
Central Venous Oxygen Saturation as a Mortality Marker in Septic Shock: An Observational Study
*Corresponding Author(s):
Sundrani OmprakashDepartment Of Anesthesiology And Critical Care, Pt J.N.M. Medical College & Dr. B.R.A.M. Hospital, India
Tel:+91-9179893535,
Email:draparnamishra@gmail.com
Abstract
Background: Septic shock is a leading cause of morbidity and mortality. Central Venous Oxygen Saturation (ScVO2) is a prognostic marker of patients in septic shock. It is influenced by the oxygen-carrying capacity of blood, organ perfusion and metabolic oxygen consumption. Tissue hypoxia may sometimes occur despite adequate global oxygen delivery. In such scenarios, ScVO2 can be useful to predict increased risk of mortality. In the previous studies on ScVO2, its importance as a tissue oxygen marker and its importance in critical care have been studied. It has not been viewed as a mortality marker previously. The present study conducted to explore the association of ScVO2 with 28 days mortality in patients with septic shock, admitted to the Critical Care Unit (CCU) and, to evaluate the usefulness of ScVO2 as a mortality marker.
Materials and Methods: A prospective, observational study which was conducted on patients admitted to the CCU with septic shock. 76 patients were enrolled for study based on inclusion and exclusion criteria. Central venous sampling by Central Venous Catheter (CVC) was done for initial ScVO2 value (T0) and was repeated after 6 hours of resuscitation for ScVO2 value (T6) to assess the response to resuscitation. All enrolled patients were observed for a period of 28 days and were divided into 2 groups based on the outcome: Group NS (Non-Survivor group, which included patients who did not survive at the end of 28 days) and Group S (Survivor group, which included patients who survived at the end of 28 days) and ScVO2 values were compared between the survivor and non-survivor group.
Results: In our study, out of 76 patients, 44 patients (57.89%) were non-survivors and 32 patients (42.11%) were survivors. The mean Central Venous Oxygen Saturation (ScVO2) at the time of admission (T0) was 64.00 ± 2.74% among non-survivors and 73.22 ± 2.62% among survivors, and after six hours of resuscitation (T6) it was 63.30 ± 2.91% among non-survivors and 73.97 ± 2.31% among survivors. The sensitivity of ScVO2 at T0 in terms of mortality for value < 70% was 88.64% and specificity was 81.25% (OR = 33.8, 95% CI = 9.34, 122.35) and sensitivity of ScVO2 at T6 in terms of mortality for value < 70% was 93.18% and specificity was 93.75% (OR = 205, 95% CI = 32.23, 1303.97), which reflected that patients with ScVO2 < 70% had a poor prognosis as compared to patients with ScVO2 > 70%.
Conclusion: Central Venous Oxygen Saturation (ScVO2) values of less than 70% at the time of admission to CCU (T0) and six hours after the resuscitation (T6) was associated with higher 28 days mortality. From the observations and analysis of our study, it can be concluded that ScVO2 can be used as a predictor of mortality in patients of septic shock.
Keywords
Central Venous Oxygen Saturation (ScVO2), Critical Care Unit (CCU); Septic shock
INTRODUCTION
Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality and is defined as sepsis along with persistent hypotension requiring vasopressors to maintain MAP ≥ 65mm Hg, and Lactate ≥ 2mmol/L despite adequate fluid resuscitation [1]. Goal-directed therapy helps to predefine resuscitation endpoints to help clinicians at the bedside in the resuscitation of patients in septic shock. Two essential features of early goal-directed therapy are maintenance of Central Venous Pressure (CVP) > 8 mmHg and Central Venous Oxygen Saturation (ScVO2) ≥ 70% [2].
