Interdisciplinary Rotations in Residency Training: Impact on Airway Management Experience
*Corresponding Author(s):
Cheryl C NoconDepartment Of Surgery, Division Of Otolaryngology-Head And Neck Surgery, University Of Wisconsin, Madison, WI, United States
Tel:+1 6082630192,
Email:nocon@surgery.wisc.edu
Abstract
Background: The management of airway emergencies is often interdisciplinary, but there are limited data on the role of interdisciplinary emergency airway training.
Methods: The University of Chicago anesthesiology residency program requires an otolaryngology rotation for half of the first year residents. In order to determine the impact of such a rotation on emergency airway experience, we surveyed the residents about their training and clinical experiences.
Results: The survey had a 100% response rate. Residents who rotated on an otolaryngology service reported greater use of fiberoptic laryngoscopy (p=0.02) and greater surgical airway experience (p<0.0001) compared to those who did not. All residents reported infrequent performance of emergency surgical airway procedures. The differences in the number of airway emergencies in which they were involved in any capacity (p=0.08) or personally managed (p=0.05) did not reach statistical significance between the two groups. Self-reported confidence regarding emergency airway skills did not vary by otolaryngology rotation exposure (p=0.68). On a scale of 1 to 10 (10 = “totally competent”, 1 = “not competent at all”), the mean self-rated competence in handling airway emergencies was 6 versus 5.69 (p=0.67) for those who rotated on an otolaryngology service and those who did not, respectively. Seniority and a more extensive call schedule correlated with a higher self-assessment (p<0.001).
Conclusion: Interdisciplinary training is associated with increased airway management experience, but there is no difference in resident self-rated confidence and competence. This high confidence-low experience dichotomy may reflect novice overconfidence and suggests the need for improved training methods, especially given low exposure.
Keywords
INTRODUCTION
Airway management is a cornerstone of anesthesia practice, in particular the management of emergent and difficult airways. Unfortunately, airway emergencies are high-stress, high-risk, and time-pressured situations that often occur at night at times of lower staffing, making their management a difficult skill to teach. As a result, there are minimal data on the methods of training of anesthesiology residents in this area, despite widespread use of a number of educational methods, including formal airway rotations, use of mannequins for practice, animal and cadaver laboratory experiences, in-service training with relevant equipment, and simulation [1,2].
Emergency airway management is often also interdisciplinary. The adoption of airway management responsibilities by other specialties (e.g., otolaryngology, critical care, emergency medicine, trauma surgery) has resulted in various approaches to the emergent airway [3]. Interdisciplinary teamwork has been hailed as necessary to coordinate and maximize the talents and skills offered by other specialists [4]. However, there are limited data on the role of interdisciplinary emergency airway training.
A previous study by our group surveyed chief residents in Anesthesiology (ANES) and Otolaryngology-Head and Neck Surgery (OHNS), which revealed an association between interdisciplinary training and a higher self-rated competence in handling airway emergencies [5]. Such findings suggested that residents who rotate with different specialties during their training may feel more confident in this clinical arena.
In 2003, the University of Chicago (U of C) ANES residency program added an OHNS rotation for approximately half of the first year interns (Post-Graduate Year 1 [PGY-1]). We sought to determine the impact of such a rotation on airway management experience, confidence and self-rated competence. We hypothesized that those ANES residents who rotated on the OHNS service would have greater experience, increased confidence, and higher self-rated competence compared to those who did not.
METHODS
Survey methodology
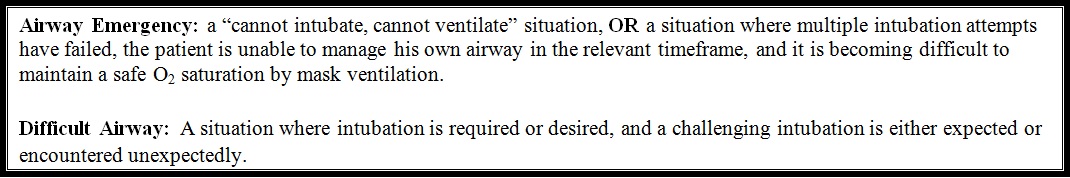
A survey was distributed to all ANES residents at the U of C (n=50). This included all PGY-2, PGY-3 and PGY-4 residents in 2008. ANES fellows (PGY-5) were included if they had completed their internship year at the U of C. Survey questions concerned training methods, call schedules, participation in airway emergencies, and self-assessment of training experiences and competence in handling airway emergencies and difficult airways (Supplementary Material, resident survey). The following definitions were provided in our survey for reference:
Airway emergency
A ‘cannot intubate, cannot ventilate’ situation OR a situation where multiple attempts to secure the airway have failed, the patient is unable to manage his own airway in the relevant timeframe, and it is becoming difficult to maintain a safe oxygen saturation by mask ventilation.
