
Comparative Effectiveness of Statin Therapy in Reducing Cardiovascular Events
*Corresponding Author(s):
Maham FatimaDepartment Of Internal Medicine, Jinnah Sindh Medical University, Karachi, Pakistan
Email:mahamfatima598@gmail.com
Abstract
Statins are a class of drugs that can help lower the blood’s low-density lipoprotein (LDL) cholesterol level. Evidence suggests that all statins are associated with a statistically significant reduction in risk for primary and secondary cardiovascular events. The drug efficacy may differ among statins, and evidence from head-to-head comparisons needs to be more extensive and consistent.
Statin therapy is associated with a reduced relative risk of all-cause mortality, Cardiovascular Mortality, CHD mortality, and fatal Myocardial Infarction (MI), but not fatal stroke. It is also linked with a reduced relative risk of morbidity [non-fatal MI, non-fatal stroke, Transient Ischaemic Attack (TIA), unstable angina] and coronary revascularization. The study aims to compare the effects of different statins in decreasing the risk of cardiovascular diseases by conducting systematic reviews and Network Meta-Analyses (NMA) after certain statins' use. This study employs a Systematic Literature Review (SLR) and meta-analysis approach to provide an overview of the existing literature. A total of 811 references from reputable journals published between 2013 and Aug 1, 2023, were reviewed, focusing on eight selected papers for in-depth analysis. The systematic review revealed that drug efficacy to reduce cardiovascular events may differ among statins. However, the comparative effectiveness of different statins in this group remains to be determined. This study aimed to compare various forms of statins and their associations with reducing cardiovascular events.
Keywords
Cardiovascular events; Cholesterol; Coronary Heart Disease; Meta-analysis; LDL 3-Hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors
Introduction and Background
Coronary Heart Disease (CHD) is most countries' leading cause of death [1]. Statins are the preferred pharmacological treatment for reducing elevated lipid levels in individuals with confirmed Atherosclerotic Cardiovascular Disease (ASCVD), and their beneficial effects have also been demonstrated in normolipidemic patients [2]. Statin medications are the most productive and scientifically supported drugs for preventing and treating this condition. They are pivotal in its management and are recommended in all established clinical guidelines [1]. All statins showed a statistically significant risk reduction of all-cause mortality and CVD in primary prevention populations while raising the risk for some harm chances. However, the benefit-harm profile differed by statin type [3].
While all statins can lower cholesterol levels, they exhibit variations in their chemical composition, pharmacokinetics (including characteristics like lipophilicity), and effectiveness in reducing LDL cholesterol, and potential pleiotropic effects, which can result in diverse clinical outcomes within the same class. Additionally, the lipophilicity of a statin is a crucial factor to consider, as it may impact the overall risk-benefit profile of a specific statin. Furthermore, hydrophilic statins might be associated with fewer side effects and drug interactions than lipophilic statins due to their reduced susceptibility to metabolism by cytochrome P450 enzymes, potentially resulting in a lower risk of muscle-related toxicity and improved treatment adherence [4].
Statin medications, recognized as the most effective and evidence-supported treatments for preventing and managing this condition, play a central role in its management and are recommended in all available guidelines. The 2013 American College of Cardiology/American Heart Association (ACC/AHA) cholesterol and assessment guidelines, often referred to as the 'new ACC/AHA guidelines,' prioritized the reduction of overall Cardiovascular (CV) risk over specifically targeting low-density lipoprotein-cholesterol (LDL-C) levels [1,5], stressed the use of statins in two dose intensities, utilized a new risk calculator using pooled cohort equations, and lowered the risk cutoff for initiation of statin therapy [1].
The National Cholesterol Education Program in the United States suggests using LDL-C values to estimate cardiovascular disease risk linked to lipoproteins in individuals. However, non-high-density lipoprotein cholesterol (non-HDL-C) might have a stronger association with cardiovascular disease risk in patients taking statins. It could be a more effective tool than LDL-C for evaluating both the risk of cardiovascular disease and the impact of treatment. This recommendation is based on the rationale that non-HDL-C encompasses all potentially atherogenic cholesterol in lipoprotein particles, including LDL, lipoprotein (a), intermediate-density lipoprotein, and remnants of very low-density lipoprotein [5].
