
Effect of Continuous Spinal Anesthesia and Single Shot Spinal Anesthesia on Hemodynamics for Lower Abdominal and Hip Surgeries in Adults: An Observational Study
*Corresponding Author(s):
Shah Pratibha JainDepartment Of Anaesthesiology And Critical Care, Pt Jnm Medical College & Dr. Bram Hospital, Raipur, Chhattisgarh, India
Tel:+91 9827276620,
Email:prati_jain@rediffmail.com
Abstract
Purpose
Continuous Spinal Anesthesia (CSA) is the technique of initiating and maintaining spinal anesthesia with small incremental doses of local anaesthetic injected intermittently into the subarachnoid space through a catheter. Hemodynamic instability due to high block largely limits the use of conventional Single Shot Spinal Anesthesia (SSSA) in high risk patients. Our primary aim was to observe hemodynamic changes, total fluid and vasopressor consumption and incidence of Post Dural Puncture Headache (PDPH), meningitis, focal sensory block after CSA and SSSA in young adults.
Methods
Total 44 patients of ASA grades I-III aged 18-60 years, scheduled for lower abdominal and hip surgery received either CSA using 19G paediatric epidural Touhy needle and 22 G catheter (Group CSA; n=22) or SSSA with 25G Quinkes spinal needle (Group SSSA, n=22) using 0.75 % isobaric ropivacaine. Hemodynamics, total fluids &vasopressor consumption and incidence of adverse events were recorded.
Results
Demographically, patients were comparable between the groups. HR and DBP was found comparable within the groups and between the groups (p>0.05). Fall in SBP was significant in SSSA group from 10-45 min with respect to baseline and from 5-25 min when compared to CSA group after induction. Mean fluid infused higher in group SSSA (p=0.0176). Five patients in SSSA group while none in CSA group had significant hypotension (p=0.190). PDPH, meningitis, focal sensory block were not observed in any of the patients.
Conclusion
CSA provides better hemodynamic stability with minimal incidence of adverse events when compared to SSSA in young patients undergoing lower abdominal and hip surgeries using 0.75% Ropivacaine.
Keywords
INTRODUCTION
However, it is surprising that CSA has been successfully used for hip & lower limb surgeries [9-12] in high risk elderly [3, 7-8] as well as young patients [3,13] but has not been tested much in healthy young patients in whom any presumed risk would be theoretically much lower. Most of the studies concerning the risk-benefits of CSA were conflicting; hence we conducted this study to compare two spinal block techniques: continuous and single shot with isobaric Ropivacaine 0.75% for lower abdominal and hip surgeries in young patients in terms of hemodynamic and safety profile.
METHODS
Patients were shifted to operation theatre after thorough pre-anaesthetic evaluation. Baseline vitals i.e. Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) and Arterial Oxygen Saturation (SpO2) while breathing room air were recorded. Intravenous line was accessed by inserting 18 G intravenous cannula over dorsum of hand and i.v. Ringer Lactate (RL) was started at 5-6 ml/kg/h infusion rate. All the patients were premedicated with i.v. Ondansetron 4 mg and i.v. Ranitidine 50 mg.
Two operation theatre were assigned for this study and patients were grouped into group CSA and SSSA accordingly one for each operation theatre separately. Both CSA & SSSA were performed in sitting position. In CSA group, after injection of local anaesthetic in midline at L4-L5 interspace, subarachnoid space was accessed through 19G Tuohy’s paediatric epidural needle (Vygon 95440, ECOUEN France) from anaesthetized area under all aseptic precautions. After confirming free flow of CSF through the needle, 22G catheter primed with 0.5 ml of 0.75% Ropivacaine was inserted through it into subarachnoid space. The catheter was fixed in situ to keep 4 cm length into the intrathecal space. Patients were made supine and CSF flow was reconfirmed by aspiration through the catheter and 1 ml of initial bolus of 0.75% Ropivacaine was injected. After 5 min, the sensory block level was checked and if it had not reached upto T10, subsequent aliquots of 0.5 ml 0.75% Ropivacaine were administered till T10 anaesthetic level was achieved after assessment of sensory level at every 5 minutes interval. Same aliquots were repeated for maintenance of T10 sensory level throughout the surgery as and when required in all the patients. The catheter & filter has 0.5 ml of dead space & hence it was primed and flushed with 0.5 ml of normal saline after each bolus dose. Catheter was removed after completion of surgery.
