
Is there a systemic analgesic effect of local anesthetics after peripheral ALR? Observation during a comparative study of three analgesic techniques for the treatment of rupture of the anterior cruciate ligament of the knee
*Corresponding Author(s):
Okba LaouamriAssociate Professor In Anesthesia And Intensive Care, Ferhat ABBAS University Of Sétif, CHU Sétif, Algeria
Tel:00213661760895,
Email:laokbus@gmail.com
Abstract
- Introduction
The aim of this study was to compare the sensory block time of spinal anesthesia and the incidence of headache between two groups each receiving a peripheral locoregional analgesia technique and a group without ALR in anterior cruciate ligament reconstruction surgery of the knee.
- Hypothesis
The systemic analgesic effect of peripheral ALR prolongs the time of sensory-motor block and reduces pain intensity, including post-spinal headache.
- Material
We included 165 patients undergoing primary reconstruction of the anterior cruciate ligament of the knee. All patients underwent spinal anesthesia. The first group, systemic analgesia (SA), received balanced systemic analgesia postoperatively for a minimum of five days, based on Paracetamol, Diclofenac and a morphine PCA. In addition to the systemic analgesia already described, the second group, femoral analgesia (FA), will benefit from a femoral peri-nervous catheter in the crural position. 20 ml of bupivacaine at 0.125% concentration is injected; maintenance is set up immediately with a continuous flow of 8 ml/h for 36 h. The third intra-articular analgesia (IAA) group received, in addition to the same systemic analgesia, an infusion through an epidural catheter of 20 ml of 0.125% bupivacaine, followed by maintenance with 8 ml /h of the same local anesthetic via an electric syringe pump for 36 hours. Cumulative morphine consumption, pain assessment using a numerical scale (EN) from 1 to 10, time to lift the spinal motor-sensory block and frequency of post-spinal headaches were evaluated.
- Results
The mean age of our patients was 30.00 ± 7.30 years, with extremes ranging from 17 to 52 years. There was a clear male predominance, with 97.6% men (n= 161) and 2.4% women. Analgesia was better in the AF group than in the AIA group, as evidenced by pain scores. Morphine consumption was lower in the AF group (femoral peri-nerve) and the difference was statistically significant with an F = 3.539(2) and a p = 0.031. Mean sensory block release was estimated at 4.78 ± 1.013 hours. Mean block release was 4.60 ± 0.913 hours for the AS group, 5.16 ± 0.903 hours for the AF group and 4.78 ± 1.013 hours for the AIA group. Comparison of these means found a statistically significant difference with an F= 4.623(2) and p=0.011. Post-spinal anesthesia headache was reported, from d 2 postoperatively, in 08 patients, i.e. 4.8%, while 06 out of 55 cases occurred in the AS group, i.e. 10.9%. Analysis of variances found a significant difference with a Chi-2 = 7.357 (2), p = 0.025.
- Discussion
This study raises the suspicion that local anesthetics given as part of peripheral locoregional analgesia have a systemic analgesic effect.
Keywords
Anesthesia ; Analgesia ; Morphine
Introduction
Cure of the anterior cruciate ligament of the knee is a common and reputedly painful surgical procedure, requiring well-conducted analgesia in advance. The most widely used technique is the Kenneth Jones (K J) open technique, which involves the use of a free bone-tendon-bone transplant using the middle third of the patellar tendon [1]. Several classic and conventional analgesic techniques were discussed and compared, taking into account the evolution of technical and pharmacological means in anesthesia and analgesia.
The aim of analgesia is twofold: on the one hand, to improve patient comfort, and on the other, to accelerate postoperative functional recovery [2]. Peripheral regional anesthesia and analgesia of the lower limb is currently the gold standard in knee surgery [3]. Several analgesic techniques and procedures have been compared, including femoral nerve blocks and intra-articular analgesia. These blocks offer considerable perioperative morphine savings and reduced pain scores.
Initial induction, with or without maintenance, with a quantity of a local anesthetic to anesthetize or analgesize the surgical site is automatically followed by resorption, redistribution and metabolism of this molecule before its elimination.
This resorption and redistribution are not without systemic effects, including an analgesic effect.
