, more specifically the regions corresponding to the 6th and 7th arches. Additional observations include multiple pulmonary granulomas and subtle degenerative alterations in the manubriosternal joint and dorsal and inferior cervical spine. Degenerative alterations in the right acromioclavicular joint were also detected along with the presence of subchondral cysts.
The patient was then submitted to a second procedure with BMA infiltration for the 6th and 7th costal arches as well as the right acromioclavicular and manubriosternal joints, specifically. This procedure took place in June 2020, one month after the CT scans from figure 2, and new CT scans were scheduled for October 2020 (Figure 3).
 Figure 3: CT scans showing fracture consolidation.
Figure 3: CT scans showing fracture consolidation.
The patient returned to our office on 2020-11-25 expressing no complaints whatsoever. The CT scans (Figure 3) taken on 2020-10-13 indicate that the fractures which affected multiple areas of the 2nd to the 12th costal arches were all visibly consolidated. The bone overlaps on the 5th, 6th, 7th, 8th, 9th and 10th ribs also showed consolidation. There was no evidence of chest wall collapse or instability, ruling out evidence of anomalous joints or even pseudoarthrosis. The sternum showed no evidence of abnormalities. Overall, the patient exhibited significant improvements in pain and functional outcomes.
Discussion
Delayed union of bones after fracture is a painful and debilitating condition that significantly impacts an individual’s wellbeing, aggravating morbidity and decreasing quality of life. The global prevalence of this condition is estimated to be of approximately 9 million annually and the majority of therapeutic interventions still have quite limited effects [5]. This ultimately generates additional challenges such as prolonged pain, reduced physical capacity and financial burden [5]. More specifically in the case of ribs, which are frequently affected by penetrating or blunt force trauma, it is important for the medical expert to accurately identify specific features in order to prevent injuries of vital organs and acute rib trauma complications [1].
Rib injuries are usually subdivided into morphological fracture patterns which are classified as buckle, displaced/nondisplaced, segmental, stress or pathologic [1]. Regardless of classification, rib fractures are still a major problem as they are significantly associated with morbidity and mortality, both of which increase in equal proportion to the number of fractured ribs [6]. Elaborating further, patients with isolated rib fractures, for instance, should be hospitalized if three or more of these structures are affected; elderly patients with six or more fractures should be taken to intensive care units as morbidity and mortality increase even further [6]. The typical complications following such traumatic events include acute pain, hemothorax, pneumothorax, extrapleural hematoma, acute vascular injury and pulmonary contusion and laceration, all of which can make the patient more susceptible to injuries of the abdominal organs [7,8].
In healthy patients, bone fractures do not usually take an extended amount of time to show signs of healing. Our patient was only 48 years old when he suffered the accident and, based on the blood panel, no irregularities associated with health issues were detected. However, in 3 months there were no evident signs of fracture consolidation and since there is no classification or consensus regarding pseudoarthrosis of rib bones, specifically, it is possible to consider the condition as probable pseudoarthrosis.
As mentioned earlier in this manuscript, the conventional methods of rib fracture management are usually limited to pain alleviation, prevention of further complications and stabilization of posttraumatic deformity [1]. However, severe thoracic rib trauma-associated delayed union as well as pseudoarthrosis still proves to be a complicated condition which diminishes the patient’s quality of life significantly. For such reasons, it may therefore require additional efficacious interventional strategies such as the administration of orthobiologics. By definition, orthobiologics are products that can rapidly enhance the healing process of orthopedic injuries [4]. BMA, for example, is being widely applied towards a variety of diseases and has shown great promise as a powerful regenerative medicine tool so far, especially in musculoskeletal conditions. There is a significant lack of studies in the literature which specifically evaluate the effects of BMA for thoracic trauma, even more so in circumstances similar to the ones discussed in this case report. To our knowledge, this is the first case report that specifically utilizes BMA for the treatment of delayed union due to severe thoracic rib trauma with multiple fractures.
As previously introduced, the bone marrow is known to carry a rich diversity of cellular and molecular components, especially the substances secreted by resident cells [4]. The MSCs found in BMA are able to perform self-renewal and differentiation into mesodermal linage cells such as bone, cartilage, muscle, fat, meniscus and tendon, which is a fundamental attribute in regenerative medicine [4]. In addition, MSCs also elicit paracrine effects, being able to manipulate their local microenvironment. These cells are highly advantageous since they do not appear to trigger aggressive immunogenic episodes and can be easily isolated, which therefore enables allogenic transplantation procedures, if necessary. In such circumstances, these cells should be considered immune evasive [4]. However, the effects of MSCs in cellular-based therapies are mostly attributed to their homing and engraftment abilities into target tissues. MSCs appear to have a rather short life span, being ultimately phagocytized by monocytes and subsequently stimulating the production of T-regulatory cells, which may significantly contribute to the overall clinical improvement [4]. Whenever tissue injury occurs, local cells secrete chemokines which result in MSC recruitment. MSCs in turn respond by releasing key agents such as Vascular Endothelial Growth Factor (VEGF), Transforming Growth Factor Beta (TGF-β), Stromal-Derived Factor 1 (SDF-1) and Stem Cell Factor (SCF), among others. These proteins promote allow MSCs to modulate the wound-healing cascade, halt apoptosis and fibrosis, alleviate autocrine the inflammatory process and stimulate cell proliferation and differentiation via paracrine and pathways [4]. Additionally, researchers have also explored the roles of Interleukin-1 Receptor Antagonist (IL-1RA), an important cytokine present in bone marrow-derived products. This protein is a competitive antagonist that binds to IL-1B and IL-1a isoforms on cell surface receptors and shuts down IL-1-induced inflammatory effects and catabolic reactions [4]. This would explain why our patient exhibited significant improvements in pain. IL-1Ra has the potential to attenuate matrix degradation since IL-1B reportedly promotes Matrix Metalloproteinase (MMP)3 and Tumor Necrosis Factor (TNF) alpha gene expression, prostaglandin E2 (PGE2) secretion, chondrocyte apoptosis and inhibition of collagen deposition [4]. In the specific case of fractures, these effects prove to be essential in order to achieve successful fusion of bones.
