Management and outcome of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations: How to Determine and What is Recommended for Surgical Treatment?
*Corresponding Author(s):
Masahide HiyoshiDepartment Of Surgery, Faculty Of Medicine, University Of Miyazaki, Miyazaki, Japan
Tel:+81-985-85-2905,
Fax:+81-985-85-5814
Email:mhiyoshi@med.miyazaki-u.ac.jp
Abstract
- Objective
Endoscopic retrograde cholangiopancreatography (ERCP)-related duodenal perforations are a worrisome and life-threatening complication. The aims of this study were to confirm the results of ERCP-related duodenal perforations and to aid in determining indications and appropriate surgical treatment.
- Methods
From January 2002 through December 2015, 4953 patients who received ERCP were investigated. We investigated the ERCP procedures, time required from ERCP to computed tomography (CT) scan, CT findings, and treatment that were performed on the patients who had ERCP-related duodenal perforations, which were classified according to Stapfer’s classification.
- Results
ERCP-related duodenal perforations occurred in 3 (0.06%) patients, and all were classified as type II. Two patients were treated conservatively and recovered. The third patient received surgical treatment 45 hours after injury. The perforated site was trimmed and primary closure was performed, drainage tube were inserted to the abdominal cavity, biliary tract, and intestine, and tube jejunostomy (triple tube ostomy) was performed. After the emergency operation, although the perforation was closed, the patient died of multiple organ failure 42 days after surgery.
- Conclusion
ERCP-related duodenal perforations are rare but require appropriate diagnosis and treatment as quickly as possible. As surgical treatments, primary simple closure, abdominal drainage, and triple tube ostomy are recommended.
Keywords
Duodenal perforation; ERCP; Stapfer’s classification; Triple tube ostomy
Introduction
Endoscopic Retrograde Cholangio Pancreatography (ERCP) is a useful and necessary procedure for pancreato-biliary disorders. Recently, many procedures, including not only classical procedures such as cytology for the diagnosis of malignancy [1,2] biliary drainage for obstructive jaundice or cholangitis [3,4] and lithotripsy for biliary stones [5,6] but also the most recent procedures such as endoscopic papillectomy for papillary tumor [7,8] have been improved and performed safely. However, the rate of ERCP-related duodenal perforations remains high (0.2-1.5%) [9-13] and delayed diagnosis or its misdiagnosis can be fatal. The aims of this study were to confirm the results of ERCP-related duodenal perforations in our institution and to aid in determining indications and appropriate surgical treatment.
Methods
- Patients
From January 2002 through December 2015, the patients who received ERCP at our Hospital were enrolled in this study. Using their medical records, we investigate the ERCP procedures, time required from ERCP to Computed Tomography (CT) scan, CT findings, and endoscopic treatment and surgical treatment for the patients who had ERCP-related duodenal perforations. The study protocols were approved by the Human Ethics Review Board of our institution (approval no. and date: #O-0489, November 30, 2020). Agreement by the patients to enter the study was obtained by an opt-out procedure for one month at the website and outpatient clinic of our hospital.
- Classification of ERCP-related duodenal perforations
ERCP-related duodenal perforations were classified using the classification system proposed by Stapfer et al. [13] as follows. Type I: Lateral or medial wall perforation caused by the endoscope that tends to be large and remote from the ampulla. Type II: Perivaterian injuries. Type III: Distal bile duct injuries related to wire or basket instrumentation near an obstructing entity and that are often small. Type IV: Retroperitoneal air alone that is probably related to the use of compressed air to maintain patency of a lumen.
- Results
ERCP was performed on 4953 patients, and 3 patients had ERCP-related duodenal perforations (0.06%) (Table 1). All 3 were men with an average age of 74.3 ± 9.6 years. They received ERCP for choledocholithiasis, and 1 patient received ERCP with forward-viewing endoscope because of Billroth II reconstruction after gastrectomy for duodenal ulcer. Endoscopic Sphincterotomy (EST) was performed on 372 patients, and all 3 of the perforated patients had received EST (0.81%) and extraction of gallstones. The duodenal perforations in these 3 patients were all classified as type II injury and were suspected based on the endoscopic findings during the procedure. Contrast medium leakage was recognized in 2 patients (cases 1, 2). An endoscopic nasobiliary drainage (ENBD) tube was placed for biliary drainage in all of them. A CT scan was performed within about 1 hour after injury (54, 57, 63 min, respectively), and it revealed the presence of retroperitoneal air. One patient (case 2) had CT findings of fluid collection in the retroperitoneal space and received surgical treatment whereas the other two patients were treated conservatively. These two patients were discharged 29 and 19 days after injury, respectively. Unfortunately, the patient who underwent surgery died 42 days after injury from multiple organ failure.