The aim of this work is to give two arguments in favor of this hypothesis.
Materials And Methods
Population
A comparative study including 165 patients undergoing anterior cruciate ligamentoplasty was divided into 03 study groups.
Inclusion criteria
- Consenting patients.
Exclusion criteria
- Patient refusal
- Surgical revision
- Alternative indications for ALR
- Contraindications to non-steroidal anti-inflammatory drugs
Population size
During the study period, 173 patients were admitted for knee ligamentoplasty, of whom eight were excluded: five refusals of spinal anesthesia, two repeat surgeries and one contraindication to diclofenac.
Methods
A total of 165 cases were included, divided into three study groups by random selection.
Study protocols
Intra-anesthetic stage
All patients underwent spinal anesthesia with 12.5 mg bupivacaine 0.5% + 25 δ clonidine, using a 27G Quincke-type needle.
Procedures
After surgery, patients were clearly informed of the three analgesic procedures and informed consent was obtained:
- The first group (AS) will receive systemically balanced analgesia postoperatively for a minimum of five days, based on:
- Paracetamol at a dose of 1g every 6h per os.
- Diclofenac 50 mg every 12 hours per os.
- And a morphine PCA with a concentration of 1mg /ml and a refractory period of 7 min.
- In addition to the systemic analgesia already described, the second group (AF) will benefit from a femoral peri-nervous catheter in the crural position for a minimum of five days, with the same dosage:
After locating the femoral nerve by ultrasound, and dilating the space with a few milliliters of saline, a 5-8 cm catheter is inserted.
20 ml of bupivacaine at a concentration of 0.125% is injected fractionally through the anti-bacterial filter. Maintenance is started immediately with a continuous flow of 8 ml/h of the same anesthetic via an electric thumb syringe, for 36 h.
- The third group (AIA) will receive, again in addition to the same systemic analgesia already described, through an epidural-type catheter placed intra-articularly by the surgeon at the end of the procedure after closure of the joint capsule and mounted 5 to 8 cm and securely fastened.
20 ml bupivacaine 0.125% is injected through the antibacterial filter 10 to 15 min before deflating the pneumatic tourniquet, with the Redon drain still clamped. Maintenance is also started immediately with 8 ml/h of the same local anesthetic via an electric syringe pump for 36 hours.
Data from
The following criteria were collected prospectively during hospitalization and after discharge home:
- Immediately postoperative and until catheter removal:
- Quantitative:
- Cumulative consumption of morphine
- Estimation of sensory-motor block release time in spinal anesthesia,
- Qualitative:
- Pain assessment using a numerical scale (EN) from 1 to 10
- The frequency of headaches after spinal anesthesia
Statistical analysis
Results are analyzed using SPSS statistics 26 software. We use both descriptive and analytical statistical techniques.
Results
Population
The demographic parameters of the cohort are reported in (Table 1).
The average age of our patients was 30.00 ± 7.30 years, with extremes ranging from 17 to 52 years. There was a clear male predominance, with 97.6% men (n= 161) and 2.4% women. there was no significant difference between the three groups for the initial criteria.
|
Groups |
Total (N = 165) |
Systemic balanced analgesia(n=55) |
Femoral peri-nerve (n=55) |
Continuous intra-articular (n=55) |
P |
|
Age |
30,00 ± 7,30 |
29.36 ± 6.745 |
30.16 ± 7.932 |
30.47 ± 7.280 |
0.716 |
|
Gender : Male : |
(161) |
33,5% (54) |
32,9% |
33,5% (54) |
0,774 |
|
Female : |
97,6% (04) 2,4% |
25% (01) |
(53) 50% (02) |
25% (01) |
|
|
ASA : |
|
|
|
|
0,551 |
|
ASA 1 : |
(158) |
(54) |
(52) |
(52) |
|
|
ASA 2 : |
95,8% (07) 4,2% |
(01) |
(03) |
(03) |
|
Table 1 : Demographic data by study group
Pain assessment
Postoperative pain assessment using a numerical scale from 0 to 10 was collected repeatedly from the second hour to the fifth day. From H2 to D5 post-op, the means with standard deviations of the EN are summarized in (Table 2) with comparisons by study group and statistical significance.