Central Venous Oxygen Saturation (ScVO2) is influenced by the oxygen carrying-capacity of blood, organ perfusion and metabolic oxygen consumption. It reflects the changes in oxygen delivery and consumption ratio. Central venous oxygen saturation (ScVO2) is a prognostic marker of patients in shock which has been underutilized in the critical care setting. Previous studies have used venous oxygen saturation as a therapeutic goal. Tissue hypoxia may sometimes occur despite adequate global oxygen delivery. Unrecognized global tissue hypoxia is associated with an increased risk of mortality and morbidity. Hence accurate detection is of prime importance. Vital signs are not sufficient for accurate and timely detection. In such scenarios, ScVO2 can be useful to predict increased risk of mortality. It can be measured from a blood sample taken from the central venous catheter or pulmonary artery catheter.
In the previous studies on ScVO2, its importance as a tissue oxygen marker and its importance in critical care have been studied. It has not been viewed as a mortality marker previously. In the present study, the association of central venous oxygen saturation with 28 days mortality in patients with septic shock admitted to the Critical Care Unit (CCU) has been explored, to evaluate the usefulness of ScVO2 as a mortality marker.
MATERIALS AND METHODS
An observational, prospective study conducted in the Department of Anesthesiology and Critical care at Pt. J.N.M. Medical College & Dr. B.R.A.M. Hospital, Raipur (C.G) from April 2018 to July 2019 to predict mortality in patients admitted to the Critical Care Unit (CCU) using ScVO2% at T0 and T6. After applying inclusion and exclusion criteria, a total of 76 patients were selected for study and all of them were followed over a period of 28 days.
Study Design: Prospective, Observational study
Study location: Pt. J.N.M. Medical College and Dr. B.R.A.M. Hospital, Raipur (C.G.)
Study Duration: April 2018 to July 2019
Sample size: 76
Sample size calculation: Using epitool by one-tailed test, taking confidence of 95%.
Study population: Patients admitted to the Critical Care Unit (CCU) of Dr. B.R.A.M. Hospital.
Inclusion Criteria: Septic shock patients of either sex aged ≥ 18 years of age.
Exclusion Criteria:
- Patients with contraindication to central venous catheterization.
- Age < 18 years.
- Patients with systolic dysfunction.
- Patients revived by Cardio-Pulmonary Resuscitation (CPR).
- Patients with imminent death.
Methodology
As the patient got shifted to the CCU, the patient’s medical records were reviewed; demographic data, clinical data, vital signs, diagnosis and associated co-morbidities were recorded. Sequential Organ Failure Assessment (SOFA score) and Systemic Inflammatory Response Syndrome (SIRS) criterion, Simplified Acute Physiology Score (SAPS II) were calculated at that time. Central venous catheter was inserted for monitoring of Central Venous Pressure (CVP) and evaluation of ScVO2, venous sampling by CVC was then done for initial ScVO2 value (T0), and an arterial blood sample was done for lactate, pH and bicarbonate levels. Venous blood sampling by CVC was repeated after 6 hours of resuscitation for ScVO2 value (T6) to assess the response to resuscitation. All enrolled patients were observed for 28 days and divided into 2 groups based on the outcome: Group NS (Non-Survivor group, which included patients who did not survive at the end of 28 days) and Group S (Survivor groups, which included patients who survived at the end of 28 days).
Statistical analysis
Univariate analyses were used to evaluate the correlations between all the variables. Multivariate logistic regression analysis using the mortality risk factors determined by univariate analysis was used to find the independent predictor of mortality. A Receiver Operating Characteristic (ROC) curve was plotted to determine the most appropriate cut off value of central venous oxygen saturation (ScVO2) at T0 and T6 used independently to predict the mortality.
Categorical data are expressed as percent, and continuous variables are expressed as mean ± SD. Continuous variables were compared by using independent Student’s t-test. Odds Ratios (OR) is given with the 95% CI. A two-tailed P-value < 0.05 was considered statistically significant.