|
Sex |
Disease |
Past History |
ERCP Procedure |
Biliary Drainage |
Stapfer Classification |
Time From ERCP to CT (Min) |
Fluid Collection |
Symptoms |
Treatment |
Prognosis |
|
Male |
CBD Stone |
Gastrectomy (B- II) Parivaterian diverticulum |
EST, Ext |
ENBD |
II |
63 |
No |
Free |
NOM |
Discharge (29 days) |
|
Male |
CBD Stone |
Cerebral Infraction Chronic hepatis |
EST, Ext |
ENBD |
II |
57 |
Yes |
Abdominal Pain Defence (+) |
Surgery |
Death (42 days) |
|
Male |
CBD Stone |
Parivaterian diverticulum Hypertension |
EST, Ext |
ENBD |
II |
54 |
No |
Abdominal Pain Defence (-) |
NOM |
Discharge (19 days) |
Table 1: ERCP-Related duodenal perforations in our institution. CBD Common Bile Duct, CT Computed Tomography; ENBD Endoscopic retrograde Cholangiopancreatography; EST Endoscopic Spincteroctomy; EXt Extraction, NOM Non Operative Management.
Case Presentation
- Case 2
An 83-year-old-man received ERCP to treat his choledocholithiasis. A filling defect of about 10 mm in diameter that indicated the presence of gallstones was recognized in the common bile duct by cholangiography using contrast medium (Figure 1a & 1b ). EST was performed and the stone was removed. During the extraction using a balloon catheter, contrast medium leakage was confirmed by cholangiography and duodenal injury was suspected. A CT scan revealed retroperitoneal air that indicated duodenal penetration and the collection of contrast medium in that space (Figure 2). Slight abdominal pain was observed but no peritoneal irritation sign, so conservative therapy with non per oral administration of antibiotics and a proton pump inhibitor was selected. However, the patient’s abdominal pain increased, his body temperature rose to 39.7°C and tachycardia and hypotension indicative of septic shock appeared. Blood examination revealed that his white blood cell count and C-reactive protein level were increased and his platelet count was decreased. Therefore, we abandoned conservative treatment and performed surgical treatment 45 hours after ERCP. Intraoperative findings revealed that the retroperitoneum was contaminated with bile and intestinal juice. As the surgical treatments, primary closure at the site of perforation, omental coverage, abdominal lavage, abdominal drainage, and catheter jejunostomy were performed. Although the site of perforation was closed, the patient’s general condition worsened over the postoperative course, and he subsequently died of multiple organ failure at 42 days after ERCP.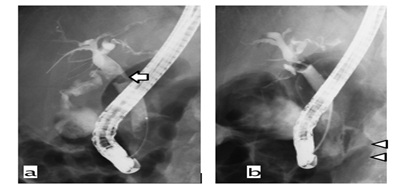 Figure 1: X-ray images from Case 2. a) Cholangiography revealed a filling defect 10 mm in diameter (white arrow) that indicated stones in the common bile duct. b) Contrast medium leakage to the retroperitoneal space was confirmed (white arrowhead).
Figure 1: X-ray images from Case 2. a) Cholangiography revealed a filling defect 10 mm in diameter (white arrow) that indicated stones in the common bile duct. b) Contrast medium leakage to the retroperitoneal space was confirmed (white arrowhead).
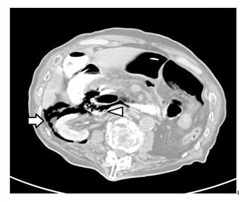 Figure 2: CT scan revealed retroperitoneal air that indicated duodenal penetration (white arrow) and with contrast medium collection in that space (white arrowhead).
Figure 2: CT scan revealed retroperitoneal air that indicated duodenal penetration (white arrow) and with contrast medium collection in that space (white arrowhead).
- Case 3
A 79-year-old man also underwent ERCP for treatment of his choledocholithiasis. After EST and extraction of a common bile duct stone, 2 holes were recognized on the endoscopic view (Figure 3). We thought that one was anterior to the bile duct and that the other led to penetration of the retroperitoneal space. An ENBD tube was immediately inserted into the bile duct. A CT scan revealed retroperitoneal air but no fluid collection. He complained of slight abdominal pain but had no peritoneal irritation sign.
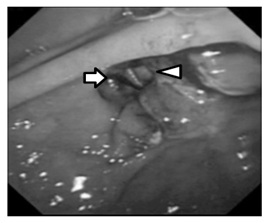 Figure 3: Endoscopic view revealed 2 holes. One was anterior to the bile duct (white arrowhead) and the other led to penetration of the retroperitoneal space (white arrow).