Analgesia was better in the AF then AIA group compared to AS as evidenced by pain scores:
|
|
Total |
AS Group |
AF Group |
AIA Group |
p |
|
H2 |
0,72(1,66) |
0,67(1,41) |
1,08(2,31) |
0,44(0,99) |
NS |
|
H4 |
2,19(2,10) |
2,45(2,21) |
1,65(1,89) |
2,42(2,12) |
NS 0.084 |
|
H6 |
3,52(2,32) |
3,50(2,39) |
3,12(2,38) |
3,91(2,16) |
NS |
|
H8 |
3,54(2,49) |
3,52(2,47) |
3,16(2,39) |
3,91(2,59) |
NS |
|
H12 |
2,29(2,26) |
2,58(2,36) |
2,27(2,35) |
2,04(2,26) |
NS |
|
H16 |
1,63(1,92) |
1,98(2,11) |
1,49(1,95) |
1,42(1,68) |
NS |
|
H20 |
1,38(1,79) |
1,60(1,79) |
1,18(1,64) |
1,35(1,93) |
NS |
|
H24 |
1,11(1,55) |
1,49(1,64) |
0,69(1,30) |
1,11(1,59) |
0,034 |
|
H28 |
0,90(1,36) |
1,24(1,52) |
0,59(1,08) |
0,85(1,36) |
NS 0.063 |
|
H36 |
0,80(1,56) |
1,26(2,04) |
0,46(1,22) |
0,61(1,13) |
0,03 |
|
J2 |
0,87(1,43) |
1,06(1,53) |
0,75(1,41) |
0,78(1,36) |
NS |
|
J3 |
0,61(1,29) |
0,62(0,86) |
0,45(1,13) |
0,72(1,72) |
NS |
|
J4 |
0,57(1,38) |
0,60(1,25) |
0,20(0,56) |
0,84(1,85) |
NS |
|
J5 |
0,57(1,48) |
0,69(1,36) |
0,41(1,33) |
0,58(1,72) |
NS |
Table 2: Means with standard deviations of EN at rest by group
Morphine consumption
Consumption was lower in the AF (femoral peri-nerve) group and the difference was statistically significant with an F = 3.539(2) and a p = 0.031.
The post-hoc test shows a difference in mean of 6.12 ± 2.41 between the AS and AF groups with a significant p = 0.012, a difference in mean of 1.67 ± 2.41 with a non-significant p = 0.49 between the AF and AIA groups and a difference in mean of 4.45 ± 2.31 with a p = 0.056 at the limit of significance between the AS and AIA groups (Figure 1).
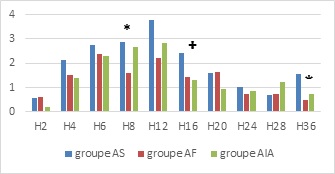 Figure 1: Average morphine consumption by group.
Figure 1: Average morphine consumption by group.
(*): p < 0.05 between AS and AF groups
(†): p < 0.05 between AF and AIA groups
(‡): p < 0.05 between AS and AIA groups
Removal of sensory-motor block:
Removal of sensory block was estimated on average at 4.78 ± 1.013 hours; it was 4 hours in 33% and 5 hours in 34% of patients.There was no statistically significant difference between the different age groups, with an F = 0.421(6), and a p = 0.864.
Block release occurred after 4.78 ± 1.002 in men versus 5.00 ± 1.732 in women. The difference was statistically insignificant with Student's t-test = -0.377(149), and p = 0.707.
Block lift was 4.81 ± 1.016 for ASA 1 versus 4.17 ± 0.753 for ASA 2 and the difference was not significant with a t = 1.524 (149), and p = 0.130.
For the different study groups, the mean of block removal was 4.60±0.913 hours for the AS group, 5.16 ± 0.903 hours for the AF group and 4.78±1.013 hours for the AIA group.
Comparison of these averages found a statistically significant difference with an F= 4.623(2) and a p=0.011 (Table 3).
