Inhaled Sevofluran vs Endovenous Propofol for Sedation Maintenance in Patients Submitted to Colonoscopy
*Corresponding Author(s):
Leopoldo WulffAnesthesiologists, Endoscopy Unit Of Centro Médico Docente La Trinidad, Caracas, Venezuela
Tel:+58 4143264549,
Email:leowulff@yahoo.com
Abstract
Introduction
Endoscopic procedures under sedation currently occupy an important place. Sedation allows optimal conditions for the study.
Objective
To compare the anesthetic efficacy of the inhalation versus intravenous technique for maintenance of sedation in patients undergoing endoscopy.
Materials and methods
A longitudinal, randomized clinical study of 32 patients of both sexes ASA I-III, aged 18-80 years undergoing diagnostic colonoscopy, which was randomly divided into 2 groups. In both, intravenous induction with propofol (2-2.5 mg / kg) was performed, Group A remained sedated with propofol infusion (1-2 mg / kg / min); Group B by inhalation with sevoflurane at a concentration of 2 vol% through a nasal cannula with an oxygen flow.
Results
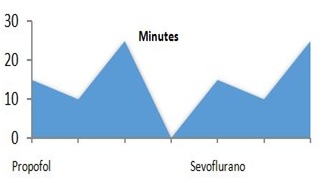
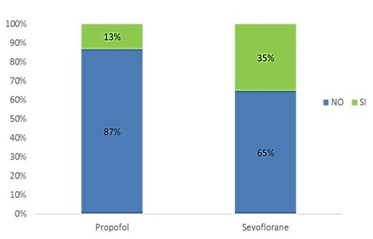
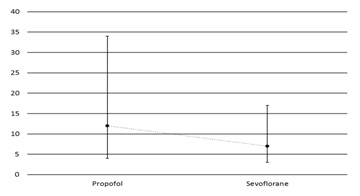
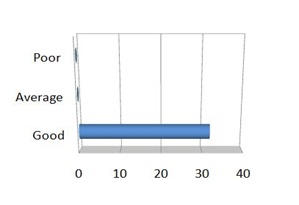
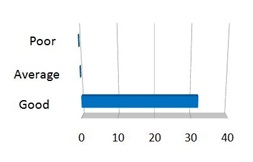
Both techniques were performed without registering complications; group A comprised of 15 patients in which only 13% required rescue bolus and a wake-up time of 12 minutes. The group B consisted of 17 patients, with a wake-up time of 7 minutes in whom 35% required salvage bolus.
Conclusion
Both anesthetic techniques proved to be safe and effective; patients receiving sevoflurane shortened their stay by 50% in the recovery of the endoscopic unit. Patients who only received propofol presented greater anesthetic depth required a lower rate of rescue boluses. Both techniques evidenced a good comfort level in both the patients and gastroenterologists.
Keywords
BACKGROUND
The endoscopic procedures under sedation currently occupy an important place in the diagnosis and treatment of pathologies of the digestive system. Sedation allows optimal conditions for the exploration and study, better control over the course of the procedure, reduction of the sympathetic response of the patient and a significant decrease in the time spent in the same, to have a patient much more collaborative and calm so the operator can perform a more complete examination.
Colonoscopy, also known as lower digestive endoscopy, involves the endoscopic exploration of the large intestine, from the anus to the ileocecal valve [1]; this is considered an outpatient procedure, the reason for why it is essential to use an anesthetic technique that includes fast metabolizing drugs, easy elimination and with the lowest incidence of complications, which allows early discharge of the patient. The intravenous anesthetic technique is the most commonly used; despite its effectiveness, it has multiple implications that are not very beneficial for the patient, which is why, to maintain effective sedation and the search for an alternative, the use of the inhalation route has recently been taken into consideration. Among the multiple benefits of its use we can achieve a quicker wake-up once the study is finished, with fewer systemic implications, making the study even easier providing greater comfort for the patient, the gastroenterologist and the anesthesiologist.
