
General Anesthesia for an Oral Surgical Procedure in a Patient with Severe Heart Valve Disease Scheduled for Cardiac Surgery: A case report
*Corresponding Author(s):
Hitomi SatomiDepartment Of Anesthesiology, Nihon University School Of Dentistry, Tokyo, Japan
Tel:+81 332198140,
Fax:+81 332198357
Email:satomi.hitomi@nihon-u.ac.jp
Abstract
For patients with cardiac disorders and oral diseases who require surgery, oral treatment sometimes precedes cardiac surgery. We report management of general anesthesia for an oral surgery in a patient who had severe Aortic Stenosis (AS) and severe Mitral Regurgitation (MR) requiring cardiac surgery, a coexisting chronic renal failure on dialysis. The patient was a 56-year-old man diagnosed with severe AS and MR who had received hemodialysis for chronic renal failure. Due to coexisting severe periodontitis, dental caries, and radicular cysts, he received oral surgery under general anesthesia before cardiac surgery. Strict circulatory management was necessary for this patient. Arterial Pressure-Based Cardiac Output (APCO; Flo Trac/VigileoTM; Edwards Lifesciences, Irvine, CA, USA) was useful for more strict circulatory management of critical heart valve disease such as this patient.
Keywords
APCO (arterial pressure-based cardiac output); General Anesthesia; Heart Valve Disease; Cardiac Surgery
INTRODUCTION
In cases of oral lesions in patients with valvular heart disease scheduled for a cardiac surgery, the oral treatment may be prioritized to prevent odontogenic infections [1]. We managed general anesthesia for an oral surgical procedure in a patient who was suffering from severe Aortic Stenosis (AS), severe Mitral Regurgitation (MR) and a coexisting chronic renal failure on dialysis. The patient was receiving maintenance dialysis and was scheduled for a cardiac surgery. In this case, strict intraoperative circulation management was necessary because the incidence of complications such as intraoperative death and nonfatal myocardial infarction in patients with severe AS undergoing noncardiac surgery is up to 31%, the key points of circulation management for both severe AS and MR are different, and the excessive or insufficient intraoperative circulating blood volume tends to occur in patients on dialysis [2-5]. Accordingly, general anesthesia was well managed through an active intraoperative circulation evaluation with a detailed anesthesia plan and Arterial pressure-based cardiac output (APCO; Flo Trac/VigileoTM; Edwards Lifesciences, Irvine, CA, USA). We hereby present a report of this case.
CASE REPORT
Patient status
The patient was a 56-year-old male with body height and body weight of 162.4 cm and 47.6 kg, respectively. In terms of medical history, he was diagnosed with hypertension and a coexisting chronic renal failure on dialysis at 40 years of age and was receiving hemodialysis (3 times a week). Subsequently, at 55 years of age, he was diagnosed with AS and MR and scheduled for aortic and mitral valve replacement. He was prescribed with omeprazole, rebamipide, precipitated calcium carbonate, etizolam, triazolam, and mianserin hydrochloride and olmesartan medoxomil. His present dental condition included severe periodontitis and radicular cysts associated with both maxillary canines and the right maxillary first premolar and first molar as well as right mandibular second molar. Thus, he was scheduled for multiple tooth extraction and radicular cystectomy.
Preoperative Blood Pressure (BP) and Heart Rate (HR) at rest were 145/88 mmHg and 98 beats/min, respectively. In addition, preoperative blood test showed the following abnormalities: Hemoglobin (Hb):10.1 g/dL, Hematocrit (Hct):9.8%, Blood Urea Nitrogen (BUN):45.7 mg/dL, and Creatinine (Cr):10.18 mg/dL. Moreover, electrocardiography indicated left ventricular hypertrophy. He didn’t have myocardium ischemia on the myocardial perfusion scintigraphy, and the pulmonary congestion was not detected in his chest X-ray (Figure 1). Transthoracic echocardiography revealed a left ventricular ejection fraction of 60%. Wall motion disorder and heart failure were not confirmed, but the patient was diagnosed with severe AS and grade III MR (Figure 2) (Table 1). Although he did not have syncope history, he had exertional dyspnea. New York Heart Association functional classification was class II and American Society of Anesthesiologists physical status was class III, respectively. In this case, because his cardiac function was kept, we decided to prioritize the oral surgery to prevent postoperative endocarditis of aortic and mitral valve replacement [6].