Figure 3: Endoscopic view revealed 2 holes. One was anterior to the bile duct (white arrowhead) and the other led to penetration of the retroperitoneal space (white arrow).
Conservative therapy was selected, and his symptoms decreased. He accidentally removed the ENBD tube by himself 2 days after ERCP, but the tube was not replaced. Follow-up CT performed 6 days after ERCP revealed that the retroperitoneal air had disappeared (Figures 4a & 4b). He was discharged uneventfully 19 days after the injury.
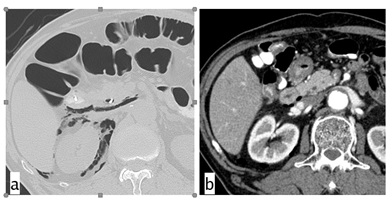 Figure 4: CT scans from Case 3. a) CT scan revealed retroperitoneal air but not fluid collection. b) Follow-up CT performed 6 days after ERCP showed disappearance of the retroperitoneal air.
Figure 4: CT scans from Case 3. a) CT scan revealed retroperitoneal air but not fluid collection. b) Follow-up CT performed 6 days after ERCP showed disappearance of the retroperitoneal air.
Discussion
ERCP-related duodenal perforations are worrisome and occasionally life-threatening complications that occur at a rate of 0.2-1.5% [9-13]. The mortality rate of patients with perforation increases to 5.9–33.3%, even if they receive surgical treatment [9-11,14,15]. Recently the rate of ERCP-related complications has increased as the opportunity for endoscopic treatment has increased. Stapfer et al. reported the classification and management of ERCP-related duodenal perforations [13]. The rates of type I, II, III, and IV perforations were 13.8–25.4%, 58.0–75.9%, 6.9–22.1%, and 2.5–10.5%, respectively [11,15,16]. Because type I injury is mainly caused by the endoscope itself and tends to be a large injury such as a laceration, it commonly requires surgical repair. Recently, according to improvements in endoscopic skill and treatments such as over-the-scope clipping [17,18] and purse-string suture [19], endoscopic repair has been attempted for duodenal perforation repair after endoscopic mucosal resection. We assume that endoscopic repair was attempted initially even in type I injury, but it was allowable in patients whose general condition was stable and the injury site was small. However, it is important not to overdo endoscopic treatment. During endoscopic repair, use of CO2 is safe, and it can help to reduce the pain [20,21].
Type II injury is caused mainly by EST or another treatment such as extraction of a stone near the papilla. This injury is mostly treated by conservative, non-operative management (NOM), and its success rate was reported to be 60-70% [13,15]. Type III injury is caused when using a treatment device inserted to the biliary tract such as a guidewire or lithotripsy basket catheter, and it is commonly treated by NOM as with type II. For treatment of type II and III injuries, biliary drainage is important to prevent the spread of bile to the retroperitoneum, hepatoduodenal ligament, and intraabdominal space. Recently, fully covered self-expandable metallic stents were used as conservative therapy for type II injury, and the results were good [22,23]. Type IV perforations are revealed only by the presence of retroperitoneal air with no physical symptoms. The cause is unknown, and this perforation is also treated conservatively or by observation of the patient’s course.
In this study, all 3 patients with perforation were classified as having a type II injury and received conservative treatment initially. Even if conservative treatment is chosen, surgeons should take care to determine whether surgical treatment is necessary as the decision is very important but very difficult. Stapfer et al. reported the surgical indications for treatment of perforation to be large extravasation of contrast at the time of ERCP, fluid collection observed on the follow-up CT, ERCP for choledocholithiasis, massive subcutaneous emphysema after ERCP, and failure of NOM [13]. Wu et al. reported that a CT findings of retroperitoneal fluid collection had a poor prognosis [24]. Park et al. reported that surgery should be considered in conditions of failed endoscopic closure, serious leakage of contrast material, development of sepsis during conservative management, peritonitis, undrained fluid retention in the peritoneum, worsening patient condition [25]. One of our patients unfortunately died after surgical treatment. He had retroperitoneal fluid collection by CT just after the ERCP scan, which indicated that careful, close follow-up was needed. Ultimately, he died of multiple organ failure and we assumed that the main cause of failure was the long time until surgical treatment was performed. Delay of surgery by more than 24 hours after ERCP results in high mortality [9,11], so the decision to perform surgery should be made within 24 hours after ERCP.