In SSSA group, subarachnoid space was accessed through 25G Quinke’s spinal needle at L4-L5 interspace under all aseptic precautions. After confirmation of free flow of CSF by aspiration through the needle, 3 ml of single shot 0.75% Ropivacaine was injected into the subarachnoid space.
Sensory block level was assessed by Pin-prick method and degree of sensory block by 3-point scale [Category A -Patient experience of no discomfort, Category B -Mild discomfort not requiring systemic analgesia, Category C -Discomfort that require systemic analgesic]. Degree of motor block was assessed by Modified Bromage score [Grade 1 - Inability to elevate extended leg but able to flex knee, Grade 2 - Inability to flex knee but able to move foot only, Grade 3 - Inability to flex ankle, Grade 4 - Complete motor paralysis]. Time taken to reach sensory level of T10 dermatome by each patient in either group was also recorded.
After the LA injection, HR, SBP, DBP and SpO2 were recorded every 5min up to 30 min and then every 15 min till completion of surgery in all patients. Fall in SBP by 20% from baseline was labelled as hypotension and managed by i.v. Ringer lactate. Severe hypotension was labelled when mean blood pressure fell by 30% from baseline and managed by i.v. Mephentermine. Heart rate below 50 beats per min was considered as bradycardia and managed with 0.6 mg atropine. Intravenous Tramadol 50 mg was given slowly over 10 min for management of rigors.
Total amount of fluids and mephentermine administered, total duration of surgery, side effects [severe hypotension, bradycardia, rigors, nausea, vomiting & delayed micturition] and complications [PDPH, meningitis & focal sensory block] were also observed and recorded. Patients were followed up till 7 days for meningitis & 30 days for focal sensory block, for the purpose of power analysis & sample size, we took the study of Saber R et al [14], who compared CSA and SSSA in 34 high risk elderly patients undergoing orthopaedic limb surgeries. He found proportion of patients having severe hypotension among both the group as-
1st proportion (CSA) = 0.08
2nd proportion (SSSA) =0.51
Taking this into consideration, before the study we calculated the difference between these two proportions with confidence level 95%, α err probability 0.05 in 90% power, it yielded a sample size of total 44 patients (as calculated by Epitools Software) (n=22).
So, we collected data of 22 patients who had surgery under Continuous spinal anesthesia (Group CSA) and 22 patients who had surgery under Single shot spinal anesthesia (Group SSSA).
Statistical analysis was performed using Graph pad in stat software. Results were expressed as mean ± SD, number and percentage (%). Normally distributed data were analysed using unpaired Student’s t-test and comparison was done using chi-square (?2) test with p value (level of significance used as 0.05) reported at 95 % confidence level.
RESULTS
|
|
Group CSA |
Group SSSA |
p Value |
|
Age (yrs) |
39.54 ± 11.86 |
38.68 ± 10.53 |
0.7997 |
|
Sex (M:F) |
11:11 |
12:10 |
|
|
Height (cm) |
157.09 ± 7.90 |
154.90 ± 6.61 |
0.3244 |
|
Weight(kg) |
59.54 ± 11.62 |
61.63 ± 11.56 |
0.5530 |
|
Mean duration of surgery (min) |
135.68 ± 39.68 |
115.22 ± 30.13 |
0.0609 |
|
Mean time to reach T10 dermatome (min) |
4.81 ± 1.95 |
4.34 ± 0.85 |
0.3060 |
SSSA: Single Shot Spinal Anesthesia
Baseline HR in Group CSA and Group SSSA was 89.86 ± 14.90 bpm and 85.40 ± 14.22 bpm, respectively (p=0.3156). Post induction HR was comparable within the group and between the groups till the completion of surgery (Graph 1).