It is usually much more common in sedation protocols in areas outside the operating room (especially in the performance of digestive endoscopy studies) to use the intravenous route. Propofol stands out as the hypnotic drug of choice, becoming in recent years the most used for the realization of this type of procedure, due of the high margin of safety it has from the respiratory and cardiovascular point of view, offering to the patient a better safety profile reporting minimal complications with its use. However it has been described that prolonged infusions of this drug or infusions above 4 mg/kg/hour can cause deleterious effects on the organism producing hyperlipidemia states and what is known as the Propofol Infusion Syndrome which is a state critical characterized by bradycardia, metabolic acidosis, rhabdomyolysis, hyperlipidemia, hepatomegaly, hepatic steatosis [2] with its consequent multi organ failure, which can cause death in the patient; In addition to this, there have been reports of septicemia due to poor handling of propofol due to the presence of soybean oil and egg phospholipid as a vehicle used in its preparation, which represent a favorable medium for bacterial growth if not handled properly and based on the manufacturer's recommendations.
Taking into account that endoscopy procedures in gastroenterology, especially colonoscopies, require prolonged times for its correct performance, the administration of a halogenated agent is proposed, in this case, sevoflurane by inhalation in order to demonstrate that it is an equal method of cash for the maintenance of sedation without observing the complications described above with the prolonged use of propofol infusions, allowing the operator to perform the study in a more calm and detailed manner, offering benefits to all the people involved: both users and medical personnel in the endoscopy unit; this is where the importance of carrying out such a study lies in the fact that it is intended to provide another safe method for both the patient and the gastroenterologist, allowing the latter to complete the procedure with a high level of satisfaction.
From the medical point of view this work is of great importance since it guarantees greater safety for health personnel, allows the gastroenterologist to carry out the study without the limitation of suspending it when the maximum doses of propofol are being reached, avoiding complications before mentioned when this happens. In turn, the anesthesiologist represents an extra tool that can be used when performing sedation outside the surgical area, especially in patients with known hypersensitivity to any of the components of propofol, for example the egg. For the Institution, it would represent an additional advantage, having a safe therapeutic option and different from the classic intravenous route. In case of demonstrating the use of the inhalation route, as a safe and effective alternative in the anesthetic management of patients requiring prolonged procedures in ambulatory endoscopic units, it would favor the non-limitation that implies the use of a single anesthetic method of sedation and the consequent availability of this single drug used, which in most cases is propofol.
In the Centro Médico Docente La Trinidad digestive endoscopic diagnostic procedures are one of the most performed procedures, each time in more complex patients prolonging the time of performing them. This makes it necessary to suspend the procedure on many occasions due to the proximity of reaching toxic doses of propofol without the gastroenterologist being able to complete the entire study. In spite of not being the inhalation technique, a method commonly used in sedation, in some countries its study has been dedicated to it, De la Torre and collaborators made an experimental and prospective study, where they tried to compare the characteristics of the conventional technique of sedation in colonoscopies with intravenous propofol and an inhalation with sevoflurane [3].
On the other hand, Chun Hui Lan and colleagues conducted a study dedicated to reducing the discomfort and complications of patients undergoing upper gastrointestinal endoscopies by comparing the use of nitrous oxide with and without sedatives in upper gastrointestinal endoscopy. The authors conclude that in those patients deeply sedated in which they used the nitrous oxide mixture plus intravenous sedatives, the studies were more accurate in terms of diagnosis, they were significantly shorter in terms of time of completion and both patients and operators reported feeling more comfortable with this technique. However, more cases of complications were reported [4], which leads to the conclusion that it is not enough to administer an agent that guarantees analgesia only in these patients, so the hypnotic component must be given greater importance since it is better valued by the patient and the patient. gastroenterologist, but in turn get a drug that allows us to achieve the desired goal without the complications that arise from the use of them and the use of 2 or more anesthetic drugs in the management of patients especially in the outpatient settings.
OBJECTIVE
Specific objectives
- To evaluate the hemodynamic variability in patients between both techniques
- Determine the duration of the study
- Need to use rescue boluses against anesthetic superficialization
- Record adverse reactions in patients undergoing lower digestive endoscopy with both techniques
- Determine the patient's wake-up time after suspending maintenance
- To assess the level of satisfaction of the gastroenterologist with respect to the anesthetic technique
- Qualitatively assess patient comfort after sedation
MATERIALS AND METHODS
Research design
Working universe
Description of the variables
Anesthetic efficacy of the inhalation versus endovenous technique according to: hemodynamic behavior, duration of the study, oxygen saturation, rescue bolus requirements, time of awakening, satisfaction of the operator and patient in relation to sedation techniques during the study.