Difficult airway
A situation where intubation is required or desired, and a challenging intubation is either expected or encountered unexpectedly.
Approval from the Institutional Review Board at U of C was obtained.
Statistical analysis
Survey data was analyzed using SYSTAT software (Systat Software, Inc, Chicago, IL). Responses were categorized according to whether the residents had rotated on an OHNS service or not. They were analyzed separately and compared with each other to determine differences between the groups. Questions regarding the number of actual airway emergencies and surgical airways performed gave the respondents a range from which to choose (i.e., “1-2,” “3-5,” etc; see Supplementary Material). Therefore, numerical data on airway emergency participation and surgical airway performance is presented as the mode of reported ranges. Ranked variables were assessed using the Mann-Whitney U test, and binary variables were compared with the Chi-square test. We used Spearman rank correlation analysis to find significant correlations between a respondent’s answer to each question and that person’s self-rating of competence. Residents self-rated their competence to handle an airway emergency and a difficult airway on a scale of 1 to 10 (1=“not competent at all,” 10=totally competent”). Self-ratings are reported as the mean value. A p-value <0.05 was considered significant.
RESULTS
Responses
Surveys were completed by all 50 ANES trainees who had completed their internship at the U of C, giving a 100% response rate. The breakdown of responses by post-graduate year is given in figure 1. 24 survey respondents completed an OHNS rotation their internship year (OHNS+), and 26 did not (OHNS-).
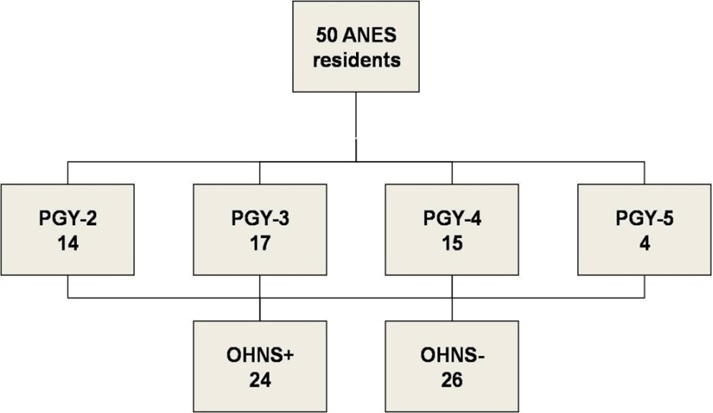
Figure 1: Survey responses of Anesthesiology (ANES) residents, broken down by Post-Graduate Year (PGY) and whether an Otolaryngology-Head and Neck Surgery (OHNS+) rotation was completed during internship year or not (OHNS-).
Training
Table 1 presents the list of training methods surveyed and the frequency of their use among OHNS+ and OHNS- groups. As expected, both groups frequently encountered routine intubations, printed materials, simple mannequins and supervised management of actual emergencies in training. Virtual reality tools, animal labs and unsupervised management of actual emergencies were rarely encountered by either group. There was a significant difference in the use of routine diagnostic fiberoptic laryngoscopy in the clinical setting (83% of OHNS+ versus 50% of OHNS- residents, p=0.02).
| OHNS+ | OHNS- | p-value | |
| Printed materials | 83% | 96% | 0.12 |
| Emergency/secondary techniques/equipment for routine intubations | 96% | 96% | 0.93 |
| Simple mannequins | 70% | 69% | 0.98 |
| Full scale computerized patient simulator | 17% | 27% | 0.43 |
| Virtual reality tools | 17% | 12% | 0.56 |
| Animal labs | 0% | 4% | 0.34 |
| Cadaver labs | 0% | 0% | 0.67 |
| Lectures | 83% | 85% | 0.85 |
| Videos | 43% | 42% | 0.93 |
| Supervised management of actual emergencies | 87% | 73% | 0.23 |
| Unsupervised management of actual emergencies | 13% | 4% | 0.24 |
| Routine diagnostic fiber optic laryngoscopy in clinical setting | 83% | 50% | 0.02 |
| Operative rigid direct laryngoscopy/bronchoscopy | 22% | 8% | 0.16 |
Table 1: Training methods in difficult and/or emergency airway management.