The ASPREE (Aspirin in Reducing Events in the Elderly) trial revealed that individuals who were already taking statins at the beginning of the study experienced substantial reductions in the risk of cardiovascular disease events. These reductions included a 32% decrease in major adverse cardiovascular events (MACE), a 29% reduction in fatal cardiovascular disease (CVD), a 44% decrease in myocardial infarction (MI), and a 25% lower risk of stroke[4].
Although statins have shown promise in lowering the risk of cardiovascular diseases, no study has examined and compared the effectiveness of various statins in reducing cardiovascular events. Consequently, we conducted a systematic review to assess the relative efficacy of different statins.
Methods
This review focuses on clinical studies concerning the effectiveness of statins in reducing cardiovascular events. We excluded animal studies and publications that only discussed cases without presenting clinical data [6-10]. The review follows the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [11,12] for 2020 in Figure 1. It only uses data collected from published papers, eliminating the need for ethical approval.
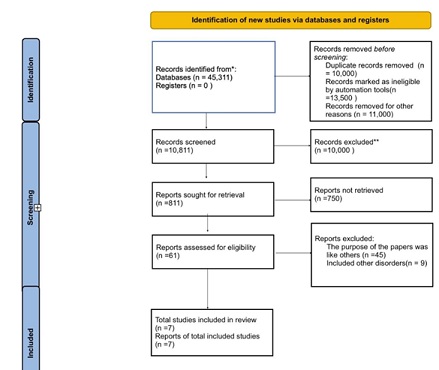 Figure 1: Identifications of new studies via databases and registers.
Figure 1: Identifications of new studies via databases and registers.
Systematic Literature Search and Study Selection
We conducted a thorough search for relevant publications by using PubMed and Google Scholar. We searched for studies mentioned in review papers, editorials, and commentaries on PubMed. Nevertheless, we continued searching for additional studies that satisfied our inclusion criteria.
We had a list of abstracts that we independently reviewed for inclusion using specific criteria. The criteria included different statins, focusing on reducing cardiovascular events, and a clearly described clinical cohort in the study. We excluded review papers and animal studies. Six reviewers conducted a dual review, and disagreements were resolved through discussion.
Inclusion And Exclusion Criteria
We established specific criteria for including and excluding participants to achieve our study goals. Our Criteria can be summarized in Table 1.
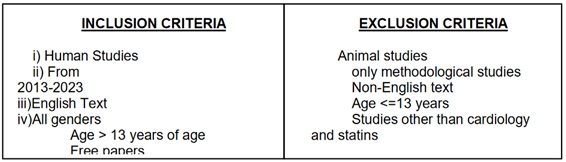 Table 1: Showing the criteria adopted during the literature search process.
Table 1: Showing the criteria adopted during the literature search process.
Search Strategy
The population, intervention/condition, control/comparison, and Outcome (PICO) criteria were utilized to conduct a thorough literature review. The search was conducted on databases such as PUBMED (including Medline) and Google Scholar Libraries, using relevant keywords, such as statins and cardiovascular events. The medical subject heading (MeSH) approach for PubMed (including Medline) and Google Scholar, as detailed in Table 2, was employed to develop a comprehensive search strategy.
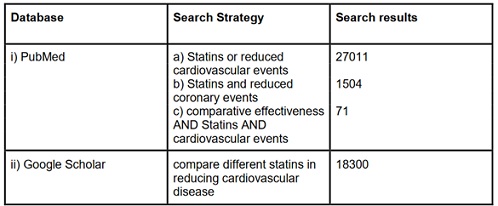 Table 2: Showing the search strategy, search engines used, and the number of results displayed.
Table 2: Showing the search strategy, search engines used, and the number of results displayed.
Quality Appraisal
To ensure the reliability of our chosen papers, we utilized various quality assessment tools. We employed the PRISMA checklist and Cochrane bias tool assessment for randomized clinical trials for systematic reviews and meta-analyses. Non-randomized clinical trials were evaluated using the Newcastle-Ottawa tool scale. We assessed the quality of qualitative studies, as shown in Table 3, using the Critical Appraisal Skills Program (CASP) checklist. To ensure clarity in the classification, we utilized the Scale to Assess Narrative Review Articles (SANRA) to evaluate the article's quality.