Independent variables
Lower digestive endoscopy, propofol and sevoflurane. They are qualitative variables, with a dichotomous qualitative measurement scale. Demographic (sex and age). Predictive (physical state according to ASA), operative, respiratory and hemodynamic.
Sample selection
Selection criteria
Age between 18 and 80 years, physical status I, II and III according to the criteria of the American Society of Anesthesiology (ASA), patients who are going to undergo diagnostic colonoscopies, have signed the informed consent.
Exclusion criteria
Allergy or hypersensitivity to some of the reference drugs in the study, patients with proven liver disease, suspicion or confirmation of pregnancy, antecedent or risk of malignant hyperthermia, fasting less than 8 hours, patients with psychic disorders or mental incapacity that make it difficult to understand their participation in the study, patients who have acute illnesses that compromise their health for which the study cannot be performed.
PROCEDURE
Graph 1: Sample characteristics.
Statistical analysis
RESULTS
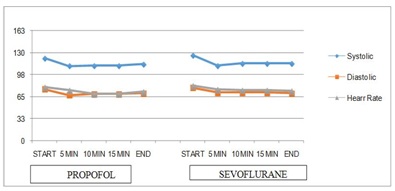
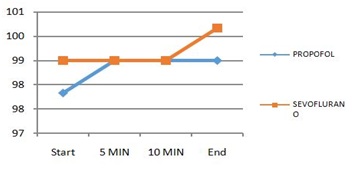
The group A (only received propofol) consisting of 15 patients of which 60% consisted of ASA II patients and 40% patients ASA I and group B (propofol plus sevoflurane) formed by 17 patients 65% ASA II and 35% ASA I (Table 1); both techniques not evidencing major respiratory complications during the study and demonstrating hemodynamic stability before, during and after the procedure. (Table 2, Graphs 2-4); however, a lower anesthetic depth was observed in group B since 35% of the patients required the use of rescue boluses with propofol to allow the continuity of the study compared to group A, which received only propofol, where a lower percentage of patients (13%) required rescue boluses (Graph 5). However, group B had a shorter time in the wake of their patients with an average of 7 minutes vs group A (propofol) with an average of 12 minutes, shortening the length of stay in the recovery of the endoscopy room in 50% approximately (Graph 6); 100% of patients and operators expressed satisfaction with both techniques; the average time of completion of the study was 15 min, there being no significant variations between both groups (Graphs 7,8).
|
Study Groups |
ASA I |
ASA II |
Total |
|
Propofol |
6 |
9 |
15 |
|
Sevoflurane |
6 |
11 |
17 |
|
Total |
12 |
20 |
32 |
Table 1: Classification of sample according ASA and study groups.
|
Previous to procedure |
Sistolic |
Diastolic |
Heart Rate |
SatO2 |
|
|
Propofol |
Average |
122 |
76 |
79 |
98 |
|
Min |
100 |
60 |
58 |
96 |
|
|
Max |
150 |
91 |
100 |
100 |
|
|
|
|
|
|
|
|
|
Sevoflurane |
Average |
126 |
78 |
81 |
99 |
|
Min |
100 |
60 |
50 |
95 |
|
|
Max |
177 |
90 |
110 |
100 |
|
|
|
|
|
|
|
|
|
5 minutes |
Sistolic |
Diastolic |
Heart Rate |
SatO2 |
|
|
Propofol |
Average |
110 |
67 |
74 |
99 |
|
Min |
100 |
59 |
60 |
97 |
|
|
Max |
120 |
82 |
92 |
100 |
|
|
|
|
|
|
|
|
|
Sevoflurane |
Average |
111 |
71 |
75 |
99 |
|
Min |
90 |
60 |
63 |
96 |
|
|
Max |
130 |
90 |
100 |
100 |
|
|
|
|
|
|
|
|
|
10 minutes |
Sistolic |
Diastolic |
Heart Rate |
SatO2 |
|
|
Propofol |
Average |
111 |
69 |
69 |
99 |
|
Min |
100 |
60 |
60 |
97 |
|
|
Max |
139 |
85 |
81 |
100 |
|
|
|
|
|
|
|
|
|
Sevoflurane |
Average |
111 |
71 |
74 |
99 |
|
Min |
90 |
60 |
60 |
99 |
|
|
Max |
130 |
90 |
97 |
100 |
|
|
|
|
|
|
|
|
|
After de procedure |
Sistolic |
Diastolic |
Heart Rate |
SatO2 |
|
|
Propofol |
Average |
113 |
70 |
72 |
99 |
|
Min |
100 |
54 |
59 |
97 |
|
|
Max |
121 |
80 |
82 |
100 |
|
|
|
|
|
|
|
|
|
Sevoflurane |
Average |
114 |
70 |
73 |
100 |
|
Min |
100 |
60 |
57 |
99 |
|
|
Max |
127 |
80 |
105 |
100 |
|
Table 2: Patients monitoring during sedations.