RESULTS
Among 76 patients enrolled in the study 72.37% (n = 55) were male and 27.63% (n = 21) were female. Male: Female distribution in NS and S group was 37:7 and 18:14 respectively. The total number of patients who died in the follow-up duration of 28 days was 44 (57.89%) and was grouped as non-survivors whereas the remaining 32 (42.11%) patients who survived were grouped under the survivor group. The difference in gender distribution between group NS and group S was found to be statistically significant (p-value = 0.01), with odds of non-survival was found more for male gender (OR = 0.24, 95% CI = 0.08, 0.71). [Table 1, Figures 1-3].
|
Variable |
Groups based on Outcome (mortality at day 28) |
||
|
Gender |
Group NS |
Group S |
Total |
|
n=44 (57.89%) |
n=32 (42.11%) |
N=76 (100%) |
|
|
Male |
37 (67.27%) |
18 (32.73%) |
55 (100%) |
|
Female |
07 (33.33) |
14 (66.67%) |
21 (100%) |
|
H/O Chronic Disease |
|
|
|
|
Present |
32 (64%) |
18 (36%) |
50 (100)% |
|
Absent |
12 (46.15%) |
14 (53.85%) |
26 (100)% |
|
Ventilator Use |
44 (57.89%) |
32 (42.11%) |
76 (100%) |
|
Vasopressors Use |
44 (57.89%) |
32 (42.11%) |
76 (100%) |
|
ScVO2% < 70% at T0 to ScVO2% ≥ 70% at T6 |
3 (33.33%) |
6 (66.67%) |
9 (100%) |
Table 1: Demographic, clinical characteristics, treatment and outcome of enrolled 76 patients.
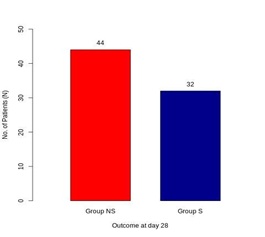 Figure 1: Distribution of study subjects based on the outcome.
Figure 1: Distribution of study subjects based on the outcome.
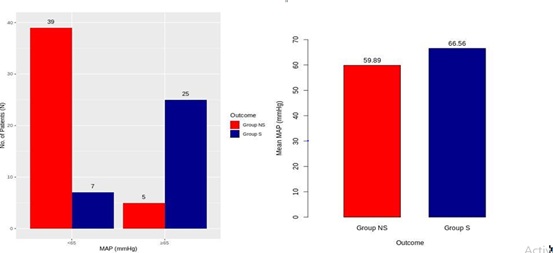 Figure 2: Distribution of Mean Arterial Pressure (MAP) and outcome.
Figure 2: Distribution of Mean Arterial Pressure (MAP) and outcome.
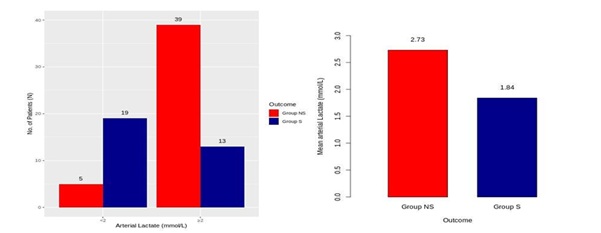 Figure 3: Distribution of arterial Lactate and outcome.
Figure 3: Distribution of arterial Lactate and outcome.
The mean Central Venous Oxygen Saturation (ScVO2) at the time of admission (T0) was 64.00 ± 2.74% among non-survivors and 73.22 ± 2.62% among survivors, and after six hours of resuscitation (T6) it was 63.30 ± 2.91% among non-survivors and 73.97 ± 2.31% among survivors. Differences between the mean of ScVO2 were significant (p-value < 0.001) at both T0 and T6 [Table 2, Figure 4-5].