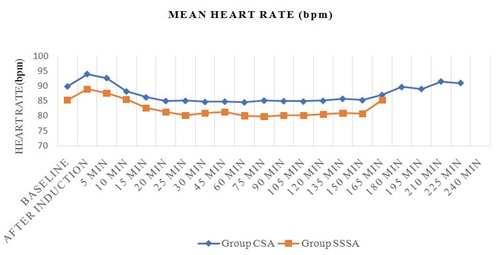
SSSA: Single Shot Spinal Anesthesia
bpm: beats per minute
Baseline mean SBP was 125.09 ± 8.82 mmHg and 123.59 ± 8.84 mmHg in group CSA and group SSSA, respectively (p=0.5761). A significant fall in SBP from 10 minutes to 45 minutes from baseline value was observed in SSSA group. Also, when compared with group CSA, SBP was significantly reduced in group SSSA from 5 minutes to 25 minutes time interval (Table 2). Baseline mean DBP in group CSA and Group SSSA was 72.90 ± 5.15 mmHg and 72.86 ± 6.35 mmHg respectively which were statistically comparable (p=0.9188). Post induction values of DBP were also comparable between both the groups (Graph 2).
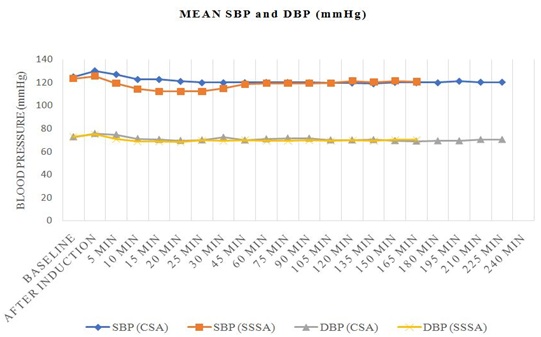
CSA: Continuous Spinal Anesthesia
SSSA: Single Shot Spinal Anesthesia
|
Time Interval |
Group CSA |
p value |
Group SSSA |
p value |
p value |
|
Baseline |
125.09±8.82 |
|
123.59±8.84 |
|
0.5761 |
|
After induction |
130.27±8.94 |
0.0598 |
125.5±12.29 |
0.5572 |
0.1484 |
|
5 min |
127.13±11.79 |
0.5193 |
119.22±12.84 |
0.1957 |
0.0392* |
|
10 min |
122.81±11.99 |
0.4764 |
114.4±12.08 |
0.0062* |
0.0254* |
|
15 min |
122.77±10.04 |
0.4201 |
112.22±12.84 |
0.0014* |
0.0041* |
|
20 min |
121.13±10.92 |
0.1929 |
112.22±13.63 |
0.0021* |
0.0213* |
|
25 min |
120±9.73 |
0.0762 |
112.22±12.26 |
0.0011* |
0.0246* |
|
30 min |
120.04±9.79 |
0.1568 |
114.68±8.83 |
0.0017* |
0.0634 |
|
45 min |
120.04±8.90 |
0.0656 |
118.36±8.02 |
0.0461* |
0.5143 |
|
60 min |
120.31±10.35 |
0.1067 |
119.27±7.38 |
0.0858 |
0.7031 |
|
75 min |
120.22±10.21 |
0.0979 |
119.31±6.93 |
0.0811 |
0.7311 |
|
90 min |
120.04±9.03 |
0.0708 |
119.27±6.09 |
0.0868 |
0.7608 |
|
105 min |
119.84±8.44 |
0.0638 |
119.50±6.57 |
0.1464 |
0.9020 |
|
120 min |
119.81±8.56 |
0.0734 |
121.30±5.36 |
0.4048 |
0.5898 |
|
135 min |
119.18±10.96 |
0.1043 |
120.42±3.86 |
0.3696 |
0.7789 |
|
150 min |
120.37±9.47 |
0.2138 |
121.50±5.06 |
0.6536 |
0.8304 |
|
165 min |
120±8.71 |
0.2982 |
120.66±3.78 |
0.5817 |
0.9086 |
|
180 min |
120±10.14 |
0.3647 |
|
|
|
|
195 min |
121.33±7.37 |
0.4898 |
|
|
|
|
210 min |
120.5±7.77 |
0.4862 |
|
|
|
|
225 min |
120.5±12.22 |
0.4972 |
|
|
|
|
240 min |
|
|
|
|
|
CSA: Continuous Spinal Anesthesia
SSSA: Single Shot Spinal Anesthesia
In our study, mean volume of fluid administered in Group CSA was significantly higher than in group SSSA (p=0.0176). None of the patient in CSA group required vasopressor while 4 (18.18%) patients in SSSA group required total of 12 mg of Mephentermine for the management of hypotension (Table 3).