The post hoc test indicates a mean difference of 0.559 [0.16-0.96] and a p=0.006 between the AF group and the AS group, and a mean difference of 0.507 [0.11-0.90] and a p=0.012 between the AF group and the AIA group. The difference between the AS and AIA groups was not significant.
|
Groups |
Average |
N |
Standard deviation |
|
Systemic balanced analgesia group |
4,60 * |
52 |
,913 |
|
Femoral peri-nerve |
5,16 |
45 |
,903 |
|
Continuous intra-articular |
4,65 † |
54 |
1,119 |
|
Total |
4,78 |
151 |
1,013 |
|
P |
0,011 |
|
|
Table 3: Mean time to block removal by study group.
(*) p = 0.006 between AS and AF groups;
(†) p = 0.012 between AF and AIA groups
Headache post-spinal anesthesia
Post-spinal anesthesia headache was reported, from d 2 postoperatively, in 08 patients, i.e. 4.8% of our sample. One case required a Blood Patch on postoperative day 15, while the rest gradually subsided with the same analgesic treatment and postural measures (lying down in a calm environment). All 08 patients were male and classified as ASA 1 (Table 4).
The age group most concerned was 20 to 24, but the difference was not statistically significant with an F = 0.325 and a p = 0.569;
|
Headache |
AS Group |
AF Group |
AIA Group |
Total |
P |
|
|
Workforce |
6 |
2 |
0 |
8 |
|
|
|
% in groups |
10,9% |
3,6% |
0,0% |
4,8% |
0,025 |
|
Table 4: Headache incidence by study group
06 out of 55 cases occurred in the AS group, i.e. 10.9%, and 02 out of 55 in the AF group, i.e. 3.6%. No cases were reported in the AIA group.
The analysis of variances found a significant difference with a Chi-square = 7.357 (2), p = 0.025
Discussion
Pain kinetics
From H0 to H36, pain kinetics in our series followed a similar pattern in both study groups compared to the AS group considered as control; with a higher fraction of mild pain in these groups but without statistical significance;
From H0 to H8, the percentage of mild pain decreased and the mean EN increased. This is explained by the gradual lifting of the sensory block and the gradual reduction in the number of patients still blocked under spinal anesthesia.Maximum pain was observed at H6 and H8, which may be explained by pain rebound after locoregional anesthesia. In our series, this was probably due to pain rebound after lifting of the spinal anesthesia sensory block. Similarly, the rebound observed at D2 in the AF and AIA groups after the scheduled cessation of continuous LA infusion.
In the literature, this rebound can increase EN by 2[1.6-2.4] [4].
From H8 to D5, pain decreased progressively, reaching a minimal average at D4 and D5 postoperatively. This decrease was probably due to the impregnation of pain receptors by analgesics and local anesthetics, but also to a natural reduction in pain intensity.
Morphine consumption
The morphine consumption curve faithfully follows the pain kinetics curve, i.e. the direct relationship between pain intensity and morphine consumption.
Femoral peri analgesia provided considerable morphine savings compared with systemic analgesia (6.12 ± 2.41; p = 0.012). An expected result that parallels the reduction in pain scores in this group.
Intra-articular analgesia resulted in morphine savings of 4.45 ± 2.31 mg with a p = 0.056.
Consumption was lower, especially in the first 06 hours, and from H12 to H24 (especially H16).
Increasing the concentration of LA and/or adding morphine could reinforce this sparing.
Lifting the block
Sensory block release was estimated to average 4.78 ± 1.013 hours in our series.
In a study comparing the lifting of sensory-motor block after spinal anesthesia with mepivacaine and bupivacaine without adjuvants, including 32 patients, the mean time of sensory block with bupivacaine was 212 ± 54.2 min or 3.53 ± 0.90 hour [5]. The difference with our series could be secondary to the addition of clonidine, known to increase spinal anesthesia time.In another study involving 106 patients divided into two groups: spinal anesthesia with bupivacaine (hyperbaric) and spinal anesthesia with 2-chloroprocaine, the time to release of sensory block in the bupivacaine group was estimated at 329 minutes or 5.48 hours [6]. In this case, hyperbaric prolongs the duration of anesthesia.Femoral nerve block appears to prolong the sensory block of spinal anesthesia by more than 30 minutes with a p = 0.011.There seems to be very little literature on the subject It is possible that the systemic resorption of local anesthetic after a peripheral block, while increasing, slows the de-fixation of local anesthetic from its site of action, thus increasing contact time and thus sensory block. In a study analyzing the pharmacokinetics of 20 ml ropivacaine after femoral block, the author reported biphasic kinetics, with a rapid resorption phase of 25 ± 4.8 min, followed by a slow phase of 3.9 ± 0.65 h, with peak plasma concentration at 10 min and then 60 min [7,8] Inspired by the analgesic model of intravascular lidocaine [9], This redistribution could have analgesic effects at a distance, including at spinal level, reinforcing the effect of spinal anesthesia.