DISCUSSION
The patient that undergoes diagnostic or therapeutic digestive endoscopy studies represents an ideal candidate for anesthetic management through the administration of pharmacological agents which allow reducing anxiety and avoiding discomforts that may arise during the procedure. Therefore, both the duration and complexity of the endoscopic studies performed have increased significantly in recent years. For this reason, it is very important to carry them out with a more calm and collaborative patient, hemo-dynamically stable, making the colonoscopy a non-obnoxious exploration [3].
The search for the ideal anesthetic has been a constant in the contemporary history of medicine. The use of effective drugs, which allow to obtain an adequate sedation plan, with few or no adverse effects and which in turn guarantee the comfort of the patient and the surgeon during the study is what is required at present.
The propofol is an anesthetic drug that was developed with the aim of reaching these standards; at adequate doses by intravenous route and in experienced hands can provide a state of sedation according to the requirements required in the areas already described, more specifically during the performance of a colonoscopy [5]. For this reason, it has become the most used anesthetic drug for performing procedures in the ambulatory area since it has a high margin of hemodynamic safety; however, after its prolonged use serious complications have been described the use of the inhalation route as an effective and alternative method in the maintenance of sedation in endoscopic studies has been taken in consideration. In the constant process of renewal and research of anesthesiology in recent years, propofol has ceased to be the only drug used for these purposes losing its exclusivity more and more. Multiple drugs, both intravenous and inhaled, have been described in recent publications, with favorable results in these indications for most of them [6]. Gupta et al., conclude that those differences in early recovery times among the different anesthetics were small of the inhaled anesthetics [7].
In this investigation, all the demographic characteristics were homogeneous in the group of patients from the statistical point of view, which allows an adequate analysis. In relation to the duration of the study, our results differ from those obtained by Lan and colleagues, who found a decrease in the time of execution of the procedure of approximately 10 minutes in patients who were given inhalation anesthesia with N2O compared to patients deeply sedated intravenously [8]. In our study, the average times of study duration in both groups were approximately 15 minutes for both, finding no significant differences between them. This is probably due to the greater degree of sedation obtained by the inhalation agent we use, sevoflurane, which has very different pharmacokinetic and metabolic characteristics than N20, an inhaled anesthetic used by Lan et al. In relation to the hemodynamic variables, De La Torre et al., found a slight increase in heart rate during colonoscopy in patients treated with inhalation anesthesia with sevoflurane. The changes linked to this phenomenon are related to superficiality in the anesthetic technique, and discomfort on the part of the patient at the time of the procedure [3]. In the present investigation, there were no significant hemodynamic changes in the groups studied. The use of rescue boluses with intravenous propofol at a dose of 1 mg/kg in patients sedated with sevoflurane is an intravenous support in those patients who present anesthetic superficiality during the study [8]. In relation to this, our results are similar to those obtained by De La Torre et al., since the group represented by patients sedated by inhalation with sevoflurane required a greater number of boluses, 35% more than the sedated group via intravenous. This anesthetic superficiality is closely related to the examiner’s technique when carrying out rectification maneuvers of the colon [3]. Ghatge S et al., report sevoflurane as an effective, safe agent with low incidence of nausea and vomiting [9].
Important to mention the experience of Cohen et al., and Wemli et al., regarding the presence of adverse effects such as arrhythmias, hypotension and SO2 desaturation between both anesthetics, not presenting statistically significant differences between their study groups being hypotension the most described complication in both groups studied [6,10]. In our study groups, unlike Cohen et al., we found no significant hypotension during the procedure.