|
|
Group CSA |
Group SSSA |
p Value |
|
Volume of fluid infused (ml) |
1209.09 ± 287.69 |
1472.72 ± 409.62 |
0.0176 |
|
Total Vasopressor consumed (mg) |
0 |
12 |
CSA: Continuous Spinal Anesthesia
SSSA: Single Shot Spinal Anesthesia
Hypotension and bradycardia were not seen in any patient of CSA group while 4 (18.18 %) patients (p=0.0381) and 1 (4.54%) patient (p=0.3192) of group SSSA experienced the same respectively. 9 and 5 patients in group SSSA experienced rigor and nausea, respectively which was statistically insignificant. Vomiting, meningitis or focal sensory block was not found in any patient in either group (Table 4).
|
Adverse Events |
Group CSA |
Group SSSA |
p Value |
|
Hypotension |
0 (0%) |
4 (18.18%) |
0.0381* |
|
Bradycardia |
0 (0%) |
1 (4.54%) |
0.3192 |
|
Rigor |
7 (31.81%) |
9 (40.90%) |
0.5355 |
|
Nausea |
1 (4.54%) |
5(22.72%) |
0.0823 |
|
Vomiting |
0 (0%) |
0 (0%) |
- |
|
Delayed Micturition |
0 (0%) |
0 (0%) |
- |
|
Post Dural Puncture Headache |
0 (0%) |
0 (0%) |
- |
|
Meningitis |
0 (0%) |
0 (0%) |
- |
|
Focal Sensory Block |
0 (0%) |
0 (0%) |
- |
CSA: Continuous Spinal Anesthesia
SSSA: Single Shot Spinal Anesthesia
DISCUSSION
In present study, HR was comparable within the group and between the groups till the completion of surgery. Studies of Saber R et al., [14], Klimscha W et al., [7], Favarel-Garrigues JF et al., [8], Lundorff L et al., [15], Maurer K et al., [11], Fettes PDW et al., [16], Baydilek Y et al., [17], Seetharam KR et al., [18] also showed similar results. Ebied RS et al., [19] found significant fall in HR relative to baseline (p<0.05) in CSA but were within the clinically acceptable range which might be due to the addition of fentanyl with 0.5% isobaric bupivacaine into the subarachnoid space in their study.
In our study, a significant fall in SBP from baseline was observed in SSSA from 10 minutes to 45 minutes. Also, when compared with group CSA, SBP was significantly reduced in group SSSA from 5 minutes to 25 minutes time interval. Though DBP was comparable in both the groups at all measured time intervals. Similar results were found in studies of Saber R et al., [14], Klimscha W et al., [7], Favarel-Garrigues JF et al., [8], Lundorff L et al., [15], Maurer K et al., [11], Fettes PDW et al., [16], Pitkanen M et al., [9]. Minville V et al., [12] found no significant variation in BP in either group (CSA or SSSA) after induction as they had preloaded all the patients with 8 ml/kg RL solution. Parthasarthy S et al., [1] found variations in hemodynamic that too within acceptable limits which could be due to administration of 2.5-3 ml of 0.5 % isobaric bupivacaine along with 1mg preservative free Midazolam intrathecally as bolus rather than titrating or fractionating the dose in CSA group while achieving the sensory blockade level of T4-T6. Baydilek Y et al., [17] noted Mean Blood Pressure (MBP) at 90-180 min and 4-24 h was significantly lower in SSSA than CSA group (p<0.05). While, MBP was significantly lower at 2.5-30 min in CSA group and all measured time interval in SSSA group than control values, respectively (p<0.05). This could be due to block level higher than T10 and premedication of all elderly ASA grade I-III patients with IM midazolam 0.03 mg/kg which has a depressant effect on sympathetic system especially in elderly patients.