BMA application procedures are highly recommended for the treatment of specific musculoskeletal disorders like joint arthritis, bone defects, osteonecrosis of the femoral head, ligament tears, and pseudoarthrosis as well. In fact, previous studies [9,10] have evaluated the application of this orthobiologic material for the repair of long-bone pseudoarthrosis, specifically. Fernandez-Bances et al., [10] aimed to describe the effects of the combination of iliac crest-derived autologous bone marrow mononuclear cells with allogenic bone graft in long-bone pseudoarthrosis of seven patients. All patients exhibited complete bone consolidation in approximately 5 months after the cell transplantation treatment along with total elimination of pain. No adverse events or cases of infection following the medical procedures occurred. The authors maintained a mean follow-up period of 35.8 months after the procedure and reported no recurrence of pseudoarthrosis or any signs of associated symptoms. Despite the small sample size, the bone marrow product still presented itself as a safe, inexpensive, easy and efficacious alternative for the treatment of an often complicated and debilitating orthopedic condition.
In similar fashion, Memeo et al., [9] recently conducted a comparative study to investigate the effectiveness of Bone Marrow Aspirate Concentrate (BMAC) as an adjuvant therapeutic in the surgical treatment of congenital pseudoarthrosis of the tibia. Again, surgical treatments for this condition often demand multiple operations and may prove to be complicated. In their study, the authors aimed to evaluate the effectiveness of in-situ injections of BMAC for congenital tibial pseudoarthrosis in individuals treated with external fixation and that of radiographic healing over time in comparison to external fixation treatment alone. It was found that the patients who received a combination of external fixation and BMAC treatment exhibited a statistically significant improvement of healing time when compared to those who were treated with external fixation only. These observations might be attributed to the fact that since the bone marrow is known to contain a rich population of MSCs, the injection of these cells into the target site after focus removal in combination with circular external fixation may therefore promote accelerated bone healing in comparison to external fixation alone.
Conclusion
In our case report, the patient exhibited a very positive response to the treatment with no serious adverse effects. We were unable to find studies specifically evaluating the administration of bone marrow products for thoracic rib trauma and pseudoarthrosis. However, the studies analyzing this orthobiologic for delayed union and non-union of long-bones provided sufficient motivation to treat our patient’s condition with BMA, meeting expected clinical outcomes. BMA infiltrations resulted insignificant improvements in pain, functional outcomes and expressive signs of complete consolidation after the second treatment session. Further studies are highly warranted in order to fully elucidate the mechanisms underpinning this technique.
References
- Talbot BS, Gange CP, Chaturvedi A, Klionsky N, Hobbs SK, et al. (2017) Traumatic rib injury: Patterns, imaging pitfalls, complications, and treatment. Radiographics 37: 628-651.
- Ivey KM, White CE, Wallum TE, Aden JK, Cannon JW, et al. (2012) Thoracic injuries in US combat casualties: A 10-year review of Operation Enduring Freedom and Iraqi Freedom. J. Trauma Acute Care Surg 73: S514-S519.
- Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S (2003) Chest injury due to blunt trauma. Eur J Cardio-thoracic Surg 23: 374-378.
- Lana JF, da Fonseca LF, Azzini G, Santos G, Braga M, et al. (2021) Bone marrow aspirate matrix: A convenient ally in regenerative medicine Int J Mol Sci 22: 2762.
- Stewart SK (2019) Fracture non-union: A review of clinical challenges and future research needs. Malaysian Orthop J 13: 1-10.
- Sirmali M, Türüt H, Topçu S, Gülhan E, Yazici U, et al. (2003) A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur J Cardio-thoracic Surg 24: 133-138.
- Al-Hassani A, Abdulrahman H, Afifi I, Almadani A, Al-Den A, et al. (2010) Rib fracture patterns predict thoracic chest wall and abdominal solid organ injury. Am Surg 76: 888-891.
- Park S (2012) Clinical analysis for the correlation of intra-abdominal organ injury in the patients with RIB fracture. Korean J Thorac Cardiovasc Surg 45: 256-250.
- Memeo A, Verdoni F, Minoli CF, Voto A, D'Amato RD, et al. (2020) Effectiveness of bone marrow aspirate concentrate (BMAC) as adjuvant therapy in the surgical treatment of congenital pseudoarthrosis of the tibia: A retrospective comparative study. J Biol Regul Homeost Agents 34: 431-440.
- Fernandez-Bances I, Perez-Basterrechea M, Perez-Lopez S, Batalla DN, Rodriguez MAF, et al. (2013) Repair of long-bone pseudoarthrosis with autologous bone marrow mononuclear cells combined with allogenic bone graft. Cytotherapy 15: 571-577.
Citation: Braga M, Braga VC, Setti T, Santos GS, Lana JF (2021) Bone Marrow Aspirate for Delayed Union due to Severe Thoracic Rib Trauma. J Stem Cell Res Dev Ther 7: 077.
Copyright: © 2021 Marcelo Braga, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