Clinical exposure
There was a trend toward a difference in the number of airway emergencies that residents participated in (i.e., resident involved in any capacity, figure 2). OHNS+ residents most frequently cited a range of “3-5” airway emergencies, compared to “1-2” by OHNS- residents (p=0.08). Only 25% of OHNS+ residents and 16% of OHNS- residents had participated in more than 5 airway emergencies (p=0.40), and 17% of OHNS+ and 4% of OHNS- residents had participated in more than 10 (p=0.13).
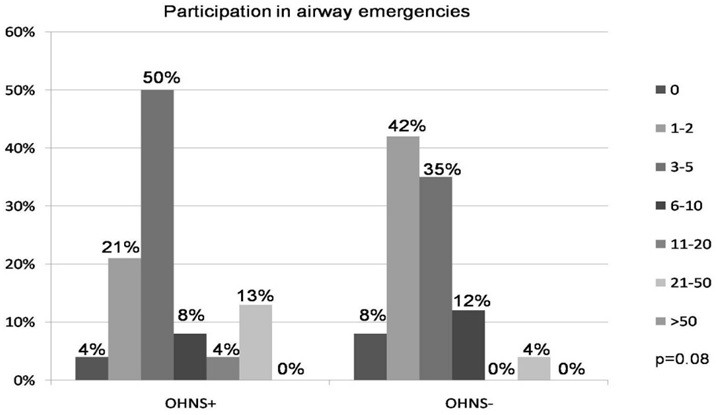
Figure 2: Airway emergencies that Anesthesiology residents participated in, categorized by whether an Otolaryngology-Head and Neck Surgery (OHNS+) rotation was completed during internship year or not (OHNS-). Surveys offered ranges of numbers of emergencies (i.e., 1-2, 3-5, etc.), and data is presented as the percentage of each range.
Similarly, there was no significant difference in the number of airway emergencies that residents personally managed (i.e., resident charged with securing the airway, (Figure 3). Residents from both groups most frequently cited a range of “1-2” airway emergencies (p=0.05). Only 29% of OHNS+ residents and 16% of OHNS- residents had personally managed more than 5 airway emergencies (p=0.24), and 16% of OHNS+ and 4% of OHNS- residents had personally managed more than 10 (p=0.13).
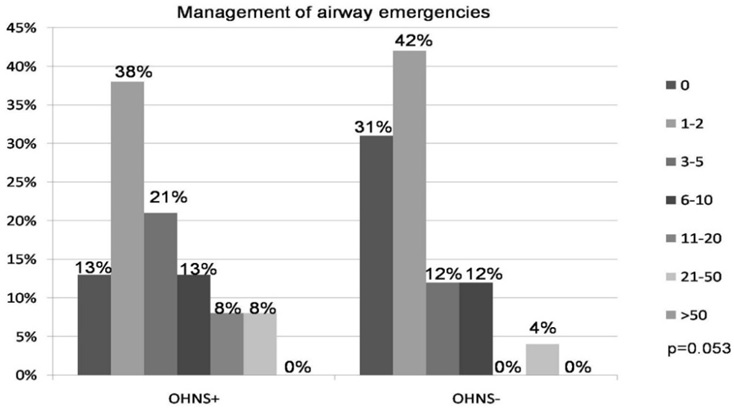
Figure 3: Airway emergencies that Anesthesiology residents personally managed, categorized by whether an Otolaryngology-Head and Neck Surgery (OHNS+) rotation was completed during internship year or not (OHNS-). Surveys offered ranges of numbers of emergencies (i.e., 1-2, 3-5, etc.), and data is presented as the percentage of each range.