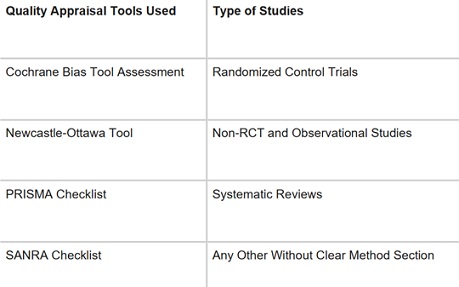 Table 3: Showing quality appraisal tools used.
Table 3: Showing quality appraisal tools used.
PRISMA: Preferred reporting items for systematic reviews and meta-analyses; SANRA: Scale for the assessment of non-systematic review articles
Results
After searching through three selected databases, PubMed, Medline, and Google Scholar, we extracted 45,311 articles. We then carefully reviewed each paper and applied specific criteria, which led to the exclusion of 13,500 pieces. From the remaining 31,811 papers, we chose not to utilize 21,000 of them due to duplicates or unsatisfactory titles and abstracts. We closely examined the remaining 61 papers and excluded 54 more as their content did not meet our inclusion criteria. Finally, we conducted a thorough quality check on the remaining seven papers, which all met our criteria. These eight articles are included in our final systematic review. Table 4 provides a detailed description of each.
|
Author / Year |
Country |
Study design |
Database used |
Conclusion |
|
Wang C et |
China |
Meta-Analysis |
Pubmed |
Combination |
|
Adams SP et al. [9] |
Canada |
Systematic |
Pubmed |
Pravastatin |
|
Yebyo HG et al.[3] |
Switzerland |
Meta- |
Pubmed |
All statins |
|
Naci H et |
UK |
Meta- |
Pubmed |
Statins |
|
Zhai C et |
China |
Meta- |
Pubmed |
In secondary |
|
Zhou Z et |
Australia and |
Post-hoc |
Pubmed |
There were |
|
Zhang X et |
China |
Systematic |
Pubmed |
Rosuvastatin is |
Table 4: Summary of the results of the selected papers.
AUC: Area Under Curve; Statins, Cardiovascular Diseases, HMG-CoA Reductase Inhibitors.
Discussion
Hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitors, commonly known as “statins”, are prescribed in conjunction with dietary and exercise interventions to manage hypercholesterolemia. They work by reducing Total Cholesterol (TC), Low-Density Lipoprotein Cholesterol (LDL-C), and triglycerides (TG) levels while elevating high-density lipoprotein cholesterol (HDL-C). FDA-approved indications for statins may vary slightly, but they are generally recommended for the treatment and prevention of atherosclerotic cardiovascular disease (ASCVD) like heart attacks and strokes [6].
Statins exert their preventive effects on the progression of cardiovascular disease through several key mechanisms: (i) Plaque Stabilization (ii) Inflammation Reduction (iii) Improved Endothelial Function (iv) Reduced Thrombogenicity [7].
The evolution of cholesterol management guidelines, which began with the initial Adult Treatment Panel (ATP) recommendations in 1988, has placed significant emphasis on aggressively lowering low-density lipoprotein cholesterol (LDL-C) levels in individuals at risk of coronary heart disease (CHD). In 2001, the National Cholesterol Education Panel (NCEP) ATP III guidelines introduced stringent LDL-C targets, particularly for patients with established CHD, non-coronary atherosclerosis, diabetes, or multiple risk factors. Subsequent studies like the Heart Protection Study (HPS) and Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE IT) provided additional evidence supporting the advantages of reducing LDL-C levels below 100 mg/dL, leading to proposed guideline updates. These updates included the introduction of an 'optional' LDL-C target below 70 mg/dL for individuals at very high risk and less than 100 mg/dL for those at intermediate risk [8].
While statins serve as the primary pharmacological approach to achieving these targets, it's important to note that their clinical effectiveness can vary among different statins [8]. Rosuvastatin, particularly at high and moderate intensities, as well as simvastatin and atorvastatin at high intensity, exhibited the most significant effectiveness in reducing non- HDL-C concentrations compared to a placebo [5]. However, Pravastatin lowers blood total cholesterol, LDL cholesterol and triglyceride in a dose-dependent linear fashion [9].
The clinical findings from the present study indicate that statin therapy yields greater benefits in secondary prevention compared to primary prevention. Statins are associated with a significant reduction in the risk of mortality, cardiovascular events, and the need for revascularization procedures [10].