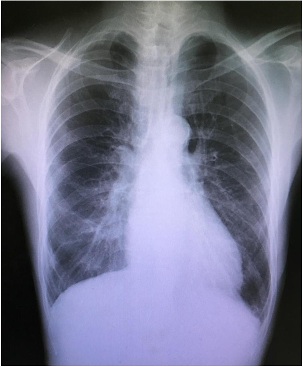 Figure 1: Chest X-ray before operation.
Figure 1: Chest X-ray before operation.
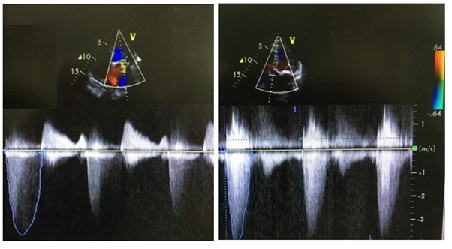 Figure 2: Echocardiography pictures of the aortic valve (light) and the mitral valve (left).
Figure 2: Echocardiography pictures of the aortic valve (light) and the mitral valve (left).
|
Valve |
Valve area (cm2) |
Mean pressure gradient (mmHg) |
Peak pressure gradient (mmHg) |
Regurgitant volume (ml) |
Peak velocity (cm/sec) |
Effective regurgitant orifice area(cm2) |
|
Aortic valve |
0.62 |
42.2 |
82.4 |
None |
453.9 |
None |
|
Mitral valve |
1.68 |
None |
None |
62 |
None |
0.41 |
|
The mobility of the anterior cusp is barely kept. |
||||||
Table 1: Echocardiographic findings of the aortic and mitral valves.
Severe Aortic Stenosis (AS): Valve area < 0.6 cm2, Mean pressure gradient≥40 mmHg, Peak velocity≥400 cm/sec.
Severe mitral Regurgitation (MR): Regurgitant volume≥60 ml, Effective regurgitant orifice area≥0.4 cm2.
ANESTHESIA PLAN
In this case, as fatal circulatory failure could have occurred intraoperatively, the procedure was performed under general anesthesia with local anesthesia to correspond with the strict intraoperative circulation management and resuscitation in such complication. To prevent endocarditis, cefazolin 1g was used in intravenous administration preoperatively. Anesthesia was induced with fentanyl in divided administration as well as midazolam, and nasotracheal intubation was scheduled after the administration of rocuronium. For anesthesia maintenance, taking into consideration a coexisting chronic renal failure on dialysis, a continuous administration of remifentanil and sevoflurane was scheduled. Moreover, as the surgical field covered the full jaw and the amount of anesthetic used was predicted to be large, the local anesthetic selected was 1% lidocaine with 1:400000 adrenalines. Kalium-free infusion solution was used, and based on the amount of fluid removed during the preoperative dialysis, the maximum intraoperative dose was set at 800 ml. Additionally, in consultation with the nephrologist and cardiologist, the preoperative dialysis was performed 2 days before the operation while prioritizing the maintenance of the intraoperative circulating blood volume. In addition to 5-lead electrocardiography, the indirect and direct arterial BP and Central Venous Pressure (CVP); APCO, which can evaluate Cardiac Output (CO); Systemic Vascular Resistance (SVR); and Stroke Volume Variation (SVV), an indicator of the circulating blood volume, were used for circulation evaluation. Furthermore, to prepare for unexpected situations, we requested for emergency dialysis and a cardiologist to be on standby.
ANESTHESIA PROGRESS
When entering the operation room, the patient’s BP and HR were 160/85 mmHg and 93 beats/min, respectively. Before anesthesia induction, an arterial-line was inserted into the right radial artery under local anesthesia following the circulation evaluation with APCO was initiated. Anesthesia was induced with 0.3 mg fentanyl in divided administration and 3 mg midazolam. Furthermore, the patient underwent nasotracheal intubation after the administration of 50 mg of rocuronium. Hemodynamics were stable around the induction. After anesthesia induction, a central venous catheter was inserted into the right internal jugular vein, and the CVP was measured. Anesthesia was maintained with 2 L/min of oxygen, 3 L/min of air, 1.5%-3.0% sevoflurane, and 0.1-0.3 µg/kg/min of remifentanil, and the partial pressure of end-tidal carbon dioxide was maintained at 40 mmHg by controlled respiration. In addition, a total of 5.6 mL of local anesthetics was implemented to the upper and lower jaws and the procedure began. The intraoperative BP and HP were constantly stable at about 110/70 mmHg and 60 beats/min, respectively. However, during maxillary teeth extraction, these reduced to 70/38 mmHg and 52 beats/min, respectively (Figure 3). In terms of the circulation indicators (Table 2(A)), SVV showed a low normal value; SVR, SVR index, and CVP were at the upper limit of the normal value; and SV, CO, and CI were at the lower limit of the normal value. Consequently, the circulating blood volume and SVR were well maintained, and the decrease in the CO was determined as the main factor of hypotension, so a total of 4 mg of ephedrine was given with 2 mg per administration. The circulation indicators 5 min after ephedrine administration are shown in table 2(B). Hemodynamics was stable until the end of the procedure, anesthesia awakening was good, and the patient was sent to the intensive care unit after extubation. The surgery and anesthesia durations were 130 min and 225 min, respectively. The total infusion and bleeding volumes were 450 mL and 127 g, respectively. The postoperative course was good, and the patient was temporarily discharged 4 days later, with a heart valve replacement scheduled in 2 months.