Surgical airway experience
There was a significant difference in surgical airway experience between the two groups (Figure 4). 67% of OHNS+ residents had performed a surgical airway (elective or emergent) up to the time surveyed in their residency, compared to only 9% of OHNS- residents (p<0.0001). Perhaps more important is the percentage of residents who had not performed any surgical airways: 91% of OHNS- residents compared to only 33% of OHNS+ residents. This difference remained impressive even among senior residents (PGY-3 and PGY-4, data not shown).
Among residents who reported having performed any surgical airway during their training, there was no difference in the number of emergency surgical airways performed (emergency tracheostomy or cricothyrotomy, excluding planned awake tracheostomies) between groups. The most commonly reported number of emergency airways performed either on the OHNS service by OHNS+ residents, or on another service by the OHNS- residents, was “0” (p=0.95). Two OHNS+ residents reported performing emergency surgical airways on the OHNS service, citing frequencies of “1-2” and “3-5.” Two OHNS- residents also reported performing emergency surgical airways on another service (Trauma rotation), both reporting frequencies of “1-2.”
In contrast, there was a significant difference in the number of elective surgical airways performed (planned awake tracheostomy in a controlled setting). OHNS+ residents most commonly reported performing “6-10” elective surgical airways, compared to “0” by OHNS- residents (p<0.001). Among the OHNS- residents who had performed an elective surgical airway, two performed them while rotating on the ANES service (“1-2” and “3-5”) and two performed them while rotating on the Trauma service (both “1-2”).
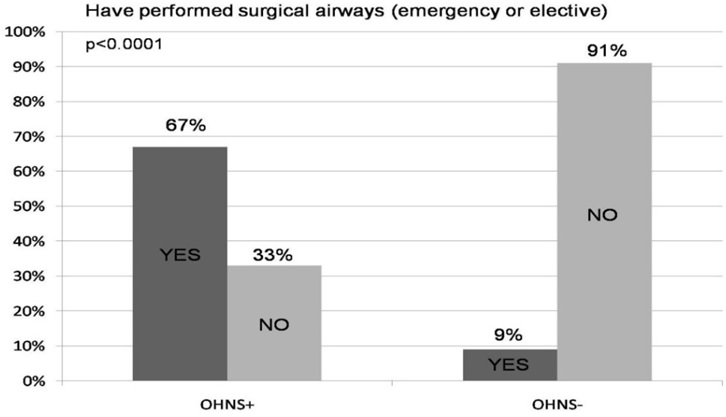
Figure 4: Elective and emergency surgical airways performed by Anesthesiology residents, categorized by whether an Otolaryngology-Head and Neck Surgery (OHNS+) rotation was completed during internship year or not (OHNS-).
Self reported confidence and competence
Resident confidence regarding their airway management experiences did not vary according to whether or not an OHNS rotation was completed (Figure 5). Only 29% of OHNS+ and 35% of OHNS- residents felt their residency training so far had afforded them an adequate experience and the opportunity to manage an adequate number of airway emergencies (p=0.68). On the other hand, 83% of OHNS+ and 77% of OHNS- residents felt their training had given them the opportunity to manage an adequate number of difficult airways (p=0.62). Among OHNS+ residents, an overwhelming 92% reported having gained clinical experience in emergency airway management not otherwise provided by the rest of their training.
Residents in both groups gave themselves average ratings for competence in managing airway emergencies. The mean self-rating for OHNS+ residents was 6, compared to 5.69 for OHNS- residents (p=0.67). OHNS+ residents gave themselves slightly higher ratings in managing difficult airways, though the difference was not significant (8 vs. 7.27, p=0.88).
We identified factors of resident training and experience that correlated with a higher self-rating of competence (Table 2). Seniority and a more extensive call schedule correlated with a higher self-assessment in handling both airway emergencies and difficult airways (p<0.001). Not surprisingly, citing an adequate exposure to airway emergencies during their training correlated with a higher self-rating in handling airway emergencies (p=0.002), and citing an adequate exposure to difficult airways correlated with a higher self-rating in handling difficult airways (p=0.03). Interestingly, there was no correlation between a higher self-rating in handling airway emergencies with having participated in (p=0.31) or having personally managed (p=0.07) a greater number of airway emergencies. The same was true for the difficult airway (p=0.73, p=0.75, respectively). There was also no correlation between confidence and having performed a surgical airway (p=0.81, during an airway emergency; p=0.89, during a difficult airway).
| Difficult Airways p-value | Airway Emergencies p-value | |
| Higher year of training | <0.001 | <0.001 |
| Greater number of PACU days on-call | <0.001 | <0.001 |
| Greater number of PACU nights on-call | <0.001 | <0.001 |
| Greater number of senior resident on-calls | <0.001 | <0.001 |
| Citing an adequate exposure to difficult airways | 0.03 | |
| Citing an adequate exposure to airway emergencies | 0.002 |
Table 2: Factors Correlating with a High Self-Assessment in Handling Difficult Airways and Airway Emergencies.