When it comes to reducing major coronary events at similar doses, both atorvastatin and fluvastatin were found to be notably more effective than rosuvastatin. In the context of secondary prevention for major coronary events, atorvastatin demonstrated superior effectiveness compared to pravastatin and simvastatin. However, in primary prevention, statins exhibited a significant reduction in deaths and major coronary events, with no discernible differences observed among individual statins [10].
Across all populations studied atorvastatin, fluvastatin, and simvastatin emerged as having the highest overall probabilities of being the most effective treatments in terms of reducing both deaths and major coronary events [10].
Limitations
Our literature review has limitations. We limited our analysis to English articles published within the last ten years. We also only used free articles, and our study was limited to English papers on statins for diagnosis and prognosis. More research is needed for specific conclusions.
Conclusion
Evidence strongly suggests that statins reduce the risk of all-cause mortality, cardiovascular events, and revascularization when used for secondary prevention. However, the overall evidence level for primary prevention is low. Differences in the effects among statins have potential therapeutic equivalence for secondary prevention. Further studies are needed to ascertain the benefits of statins for primary prevention.
Compliance with Ethical Standard
- Conflict of interest
The authors declare that they have no conflict of interest
- Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
- Informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors, so there was no need for informed consent.
References
- Kones R, Rumana U (2015) Current Treatment of Dyslipidemia: A New Paradigm for Statin Drug Use and the Need for Additional Therapies. Drugs 75: 1187-1199.
- Zhang X, Xing L, Jia X, Pang X, Xiang Q, et al. (2020) Comparative Lipid- Lowering/Increasing Efficacy of 7 Statins in Patients with Dyslipidemia, Cardiovascular Diseases, or Diabetes Mellitus: Systematic Review and Network Meta-Analyses of 50 Randomized Controlled Trials. Cardiovasc Ther Page no: 1-21.
- Yebyo HG, Aschmann HE, Kaufmann M, Puhan MA (2019) Comparative effectiveness and safety of statins as a class and of specific statins for primary prevention of cardiovascular disease: A systematic review, meta-analysis, and network meta-analysis of randomized trials with 94,283 participants. Am Heart J 210: 18-28.
- Zhou Z, Curtis AJ, Ernst ME, Ryan J, Zoungas S, et al. (2021) Comparison of statins for primary prevention of cardiovascular disease and persistent physical disability in older adults. Eur J Clin Pharmacol.
- Hodkinson A, Tsimpida D, Kontopantelis E, Rutter MK, Mamas MA, et al. (2022) Comparative effectiveness of statins on non-high density lipoprotein cholesterol in people with diabetes and at risk of cardiovascular disease: systematic review and network meta-analysis. BMJ 376: 067731.
- Levine G, Bates E, Bittl J, Brindis R, Fihn S, et al. (2012) 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for Circulation 134: 123-55.
- Mihos CG, Pineda AM, Santana O (2014) Cardiovascular effects of statins, beyond lipid-lowering properties. Pharmacol Res 88: 12-19.
- Talwalkar PG, Sreenivas CG, Gulati A, Baxi H (2013) Journey in guidelines for lipid management: From adult treatment panel (ATP)-I to ATP-III and what to expect in ATP-IV. Indian Journal of Endocrinology and Metabolism 17: 628-635.
- Tasnim S, Wright JM (2023) Pravastatin for lowering lipids. Cochrane Database Syst Rev 9: 13673.
- Naci H, Brugts JJ, Fleurence R, Tsoi B, Toor H, et al. (2013) Comparative benefits of statins in the primary and secondary prevention of major coronary events and all- cause mortality: a network meta-analysis of placebo-controlled and active-comparator trials. European Journal of Preventive Cardiology 20: 641-657.
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, et al. (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2: 349.
- Zhai C, Hou K, Li R, Hu Y, Zhang J, et al. (2020) Efficacy of statin treatment based on cardiovascular outcomes in elderly patients: a standard meta-analysis and Bayesian network analysis. The Journal of international medical research. 48: 300060520926349.
- Wang C, Wang F, Cao Q, Li Z, Huang L, et al. (2018) Effect and safety of combination lipid - lowering therapies based on statin treatment versus statin monotherapies on patients with high risk of cardiovascular events. Aging Med 1: 176-184.
Citation: Fatima M, Wajid F (2023) Comparative Effectiveness of Statin Therapy in Reducing Cardiovascular Events. J Diabetes Metab Disord 10: 051.
Copyright: © 2024 Maham Fatima, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