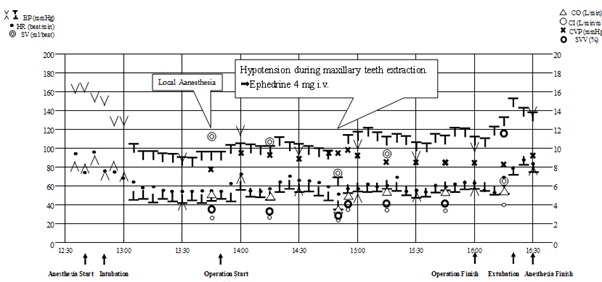
Figure 3: General anesthesia records.
BP: Blood Pressure (invasive or non-invasive), HR: Heart Rate, SV: Stroke Volume,
CO: Cardiac Output, CI: Cardiac Index, CVP: Central Venous Pressure, SVV: Stroke Volume Variation.
|
Hemodynamic parameter |
A |
B |
|
Blood pressure (systolic/diastolic, mmHg) |
70/38 |
115/55 |
|
Heat rate (beats/min) |
52 |
59 |
|
Stroke volume (mL/beat) |
76.9 |
91.5 |
|
Cardiac output (L/min) |
4 |
5.4 |
|
Cardiac index (L/min/m2) |
2.6 |
3.5 |
|
Stroke volume variation (%) |
4 |
6 |
|
Systemic vascular resistance (dynes/sec/cm5) |
1480 |
1615 |
|
Systemic vascular resistance index (dynes/sec/cm5/m2) |
2200 |
2400 |
|
Central venous pressure (mmHg) |
10 |
11 |
Table 2: Hemodynamics at hypotension onset and 5 min after ephedrine administration.
A: At the time of hypotension onset.
B: Five min after ephedrine administration.
DISCUSSION
The occurrence rate of Infective Endocarditic (IE) has been reported to be 3-10 per 100,000 people, among which 10%–20% are related to oral bacteria [7-8]. Therefore, dental treatment before cardiac surgery is important for the infective endocarditic prevention [1]. In this case, we also prioritized oral surgery over cardiac surgery and performed it under general anesthesia.
Anesthesia risk for this patient was severe AS and MR as well as a coexisting chronic renal failure on dialysis. The patients with AS are prone to myocardial ischemia due to the hypotension-induced decrease in the coronary flow, so the SVR should not be reduced. In addition, 50-70 beats/min HR value is desirable to maintain the systolic time when passing through the stenosed aortic valve [3]. Contrarily, the patients with MR have a higher risk of heart failure due to a CO decrease of the systemic circulation since an increase of the regurgitation volume by bradycardia and afterload increase. Therefore, it is necessary to keep the SVR low and maintain the HR at a normal to rather high value [3]. And, to keep the CO in the case of AS and MR, it is important to maintain the myocardial contraction. Due to preoperative dialysis and infusion restrictions, patients on dialysis are prone to excessive or insufficient circulating blood volume, which is a significant regulatory factor of circulation [5]. Based on the aforementioned, it was necessary to individually evaluate the circulation parameters, such as CO, SVR, and circulating blood volume, for the circulation management in this case.
In this case, BP decreased during the operation. Usually, when dealing with hypotension in the cases of combined AS and MR, AS is prioritized, which tends to be more fatal, and the first intervention is to administer α-stimulants, such as phenylephrine, to maintain SVR [4]. Meanwhile, at the low blood pressure in this case, based on the circulation evaluation with APCO, we were able to judge the CO drop due to the myocardial contraction drop, and the addition of infusion and phenylephrine administration has been avoided, and the intervention for hypotension through ephedrine administration was selected. Aside from BP recovery, SV, CO, and CI increased to appropriate values, and based on these results, we could be inferred that the selection of intervention for hypotension was appropriate. The indications of APCO for various valvular diseases have been widely discussed, but the respective effectiveness of AS and MR has been previously reported [9,10], circulation evaluation with the APCO in the cases of combined AS and MR seemed to be effective.