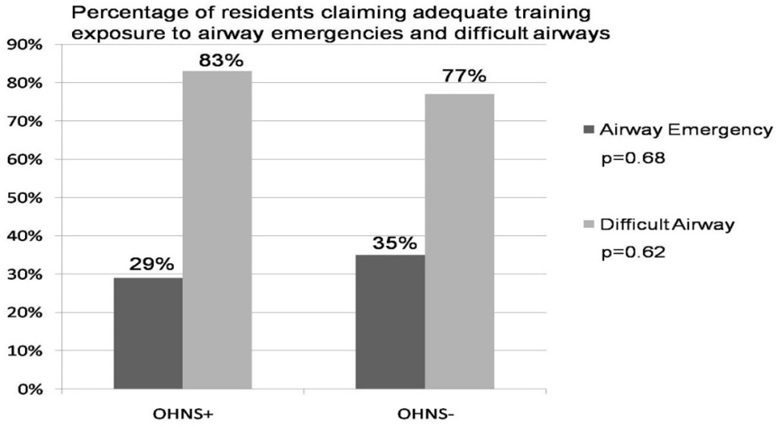
Figure 5: Anesthesiology resident confidence regarding airway emergency and difficult airway training, categorized by whether an Otolaryngology-Head and Neck Surgery (OHNS+) rotation was completed during internship year or not (OHNS-).
Resident feedback on airway management training
Residents were invited to provide written feedback on any aspect of their airway management training. Their responses can be separated into two broad categories of “Concerns” and “Recommendations.” Table 3 provides a sampling of the responses that were given. Their concerns reflect the relative rarity of airway emergencies in clinical practice, especially surgical airways, making it difficult to gain proficiency in their management. Specific recommendations include greater experience handling airway emergencies, whether through formal workshops and classes or through interdisciplinary training with the OHNS service.
Residents who completed an OHNS rotation their internship year were also asked for their feedback on the rotation (Table 3). The feedback was overwhelmingly positive, with most respondents finding the rotation instructive and educational. Some respondents offered suggestions on how to improve the rotation. These included more surgical airway experience and more work with specialized airway instruments.
| Regarding Airway Management Training | Regarding OHNS Rotation |
| Concerns | Comments |
|
|
| Recommendations | |
|
|
Table 3: Sampling of resident feedback.
DISCUSSION
Modern anesthesia training in airway management faces new challenges. Experience in techniques of airway management has steadily decreased as a result of exposure to fewer cases [6]. Traditional “on the job” training time also competes with other non-clinical aspects of resident training [7]. Furthermore, reduced resident work hours and the increased use of regional anesthesia techniques and supraglottic devices have reduced trainees’ exposure to endotracheal intubation and face mask ventilation [7].
It appears that this trend also affects training in emergency airway management. Whereas the incidence of failed tracheal intubation is relatively low at an estimated 1 in every 2230 non-obstetric patients, approximately 30% of all deaths attributed to anesthesia are related to difficult airway management [8]. The relative rarity of these critical events makes it difficult to ensure that residents gain enough experience in their actual management. Despite the importance of managing difficult and emergent airways, formal instruction under controlled scenarios has its limits, potentially resulting in variable and/or less than optimal training [6,9]. Studies of anesthesiology training experiences in different countries demonstrate similar findings [9-11]. Although the use of a percutaneous tracheostomy or cricothyrotomy is considered the final step in the difficult airway algorithm in many organizational guidelines, the topic of training is often neglected. Only Italian and Canadian guidelines for difficult airway management emphasize that rapid tracheal access should be an anesthesiologist’s core skill [12], and there have been recommendations to make performance of surgical airways a requirement in airway training for anesthesiologists [13].