|
Variable |
Group NS (n = 44) Mean ± SD |
Group S (n = 32) Mean ± SD |
p-value |
|
Age (in Years) |
50.34 ± 13.01 |
43.53 ± 15.04 |
0.04 |
|
MAP (mmHg) |
59.89 ± 4.16 |
66.56 ± 2.45 |
< 0.001 |
|
Arterial Lactate (mmol/L) at T0 |
2.73 ± 0.58 |
1.84 ± 0.68 |
< 0.001 |
|
ScVO2 (%) at T0 |
64.09 ± 2.92 |
72.97 ± 2.91 |
< 0.001 |
|
ScVO2 (%) at T6 |
63.48 ± 3.12 |
73.75 ± 2.59 |
< 0.001 |
|
SAPS II Score |
50.34 ± 3.09 |
42.34 ± 2.25 |
< 0.001 |
|
SOFA Score |
11.02 ± 1.25 |
7.56 ± 1.08 |
< 0.001 |
Table 2: Demographic, clinical characteristics, treatment and outcome of enrolled 76 patients.
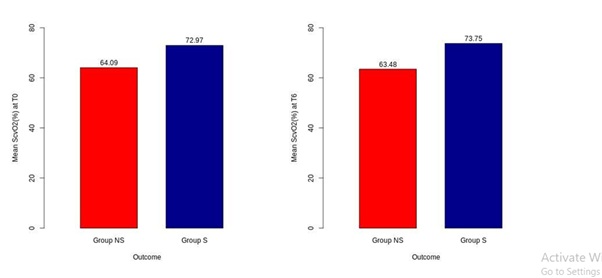 Figure 4: Mean ScVO2 of groups at T0 and T6.
Figure 4: Mean ScVO2 of groups at T0 and T6.
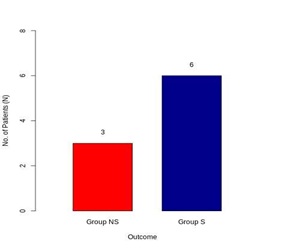 Figure 5: Effect of intervention on the outcome.
Figure 5: Effect of intervention on the outcome.
The sensitivity of ScVO2 at T0 in terms of mortality for value < 70% was 88.64% and specificity was 81.25% (OR = 33.8, 95% CI = 9.34, 122.35) and study the sensitivity of ScVO2 at T6 in terms of mortality for value < 70% was 93.18% and specificity was 93.75% (OR = 205, 95% CI = 32.23, 1303.97) [Table 3].
|
Variable |
Outcome |
p-value |
Relative Risk for Outcome (Group NS / Group S) |
||
|
Gender |
Group NS (N = 44) |
Group S (N = 32) |
Total (N = 76) |
|
|
|
Female |
7 |
14 |
21 |
0.01 |
0.24 |
|
Male |
37 |
18 |
55 |
|
|
|
Chronic Disease |
|
|
|
|
|
|
Absent |
12 |
14 |
26 |
0.14 |
0.48 |
|
Present |
32 |
18 |
50 |
|
|
|
ScVO2 at T0 |
|
|
|
|
|
|
< 70% |
39 |
6 |
45 |
< 0.001 |
33.8 |
|
≥ 70% |
5 |
26 |
31 |
|
|
|
ScVO2 at T6 |
|
|
|
|
|
|
< 70% |
41 |
2 |
43 |
< 0.001 |
205 |
|
≥ 70% |
3 |
30 |
33 |
|
|
|
|
ScVO2% at T0 |
ScVO2% at T6 |
|
Sensitivity |
88.64% |
93.18% |
|
Specificity |
81.25% |
93.75% |
|
Positive Predictive Value |
86.67% |
95.35% |
|
Negative Predictive Value |
83.67% |
90.91% |
|
Positive Likelihood Ratio |
4.73 |
14.91 |
|
Negative Likelihood Ratio |
0.14 |
0.07 |
Table 3: Relative risk, Sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio and negative likelihood ratio based on ScVO2 value at T0 and T6.