We observed significantly higher incidence of hypotension in SSSA group (p=0.0381). Incidence of bradycardia, rigors and nausea was higher in SSSA group but was not significant (p > 0.05). None of the patient had vomiting, meningitis or focal sensory block in either group. Saber R et al., [14], Favarel-Garrigues JF et al., [8], Baydilek Y et al., [17], Seetharam KR et al., [18], Pitkanen M et al., [9], McNamee DA et al., [20] observed similar incidence of adverse events. Klimscha W et al., [7] noticed discomfort in 2 patients of CSA group due to inability to move their legs during postoperative analgesia which could be due to the use of micro catheters which usually results in maldistribution of drug. Lundorff L et al., [15] noticed PDPH in 1 patient (3.84%) in CSA group and unilateral paraesthesia in operative lower limb in 2 patients (7.69 % in CSA and 6.66 % in SSSA) in each group experienced which was explained by trauma during the needle-catheter placement and ischemic disturbances due to surgery. Minville V et al., [12] observed significantly higher incidence of hypotension and severe hypotension in SSSA group than CSA group which might be due to inclusion of ASA grade II-IV patients with various co-morbidities. Parthasarathy S et al., [1] noticed PDPH in 2 patients which resolved within 2 days with oral analgesics which might be due to use of larger bore 16 G needle and 18 G catheters for CSA. Imbelloni LE et al., [21] found higher incidence of arterial hypotension (3.41%) and PDPH (2.33%) in CSA group, respectively which could be due to the larger proportion of elderly females in their study. Bradycardia (5.95%) was also observed which might be due to fentanyl used for premedication in all patients.
In our study, mean volume of fluid administered was statistically higher in SSSA group than in Group CSA (p=0.0176). None of the patient in CSA group required vasopressor while 4 (18.18%) patients in SSSA group required total 12 mg of Mephentermine for the management of hypotension. Studies of Klimscha W et al., [7], Favarel-Garrigues JF et al., [8], Saber R et al., [14], Baydilek Y et al., [17], Minville V et al., [12], Andres JD et al., [13] showed comparable results which could be because of similar pattern of administration of drug aliquots and preloading. Lundorff L et al., [15] found higher consumption of ephedrine in SSSA group which could be because of higher block level compared to CSA group.
Limitations of our study are small sample size, block restricted to T10 (lower level of block) & observational study, so the results of our study cannot be extrapolated to other surgeries requiring higher level of block. Also, in present study drug administration was not extended for post- operative analgesia. Hence, the same study can be conducted as randomized control trial using large sample size for surgeries requiring higher level of block and can be extended for post operative analgesia.
CONCLUSION
REFERENCES
- Parthasarathy S, Sheeba AJ (2015) Continuous Spinal Anesthesia: A Need for a Re?emergence? Asian journal of Pharmaceutical and clinical research 8: 50-53.
- Horlocker TT, McGregor DG, Matsushige DK, Chantigian RC, Schroeder DR, et al. (1997) Neurologic complications of 603 consecutive continuous spinal anesthetics using macrocatheter and microcatheter techniques. Perioperative Outcomes Group. Anesth Analg 84: 1063-1070.
- Anon [online]: https://scholar.cu.edu.eg/sites/default/files/eslamayman/ files/updates_in_continuous_spinal_anesthesia_-_eslam_ayman. [Accessed 12 Aug. 2018]
- Denny NM, Selander DE (1998) Continuous spinal anaesthesia. British Journal of Anaesthesia 81: 590-597.
- Dripps RD (1950) A comparison of the malleable needle and catheter technics for continuous spinal anesthesia. N Y State J Med 50: 1595-1599.
- Hurley RJ, Lambert DH (1990) Continuous spinal anesthesia with a microcatheter technique: preliminary experience. Preliminary experience. Anesth Analg 70: 97-102.