The inconsistency in airway training may also be a reflection of the variable definitions of “airway emergency” and “difficult airway,”[14] and as a result, a difference in training emphasis among different specialties [15]. The fields of otolaryngology, emergency medicine, critical care, trauma and anesthesiology have different training priorities that reflect their specific clinical settings and patient populations. The emphasis on surgical versus non-surgical airway management techniques and adjuncts varies depending on the specialty. These differences in approaches suggest the potential benefit of interdisciplinary training.
Survey research can present certain limitations, including selection bias, recall bias, low response rates and faulty survey design. When obtaining numerical data on resident airway experience, we relied heavily on individual recollection. There was no procedure record/log against which we could confirm the responses provided. Although this precluded the comparison of actual numbers of airways, it nonetheless provided useful information regarding the training experiences of the two groups. We were also able to achieve a response rate of 100%. A study of response rates to e-mail surveys shows that since the initiation of such surveys in 1986, response rates have been trending downwards year-by-year [16]. Compared with the 31 academic surveys included in that study, our response rate of 100% compares favorably (range: 19% to 61%).
Our findings suggest the limitations of traditional apprenticeship training approaches when it comes to airway emergencies. Less than 20% of residents from both groups had participated in or personally managed more than 10 airway emergencies. This implies that throughout their training, residents have limited opportunities of participating in an airway emergency, let alone being in charge of one event. The number of emergency surgical airways is even more striking, with almost all of the residents reporting that they never performed one, even with the opportunity to rotate on an OHNS service where greater surgical airway exposure is expected. The fact that even some OHNS+ residents did not perform any surgical airways probably reflects the rarity of these events and/or the fact that more senior trainees or faculty manage these critical situations when life, death or significant morbidity is at stake.
One study demonstrated that even in a controlled environment, 96% of participants needed at least five attempts on a mannequin in order to perform a cricothyrotomy correctly in 40 seconds or less [17]. A recent survey study revealed that surgeons from all disciplines generally lack training and confidence in performing surgical airways, and only infrequently perform them in the operating room [18]. This has implications for the anesthesiologist, who cannot always rely on surgical colleagues to provide a surgical airway during a crisis. Accordingly, the authors suggest that anesthesia training should include surgical airway management.
In contrast to emergency surgical airways, elective surgical airways were performed significantly more often by residents who had rotated on an OHNS service. More importantly, they were performed while rotating on the OHNS service, demonstrating the value of an OHNS rotation in airway management training. At our institution, the goals of this month-long rotation are improved exposure to upper airway anatomy, training in endoscopy (awake flexible nasolaryngoscopy and anesthestized laryngoscopy and flexible and rigid bronchoscopy and esophagoscopy as part of head and neck cancer care), and exposure and training in surgical airways (primarily elective tracheotomy). This exposure is also reflected in the percentage of residents who had performed any type of surgical airway during their training. Strikingly, nearly all OHNS- residents never performed any surgical airway and even only 33% of OHNS+ did so. This difference remains salient throughout their training, such that PGY-4 residents who never rotated on an OHNS service are now graduating residency without ever having performed a single surgical airway. The limited exposure during residency is perhaps a consequence of an overall decline in the use of surgical airways [19,20], a phenomenon that should compel program directors to reconsider how its trainees will gain the necessary experience before graduation [21]. Thus, the PGY1 OHNS rotation and subsequent experiences in the ANES residency are complimentary.
Despite disparate OHNS training experiences, most ANES residents believe their difficult airway experience has been adequate, and rate their own competence highly. On the other hand, most ANES residents believe their airway emergency experience has not been adequate. Nonetheless, most rate their own competence as slightly above average.
This suggests that either residents are truly competent or they are overconfident. In the first case, one concludes that airway emergency training is adequate and that residents are heading into practice with high levels of skill in dealing with this critical clinical situation. Clinical experience and prior study [22,23], however, reveal that airway management problems remain a source of preventable morbidity and mortality, with improved training as one potential remedy [24-26]. In the second case, one supposes that residents are graduating full of confidence, but with their inexperience, they do not have the competence they think they have, and possibly suffer from “novice overconfidence.” Such a discrepancy in airway experience and confidence was previously demonstrated in chief residents in ANES and OHNS [5].