Finally we must highlight our results and those obtained by López and colleagues, which lead the author to confirm that propofol and sevoflurane are drugs with an adequate safety profile, which favor adequate spontaneous ventilation and decrease the recovery stay of patients, obtaining a somewhat different results since in our study the least stay was presented in patients sedated with sevoflurane as opposed to those with intravenous propofol, achieving the well-being and satisfaction of the patient and the endoscopist [11]. Likewise, Faga et al., mention the safety of propofol in cirrhotic patients undergoing colonoscopy and endoscopic retrograde cholangiography [12].
CONCLUSION
Both anesthetic techniques were found to be safe and effective for the study, without causing changes in the time of realization [13]; the awakening after sedation of the patients who received inhaled sevoflurane was significantly shorter than those who received only propofol reducing by 50% their stay in the recovery area. In those patients in whom only propofol was administered a much deeper anesthetic level was evidenced since only 13% of the patients required the use of rescue boluses unlike the group that received sevoflurane where it had been used in 35%, twice the number of patients when comparing with the group that only received propofol during the induction and maintenance of sedation.
To conclude, in all the patients a good level of satisfaction was demonstrated with both techniques, which makes sevoflurane a good strategy when performing sedation for lower digestive video diagnostic procedures.
REFERENCES
- Müller AD, Sonnenberg A (1995) Prevention of colorectal cancer by flexible endoscopy and polypectomy. A case-control study of 32,702 veterans. Ann Intern Med 123: 904-910.
- Kam PC, Cardone D (2007) Propofol infusion syndrom. Anesthesia 62: 690-701.
- De la Torre Carazo S y cols (2012) Anestesia para colonoscopia: anestesia inhalatoria con sevoflurano frente a anestesia intravenosa con propofol. Sanid mil 68: 1.
- Lan C, Shen X, Cui H, Liu H, Li P, et al. (2013) Comparison of nitrous oxide to no sedation and deep sedation for diagnostic upper gastrointestinal endoscopy. J Gastrointest Surg 17: 1066-1072.
- Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, et al. (2009) Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology 137: 1229-1237.
- Cohen LB, Delegge MH, Aisenberg J, Brill JV, Inadomi JM, et al. (2007) AGA Institute review of endoscopic sedation. Gastroenterology 133: 675-701.
- Gupta A, Stierer T, Zuckerman R, Sakima N, Parker SD, et al. (2004) Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: systematic review. Anesth Analg 98: 632-641.
- Hernández de la Vega, Leticia (2004) Sedación consciente e inconsciente. Revista mexicana de Anestesiologia 27: 95-97.
- Ghatge S, Lee J, Smith J (2003) Sevoflurane: and ideal agent for adult day-case anesthesia? Acta Anaesthesiol Scand 47: 917-931.
- Wemli KJ, Inadomi JM (2013) Anesthesia for Colonoscopy: Too Much a Good Thing? Comment on “Complications Following Colonoscopy With Anesthesia Assistance”. JAMA Intern Med 173: 556-558.
- López Rosés L, Subcomité de Protocolos de la Sociedad Española de Endoscopia Digestiva (SEED) (2006) Directrices “guidelines” de sedación/analgesia en endoscopia. Rev Esp Enferm Dig 98: 685-692.
- Faga E, De Cento M, Giordanino C, Barletti C, Bruno M, et al. (2012) Safety of propofol in cirrhotic patients undergoing colonoscopy and endoscopic retrograde cholangiography: results of a prospective controlled study. Eur J Gastroenterol Hepatol 24: 70-76.
- Riphaus A, Wehrmann T, Weber B, Arnold J, Beilenhoff U, et al. (2009) S3 Guideline: sedation for gastrointestinal endoscopy 2008. Endoscopy 41: 996-996.
Citation: Pérez-Díaz L, Wulff L, Salazar A, Amaro M, Álvarez J (2019) Inhaled Sevofluran vs Endovenous Propofol for Sedation Maintenance in Patients Submitted to Colonoscopy. J Anesth Clin Care 6: 32.
Copyright: © 2019 Luis Pérez Díaz, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.