- Klimscha W, Weinstabl C, Ilias W, Mayer N, Kashanipour A, et al. (1993) Continuous spinal anesthesia with a microcatheter and low-dose bupivacaine decreases the hemodynamic effects of centroneuraxis blocks in elderly patients. Anesth Analg 77: 275-280.
- Favarel-Garrigues JF, Sztark F, Petitjean ME, Thicoïpé M, Lassié P, et al. (1996) Hemodynamic effects of spinal anesthesia in the Elderly: Single dose versus titration through a catheter. Anesth Analg 82: 312-316.
- Pitkanen M, Rosenberg P, Silvanto M, Tuominen M (1992) Haemodynamic changes during spinal anaesthesia with slow continuous infusion or single dose of plain Bupivacaine. Acta Anaesthesiol Scand 36: 526-529.
- Compostella F, Seraglio P (2001) Continuous Spinal Anaesthesia (CSA) With Ropivacaine In Patients Undergoing Orthopaedic Surgery: Preliminary Report. The third European congress of orthopaedic anaesthesia, London, UK.
- Maurer K, Bonvini JM, Ekatodramis G, Serena S, Borgeat A (2003) Continuous spinal anesthesia/analgesia vs. single-shot spinal anesthesia with patient-controlled analgesia for elective hip arthroplasty. Acta Anaesthesiol Scand 47: 878-883.
- Minville V, Fourcade O, Grousset D, Chassery C, Nguyen L, et al. (2006) Spinal anesthesia using single injection small-dose bupivacaine versus continuous catheter injection techniques for surgical repair of hip fracture in elderly patients. Anesth Analg 102: 1559-1563.
- Andrés JD, Bellver J, Bolinches R (1994) Comparison of continuous spinal anaesthesia using a 32-gauge catheter with anaesthesia using a single-dose 24-gauge atraumatic needle in young patients. Br J Anaesth 73: 747-750.
- Saber R, Metainy SE (2015) Continuous spinal anesthesia versus single small dose bupivacaine–fentanyl spinal anesthesia in high risk elderly patients: A randomized controlled trial. Egyptian Journal of Anaesthesia 31: 233-238.
- Lundorff L, Dich-Nielsen OJ, Laugesen H, Jensen MM (1999) Single-dose spinal anaesthesia versus incremental dosing for lower limb vascular surgery. Acta Anaesthesiol Scand 43: 405-410.
- Fettes PDW, Hocking G, Peterson MK, Luck JF, Wildsmith JAW (2005) Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth 94: 107-111.
- Baydilek Y, Yurtlu BS, Hanci V, Ayoglu H, Okyay RD, et al. (2014) The comparison of levobupivacaine in continuous or single dose spinal anesthesia for transurethral resection of prostate surgery. Braz J Anesthesiol 64: 89-97.
- Seetharam KR, Bhat G (2015) Effects of isobaric ropivacaine with or without fentanyl in subarachnoid blockade: A prospective double-blind, randomized study. Anesth Essays Res 9: 173-177.
- Ebied RS, Ali MZ, Khafagy HF, Maher MA, Samhan YM (2016) Comparative study between continuous epidural anaesthesia and continuous Wiley Spinal® anaesthesia in elderly patients undergoing TURP. Egyptian Journal of Anaesthesia 32: 527-533.
- McNamee DA, McClelland AM, Scott S, Milligan KR, Westman L, et al. (2002) Spinal anaesthesia: comparison of plain ropivacaine 5 mg ml(-1) with bupivacaine 5 mg ml(-1) for major orthopaedic surgery. Br J Anaesth 89: 702-706.
- Imbelloni LE, Gouveia MA, Cordeiro JA (2009) Continuous spinal anesthesia versus combined spinal epidural block for major orthopedic surgery: prospective randomized study. Sao Paulo Med J 127: 7-11.
Citation: Jain SP, Rashmi N, Chandrapal B, Kumar GR (2019) Effect of Continuous Spinal Anesthesia and Single Shot Spinal Anesthesia on Hemodynamics for Lower Abdominal and Hip Surgeries in Adults: An Observational Study. J Anesth Clin Care 6: 39.
Copyright: © 2019 Shah Pratibha Jain, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