Several studies in different domains of proficiency have compared self-assessed competence with competence assessed by an expert observer [27]. Most studies show a weak to moderate correlation between self-assessment and independently-judged skill [28-30]. This cognitive bias toward an overestimation of one’s abilities has been well-studied in the Social Psychology literature and is known as the Kruger-Dunning effect [31]. Interestingly, it is only with improved competence that participants are able to recognize the limitations of their abilities.
This high confidence-low experience dichotomy calls for effective training methods to address the experience deficit and improve competency levels. The low-frequency, high-impact nature of airway emergencies, however, makes it difficult to study the impact of training on patient outcomes. Certainly training exposure is important, as evidenced by the correlation between a higher self-rated competence handling airway emergencies and year of training and greater call experience. However, only 29% of OHNS+ and 35% of OHNS- residents cited an adequate exposure to airway emergencies, underscoring the paucity of such events during residency training. The advent of complex, computerized mannequin simulators deployed in realistic clinical settings and scenarios provides one possible mechanism to provide trainees with lifelike experiences [32]. The use of these simulators in both ANES and OHNS residency programs may improve proficiency in real-life high-stress environments [33-35]. At our institution, we address this training limitation with a simulation center that recreates realistic clinical scenarios and procedures with patient simulators, thereby allowing for the deliberate and repeated practice of critical skills to improve quality and patient safety.
The feedback provided by ANES residents suggests that interdisciplinary training with an OHNS service is highly valuable, both in didactic instruction and in practical experience. By far the most frequently cited benefit of the rotation was the exposure to and participation in surgical airways. They also described an enhanced working relationship with the OHNS service, and an appreciation for the airway management skills and techniques they can learn from otolaryngologists. Understanding what each specialty can offer and awareness of where gaps exist in the training curriculum are important consequences of interdisciplinary training that may result in more comprehensive training and experiences for all specialties.
CONCLUSION
In concordance with our hypothesis, this study demonstrates that completion of an OHNS rotation is associated with increased airway management experience, a markedly increased experience with surgical airways and a trend toward experiencing more airway emergencies. However, despite these differences in experience and exposure, there is no difference in resident self-rated confidence and competence. This high confidence-low experience dichotomy may reflect novice overconfidence and suggests the need for improved training methods in emergency airway management. We feel there are enough documented qualitative benefits to continue the OHNS rotation. To close the gap between overconfidence and limited or no experience, we recommend systematic, objectively-assessed training in emergency airway managment with specific emphasis on surgical airways for both OHNS and ANES residents. This could likely be most effectively accomplished through simulation-based deliberate practice using mannequins, cadavers, or both in settings approximating the challenges of real cases.
ACKNOWLEDGMENT
We thank the University of Chicago Simulation Center for intellectual input and support. We thank Ms. Jamie M. Phillips for logistical assistance.
REFERENCES
- Dunn S, Connelly NR, Robbins L (2004) Resident training in advanced airway management. J Clin Anesth 16: 472-476.
- Gaiser RR (2000) Teaching airway management skills. How and what to learn and teach. Crit Care Clin 16: 515-525.
- Wong E, Ng YY (2008) The difficult airway in the emergency department. Int J Emerg Med 1: 107-111.
- Mort TC (2007) Anesthesia practice in the emergency department: overview, with a focus on airway management. Curr Opin Anaesthesiol 20: 373-378.
- Andrews JD, Nocon CC, Small SM, Pinto JM, Blair EA (2012) Emergency airway management: training and experience of chief residents in otolaryngology and anesthesiology. Head Neck 34: 1720-1726.
- Goldmann K, Ferson DZ (2005) Education and training in airway management. Best Pract Res Clin Anaesthesiol 19: 717-732.
- Greenland KB, Edwards MJ, Beckmann L, Hutton N (2009) Difficult airway management--a glass half empty. Anaesthesia 64: 1024-1025.
- Koppel JN, Reed AP (1995) Formal instruction in difficult airway management. A survey of anesthesiology residency programs. Anesthesiology 83: 1343-1346.
- Ratnayake B, Langford RM (1996) A survey of emergency airway management in the United Kingdom. Anaesthesia 51: 908-911.
- Clarke RC, Gardner AI (2008) Anaesthesia trainees’ exposure to airway management in an Australian tertiary adult teaching hospital. Anaesth Intensive Care 36: 513-515.