The ROC area under the curve for ScVO2 at T0 which was assumed to be a predictor of mortality was 0.96 (p-value < 0.001). The best cut off value for ScVO2 at T0 using the ROC curve was 69% with 100% sensitivity and 88.64% specificity, similarly, the ROC area under the curve for ScVO2 at T6 as a predictor of mortality was 0.99 (p-value < 0.001). The best cut off value for ScVO2 at T6 using ROC was 69% with 100% sensitivity and 90.91% specificity. According to the guidelines by Surviving Sepsis Campaign, the target cut off value of ScVO2 was set as 70% [Table 4, Figure 6-7].
|
Variable |
Area Under Curve |
p-value |
|
Mean ScVO2 value at T0 |
0.96 |
< 0.001 |
|
Mean ScVO2 value at T6 |
0.99 |
< 0.001 |
Table 4: ROC curve for ScVO2.
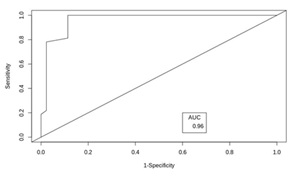 Figure 6: ROC of ScVO2 at T0.
Figure 6: ROC of ScVO2 at T0.
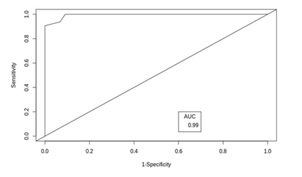 Figure 7: ROC of ScVO2 at T6.
Figure 7: ROC of ScVO2 at T6.
The difference of the mean of lactate value was 2.73 ± 0.58 mmol/L among non-survivors and 1.84 ± 0.68 mmol/L among survivors which was statistically significant (p-va1ue = 0.001) and showed higher mortality in patients with mean lactate > 2 mmol/L at the time of admission. Mean of SAPS II score was 50.34 ± 3.09 among non-survivors and 42.34 ± 2.25 among survivors. Mean of SOFA score was 11.02 ± 1.25 among non-survivors and 7.28 ± 0.58 in the survivor group. In our study, all 76 patients required ventilator support and were on vasopressors support. The presence of chronic disease was seen in 32 patients in the NS group and 18 patients in S group, with a relative risk of 0.48 (OR = 0.48, 95% CI = 0.18, 1.26), which reflected higher mortality among patients having a history of chronic disease.
DISCUSSION
Central Venous Oxygen Saturation (ScVO2) has been studied as a prognostic marker and as resuscitation end-point in patients with septic shock. Rivers E, et al., (2001) showed that an early therapeutic strategy that includes aiming for the rapid normalization of ScVO2 (≥ 70%) in patients suffering from septic shock at the time of admission to the emergency department could improve survival [3]. Since then, international guidelines have recommended targeting ScVO2 > 70% during the first 6 hours of care in patients presenting with severe sepsis or septic shock.
Since 2004, international guidelines for the treatment of severe sepsis and septic shock have been issued under the auspices of the Surviving Sepsis Campaign. Following these guidelines, all patients should be treated according to Early Goal-Directed Therapy (EGDT).
Early goal-directed therapy consists of the application of a bundle of interventions that are performed following a defined algorithm during the first 6 hours of treatment of patients in septic shock. Early goal-directed therapy includes the administration of fluid boluses until a Central Venous pressure (CVP) of 8 to 12 mm Hg has been reached, followed by the use of vasopressors if necessary aiming at a Mean Arterial Pressure (MAP) of at least 65 mmHg. If ScVO2 remains less than 70% and hematocrit is less than 30% then Red Blood Cell (RBC) transfusion is done to obtain a hematocrit more than 30% and if ScVO2 remains less than 70%, inotropes are administered to attain ScVO2 value to more than 70%.
Many scoring systems that show the severity of serious illness, such as the Acute Physiological and Chronic Health Evaluation II (APACHE-II), Sequential Organ Failure Assessment (SOFA), Simplified Acute Physiology Score (SAPS-II) for the prediction of mortality and morbidity. To the best of our knowledge, to date, no scoring systems consider the ScVO2 as a mortality marker in septic shock patients. The blood lactate level increases in response to tissue hypoxia and might be more sensitive for detection of imbalance between oxygen supply and demand. Limited reports analyzed the relationship between ScVO2 and mortality risk in septic shock patients. Our study aimed to determine whether Central Venous Oxygen Saturation (ScVO2) acts as a mortality marker in septic shock patients.