Post-spinal anesthesia headache
The incidence of post-spinal anesthesia headache in our series was 4.8% (08 cases), all occurring in males. Relatively high incidence despite preventive precautions such as the use of a fine needle [10, 11] 06 cases occurred in the AS group, 02 in the AF group and 0 in the AIA group. The difference was significant (p = 0.025).The significant difference in incidences according to study group is purely coincidental, given that analgesic procedures are independent of spinal anesthesia.
These headaches remain a major source of patient dissatisfaction.
Conclusion
Peripheral ALR provides better analgesic quality and a considerable reduction in morphine consumption. The prolonged sensory-motor block time of spinal anesthesia and reduced incidence of post-spinal headache in patients undergoing peripheral ALR procedures could be a systemic analgesic effect of local anesthetics.
References
- Jones KG (1970) Reconstruction of the Anterior Cruciate Ligament Using the Central One-Third of the Patellar Ligament: A follow-up report. J Bone Joint Surg Am 52:1302-1308.
- Capdevila X, Morau BD (2000) Analgésie pour chirurgie du genou: conférences d'actualisation. SFAR 21- 41
- Choquet O, Zetlaoui PJ (2014) Techniques d'anesthesie regionale peripherique du membre inferieur. EMC- Anésthesie Réanimation 11: 294-322.
- Williams BA, Bottegal MT, Kentor ML, Irrgang JJ, Williams JP (2007) Rebound pain scores as a function of femoral nerve block duration after anterior cruciate ligament reconstruction: retrospective analysis of a prospective, randomized clinical trial. Reg Anesth Pain Med 32:186-192.
- Mahan CM, Jildeh TR, Tenbrunsel T (2000) Time of return of neurologic function after spinal anesthesia for total knee arthroplasty: mepivacaine vs bupivacaine in a randomized controlled trial. Arthroplasty Today 5: 226-233.
- Lacasse MA, Roy JD, Forget J, Vandenbroucke F, Seal RF, et al. (2000) Comparison of bupivacaine and 2-chloroprocaine for spinal anesthesia for outpatient surgery: a double-blind randomized trial. Can J Anesth 58: 384-391.
- Gaudreault F, Drolet P, Fallaha M, Varin F (2012) A population pharmacokinetic model for the complex systemic absorption of ropivacaine after femoral nerve block in patients undergoing knee surgery. J Pharmacokinec Pharmacodyn 39: 635-642.
- Gaudreault F, Drolet P, Fallaha M, Varin F (2015) Modeling the Anesthetic Effect of Ropivacaine after a Femoral Nerve Block in Orthopedic Patients. A Population Pharmacokinetic-Pharmacodynamic Analysis. Anesthesiology 122: 1010-1020.
- Kranke P, Jokinen J, Pace NL, Helf A, Eberhart LH, et al. (2015) Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery (Review). Cochrane Database of Systematic Reviews 6: CD009642.
- Eledjam JJ, Viel E, Aya G, Manqin R (1993) Postdural puncture headache. Cah Anestesiol 41: 579-588.
- Lambert DH, Hurley RJ, Hertwiq L, Datta S (1997) Role of needle gauge and tip configuration in the production of lumbar puncture headache. Reg Anesth 22: 66-72.
Citation: Laouamri O (2023) Is there a systemic analgesic effect of local anesthetics after peripheral ALR? Observation during a comparative study of three analgesic techniques for the treatment of rupture of the anterior cruciate ligament of the knee.J Anesth Clin Care 10: 083.
Copyright: © 2023 Okba Laouamri, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