- Duwat A, Hubert V, Deransy R, Dupont H (2013) [Difficult airway management: assessment of knowledge and experience in anaesthesiology residents]. Ann Fr Anesth Reanim 32: 231-234.
- Frova G, Sorbello M (2009) Algorithms for difficult airway management: a review. Minerva Anestesiol 75: 201-209.
- Goldhill DR, Cook TM, Waldmann CS (2009) Airway incidents in critical care, the NPSA, medical training and capnography. Anaesthesia 64: 354-357.
- Rose DK, Cohen MM (1996) The incidence of airway problems depends on the definition used. Can J Anaesth 43: 30-34.
- Orebaugh SL (2002) Difficult airway management in the emergency department. J Emerg Med 22: 31-48.
- Sheehan K (2001) E-mail survey response rates: a review. J Computer-Mediated Communication 6.
- Wong DT, Prabhu AJ, Coloma M, Imasogie N, Chung FF (2003) What is the minimum training required for successful cricothyroidotomy?: a study in mannequins. Anesthesiology 98: 349-353.
- Riley RH, Strang T, Rao S (2009) Survey of airway skills of surgeons in Western Australia. Anaesth Intensive Care 37: 630-633.
- Bair AE, Filbin MR, Kulkarni RG, Walls RM (2002) The failed intubation attempt in the emergency department: analysis of prevalence, rescue techniques, and personnel. J Emerg Med 23: 131-140.
- Chang RS, Hamilton RJ, Carter WA (1998) Declining rate of cricothyrotomy in trauma patients with an emergency medicine residency: implications for skills training. Acad Emerg Med 5: 247-251.
- Levitan RM (2001) Myths and realities: the “difficult airway” and alternative airway devices in the emergency setting. Acad Emerg Med 8: 829-832.
- Clyburn PA (2004) Early thoughts on ‘Why Mothers Die 2000-2002’. Anaesthesia 59: 1157-1159.
- Cheney FW (1999) The American Society of Anesthesiologists Closed Claims Project: what have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology 91: 552-556.
- Dunn S, Connelly NR, Robbins L (2004) Resident training in advanced airway management. J Clin Anesth 16: 472-476.
- Hagberg CA, Greger J, Chelly JE, Saad-Eddin HE (2003) Instruction of airway management skills during anesthesiology residency training. J Clin Anesth 15: 149-153.
- Lavery GG, McCloskey BV (2008) The difficult airway in adult critical care. Crit Care Med 36: 2163-2173.
- Davis DA, Mazmanian PE, Fordis M, van Harrison R, Thorpe KE, et al. (2006) Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 296: 1094-1102.
- Mandel LS, Goff BA, Lentz GM (2005) Self-assessment of resident surgical skills: is it feasible? Am J Obstet Gynecol 193: 1817-1822.
- Nadel FM, Lavelle JM, Fein JA, Giardino AP, Decker JM, et al. (2000) Assessing pediatric senior residents’ training in resuscitation: fund of knowledge, technical skills, and perception of confidence. Pediatr Emerg Care 16: 73-76.
- Pothier DD, Bredenkamp C (2006) Hearing aid insertion: correlation between patients’ confidence and ability. J Laryngol Otol 120: 378-380.
- Kruger J, Dunning D (1999) Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol 77: 1121-1134.
- Kory PD, Eisen LA, Adachi M, Ribaudo VA, Rosenthal ME, et al. (2007) Initial airway management skills of senior residents: simulation training compared with traditional training. Chest 132: 1927-1931.
- Abrahamson S, Denson JS, Wolf RM (2004) Effectiveness of a simulator in training anesthesiology residents 1969. Qual Saf Health Care 13: 395-397.
- Amin MR, Friedmann DR (2013) Simulation-based training in advanced airway skills in an otolaryngology residency program. Laryngoscope 123: 629-634.
- Côté V, Kus LH, Zhang X, Richardson K, Nguyen LH (2015) Advanced airway management teaching in otolaryngology residency programs in Canada: A survey of residents. Ear Nose Throat J 94: 187-192.
Citation: Nocon CC, Pinto JM, Blair EA, Small SD (2016) Interdisciplinary Rotations in Residency Training: Impact on Airway Management Experience. J Anesth Clin Care 3: 014
Copyright: © 2016 Cheryl C Nocon, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.