In a study conducted by Narula GK, et al., (2018) the 28 days mortality was 60% among patients who failed to achieve target ScVO2 > 70% [4]. Gajbe S, et al., (2018) found that the mean ScVO2 among non-survivors was 53.34 ± 4.08% [5]. Worapratya P, et al., (2016) concluded that the mortality rate of patients who failed to achieve the target goals of Early Goal Directed Therapy (EGDT) which included ScVO2 > 70% was found to be 93.8% [6]. Rady MY, et al., (1996) in their study concluded that after resuscitating patients with EGDT the mortality was 14% (5 patients out of 36), in patients with ScVO2 < 65% and low ScVO2 is associated with higher mortality, which was similar to our study [7].
In our study, all 76 patients required ventilator support. In a study by Gajbe S, et al., (2018) all 99 patients included in the study were on ventilator support which was similar to our study which could be explained by the fact that majority of the patients who were admitted to our CCU were either transferred from other ICU for further management or postoperative cases who required ventilator support and invasive monitoring in the postoperative period [5].
Presence of chronic disease was seen in 32 patients in the group NS and 18 patients in group S, with a relative risk of 0.48 (OR = 0.48, 95% CI; 0.18, 1.26), which reflected higher mortality among patients having a history of chronic disease.
The mean SOFA score was 11.02 ± 1.25 among non-survivors and 7.28 ± 0.58 in the survivor group in our study, Narula GK, et al., (2018) observed the mean SOFA score of patients in ScVO2 group was 11.68 as compared to 11.71 in patients of lactate clearance [4]. Similar findings were seen in a study by Lee YK, et al., (2016) where the mean SOFA score was 10 (9 - 12) among non-survivors and 7 (5 - 9) among survivors which signify higher mortality associated with patients having higher SOFA score [8].
CONCLUSION
From the observations and analysis of this study, it can be concluded that Central Venous Oxygen Saturation (ScVO2) can be used as a predictor of mortality in patients of Septic shock. ScVO2 values of less than 70% at the time of admission to CCU (T0) and six hours after the resuscitation (T6) was associated with higher 28 days mortality.
REFERENCES
- Abraham E (2016) New definitions for sepsis and septic shock: continuing evolution but with much still to be done. JAMA 315: 757-759.
- Levy MM, Evans LE, Rhodes A (2018) The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 44: 925-928.
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, et al. (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345: 1368-1377.
- Narula GK, Singh AK, Adya A (2018) Comparison of central venous oxygen saturation and serum lactate clearance as predictors of outcome in septic shock patients: a prospective control trial. International Journal of Research in Medical Sciences 6: 653.
- Gajbe S, Dave S, Kasimahanti R (2018) Central Venous Oxygen Saturation as a Surrogate Marker of Outcome in Critically ill Patients-A Prospective Observational Cohort Study. Journal of Anaesthesia & Intensive Care Medicine 6: ID: 555698.
- Worapratya P, Wanjaroenchaisuk A, Joraluck J, Wuthisuthimethawee P (2016) Success of applying early goal-directed therapy for septic shock patients in the emergency department. Open Access Emerg Med 8: 1-6.
- Rady MY, Rivers EP, Nowak RM (1996) Resuscitation of the critically III in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. The American journal of emergency medicine 14: 218-225.
- Lee YK, Hwang SY, Shin TG, Jo IJ, Suh GY, et al. (2016) Prognostic value of lactate and central venous oxygen saturation after early resuscitation in sepsis patients. PLoS One 11: 0153305.
Citation: Omprakash S, Chandrapal B, Aparna M, Kamalkishore S (2020) Central Venous Oxygen Saturation as a Mortality Marker in Septic Shock: An Observational Study. J Anesth Clin Care 7: 52.
Copyright: © 2020 Sundrani Omprakash, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