In principle, preoperative dialysis is performed on the day before the surgery [4]. However, in this case, because the scheduled surgery time was short and the possibility of both intraoperative fluid overload and blood transfusion were low, the priority was given to the prevention of intraoperative circulatory failure due to excessive circulating blood volume insufficiency. Thus, preoperative dialysis was performed 2 days before the operation. This judgement would contribute to the maintenance of the sufficient intraoperative circulating blood volume in CVP and SVV evaluation.
To avoid the effects of adrenaline on the circulation as much as possible, 1% lidocaine with adrenaline content adjusted to 1:400000 was used for local anesthesia in this case. However, for patients suffering from circulatory system diseases, 2% lidocaine with 1:200000 adrenalines has been recommended as the local anesthetic to prevent its effects on the cardiovascular system while achieving sufficient hemostatic and anesthetic effects [11]. Thus, a thorough and detailed discussion might be necessary, including the advisability of adrenaline use in the selection of local anesthetics, with the surgeon before the operation.
In conclusion, for patient with cardiac disorders and oral diseases, dental treatment before cardiac surgery is significant for the IE prevention. We managed general anesthesia for an oral surgical procedure in a patient with a coexisting chronic renal failure on dialysis and severe heart valve diseases scheduled for a cardiac surgery. It was well managed through a detailed anesthesia plan and strict intraoperative circulation evaluation with APCO for this patient.
ACKNOWLEDGEMENT
This study was supported by Sato Fund, Nihon University School of Dentistry.
REFERENCES
- Souza AF, Rocha AL, Castro WH, Ferreira FM, Gelape CL, et al. (2016) Dental care before cardiac valve surgery: is it important to prevent infective endocarditis? Int J Cardiol Heart Vasc 12: 57-62.
- Kertai MD, Bountioukos M, Boersma E, Bax JJ, Thomson IR, et al. (2004) Aortic stenosis: an underestimated risk factor for Perioperative complications in patients undergoing noncardiac surgery. Am J Med 116: 8-13.
- Paul A, Das S (2017) Valvular heart disease and anaethesia. Indian J Anaesth 61: 721-727.
- Christ M, Sharkova Y, Geldner G, Maisch B (2005) Preoperative and perioperative care for patients with suspected or established aortic stenosis facing noncardiac surgery. Chest 128: 2944-2953.
- Kanda H, Hirasaki Y, Iida T, Kanao-kanda M, Toyama Y, et al. (2017) Perioperative management of patients with end-stage renal disease. J Cardiothorac Vasc Anesth 31: 2251-2267.
- Kyo S, Imanaka K, Masuda M, Miyata T, Morita K, et al. (2017) Guidelines for Perioperative Cardiovascular Evaluation and Management for Noncardiac Surgery (JCS 2014). Circ J 81: 245-267.
- Selton-Suty C, Célard M, Moing VL, Doco-Lecompte T, Chirouze C, et al. (2012) Preeminence of staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis 54: 1230-1239.
- Rosa MRM, Cosano LC, Perez MJR, Cutando A (2014) The bacteremia of dental origin and its implications in the appearance of bacterial endocarditis. Med Oral Patol Oral Cir Bucal 19: 67-73.
- Lorsomradee S, Lorsomradee S, Cromheecke S, De Hert SG (2007) Uncalibrated arterial pulse contour analysis versus continuous thermodilution technique: effects of alterations in arterial waveform. J Cardiothorac Vasc Anesth 21: 636-643.
- Tamura T, Yatabe T, Yamashita K, Yokoyama M (2013) Management of anesthesia for pheochromocytoma in a patient complicated with severe mitral regurgitation. The Journal of Japan Society for Clinical Anesthesia 33: 815-819.
- Karm MH, Kim M, Park FD, Seo KS, Kim HJ (2018) Comparative evolution of the efficacy, safety, and hemostatic effect of 2% lidocaine with various concentration of epinephrine. J Dent Anesth Pain Med 18: 143-149.
Citation: Satomi H, Hirose N, Oka S, Oi Y (2020) General Anesthesia for an Oral Surgical Procedure in a Patient with Severe Heart Valve Disease Scheduled for Cardiac Surgery: A case report. J Anesth Clin Care 7: 55.
Copyright: © 2020 Hitomi Satomi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