Commonly, because the periampullary site is complicated anatomically, it is hard to diagnosis and repair the perforated site correctly, but it is necessary. There are many procedures surgeons can perform to treat duodenal perforations such as primary simple closure, serosal patch closure, pyloric exclusion and pancreaticoduodenectomy. However, emergency pancreaticoduodenectomy is too invasive and has high mortality rates of up to 30-40%, so it is not recommended except when the patient truly requires it and it should be performed by expert hepato-biliary-pancreatic surgeons [26,27]. Pyloric exclusion would appear to be useful for repair of duodenal trauma, although no difference was reported in surgical outcomes of morbidity and mortality between primary closure and pyloric exclusion [28,29]. Ivantury et al. reported that serosal patch repair had a high morbidity rate compared with primary repair and an additional serosal patch did not improve the results [30]. So, primary simple closure would appear to be the best basic surgical procedure for ERCP-related duodenal perforations. When the sites of perforation can be recognized, debridement and primary closure should be attempted.
There are some important technical points to consider in the surgical treatment of perforation. First, at a minimum, appropriate abdominal drainage is necessary [31,32]. In type II injury, the perforated site can spread between the duodenum and pancreas, so debridement and primary simple closure can be difficult in some cases. Even in such cases when the site of perforation cannot be identified or cannot be closed, a drainage tube must be inserted to the retroperitoneal and peritoneal spaces that are close to the duodenum. Second, intestinal decompression via the stomach or duodenum is useful and less invasive. Third, we assume that biliary drainage is useful to prevent the condition from worsening [12,33]. For biliary drainage, a C-tube or T-tube can be inserted via a cystic duct or common bile duct. If possible, catheter jejunostomy is recommended to maintain enteral nutrition and it can accelerate the repair of duodenal perforations (triple tube ostomy) [33,34]. Of course, blood loss and surgical time should be kept to a minimum to reduce surgical stress on the patients.
We present a management strategy for ERCP-related duodenal perforations based on our opinion (Figure 5). As the first step, a CT scan is necessary for diagnosis and classification. Type I injury requires surgical treatment, whereas Type III and IV injuries may be treated conservatively. For Type II injury, the surgeon needs to identify whether conservative or surgical treatment is best. As mentioned earlier, the presence of the retroperitoneal fluid collection should be assessed as its presence indicates the need for surgical treatment. In the second step, endoscopic treatments such as closure of the perforation or biliary drainage are attempted by an expert endoscopist. For Non-Operative Management (NPO) decompression by nasogastric tube, administration of a proton pump inhibitor, broad-spectrum antibiotics, octreotide can be selected. Surgeons should also pay attention to the appearance or exacerbation of abdominal symptoms. In addition, imaging evaluations are needed 6-12, 24, 48-72 hours after injury. If possible, the decision to perform surgical treatment should be made within 12 hours. As surgical treatments, abdominal drainage, primary closure, biliary drainage with C- or T-tube, catheter decompression and catheter jejunostomy (triple tube ostomy) are recommended.
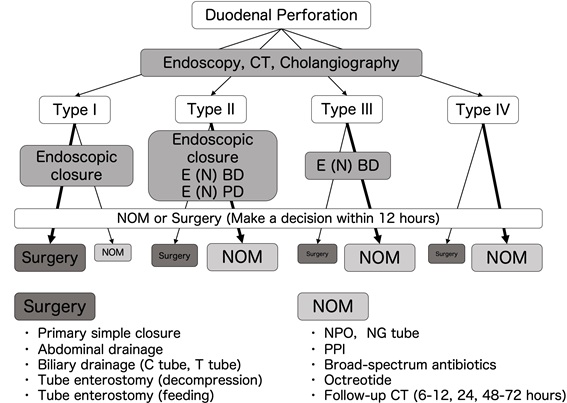 Figure 5: Our management strategy for ERCP-related duodenal perforation. E (N) BD endoscopic (naso) biliary drainage, E (N) PD endoscopic (naso) pancreatic drainage, NOM non-operative management, NPO no peroral, NG tube nasogastric tube, PPI.
Figure 5: Our management strategy for ERCP-related duodenal perforation. E (N) BD endoscopic (naso) biliary drainage, E (N) PD endoscopic (naso) pancreatic drainage, NOM non-operative management, NPO no peroral, NG tube nasogastric tube, PPI.
Conclusion
ERCP-related duodenal perforations are rare but require appropriate diagnosis and treatment. As surgical treatments, primary simple closure, abdominal drainage, triple tube ostomy are recommended.
Funding
The authors received no financial support for the research, authorship and publication of this article.
Declaration of interest
The authors declare that there is no conflict of interest.
References
- Chang HY, Liu B, Wang YZ, Liu B, Wang WJ, et al. (2020) Percutaneous transhepatic cholangiography versus endoscopic retrograde cholangiography for the pathological diagnosis of suspected malignant bile duct strictures. Medicine 99: e19545.
- Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, et al. (2015) Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc 81: 168-176.
- Wang AY, Yachimski PS (2018) Endoscopic management of pancreatobiliary neoplasms. Gastroenterology 154: 1947-1963.
- Mukai S, Itoi T, Baron TH, Takada T, Strasberg SM, et al. (2017) Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guidelines 2018. J Hepatobiliary Pancreat Sci 24: 537-549.
- Lyu Y, Cheng Y, Li T, Cheng B, Jin X (2019) Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc 33: 3275-3286.
- Park CH, Jung JH, Nam E, Kim EH, Kim MG, et al. (2018) Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc 87: 43-57.
- Li S, Wang Z, Cai F, Linghu E, Sun G, et al. (2019) New experience of endoscopic papillectomy for ampullary neoplasms. Surg Endosc 33: 612-619.
- Van der Wiel SE, Poley JW, Koch AD (2019) Endoscopic resection of advanced ampullary adenomas: a single-center 14-year retrospective cohort study. Surg Endosc 33: 1180-188.
- Patil NS, Solanki N, Mishra PK, Sharma BC, Saluja SS, et al. (2020) ERCP-related perforation: an analysis of operative outcomes in a large series over 12 years. Surg Endosc 34: 77-87.
- Mousa HM, Hefny AF, Abu-Zidan FM (2020) Life-threatening duodenal perforation complicating endoscopic retrograde cholangiopancreatography: a case series. Int J Surg Case Rep 66: 404-407.
- Cirocchi R, Kelly MD, Griffiths EA, Tabola R, Sartelli M, et al. (2017) A systematic review of the management and outcome of ERCP related duodenal perforations using a standardized classification system. Surgeon 15: 379-387.
- Machado NO (2012) Management of duodenal perforation post-endoscopic retrograde cholangiography. When and whom to operate and what factors determine the outcome?. A review article JOP 13: 18-25.
- Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, et al. (2000) Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg 232: 191-198.
- Jin YJ, Jeong S, Kim JH, Hwang JC, Yoo BM, et al. (2013) Clinical course and proposed treatment strategy for ERCP-related duodenal perforation: a multicenter analysis. Endoscopy 45: 806-812.
- Vezakis A, Fragulidis G, Polydorou A (2015) Endoscopic retrograde cholangiopancreatography-related perforations: Diagnosis and management. World J Gastrointest Endosc 7: 1135-1141.
- Shi D, Yang JF, Liu YP (2019) Endoscopic treatment of endoscopic retrograde cholangiopancreatography-related duodenal perforations. J Laparoendosc Adv Surg Tech A 29: 385-391.
- Weiland T, Fehlker M, Gottwald T, Schurr MO (2013) Performance of the OTSC System in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc 27: 2258-2274.
- Tashima T, Nonaka K, Ryozawa R (2018) Endoscopic omental patch using an over-the-scope clip for endoscopic retrograde cholangiopancreatography-related large duodenal perforation. Dig Endosc 30: 524.
- Zhu S, Lin J, Xu F, Guo S, Huang S, et al. (2019) Purse-string sutures using novel endoloops and repositionable clips for the closure of large iatrogenic duodenal perforations with single-channel endoscope: a multicenter study. Surg Endosc 33: 1319-1325.
- Passos ML, Ribeiro IB, de Moura DTH, Korkischko N, Silva GLR, et al. (2019) Efficacy and safety of carbon dioxide insufflation versus air insufflation during endoscopic retrograde cholangiopancreatography in randomized controlled trials: a systematic review and meta-analysis. Endosc Int Open 7: e487-e497.
- Muraki T, Arakura N, Kodama R, Maruyama M, Itou T, et al. (2013) Comparison of carbon dioxide and air insufflation use by non-expert endoscopist during endoscopic retrograde cholangiopancreatography. Dig Endosc 25: 189-196.
- Odemis B, Oztas E, Kuzu UB, Parlak E, Disibeyaz S, et al. (2016) Can a fully covered self-expandable metallic stent be used temporarily for the management of duodenal retroperitoneal perforation during ERCP as a part of conservative therapy? Surg Laparosc Endosc Percutan Tech 26: e9-e17.
- Tringali A, Pizzicannella M, Andrisani G, Cintolo M, Hassan C, et al. (2018) Temporary FC-SEMS for type II ERCP-related perforations: a case series from two referral centers and review of the literature. Scand J Gastroenterol 53: 760-767.
- Wu HM, Dixon E, May GR (2006) Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford) 8: 393-399.
- Park SM (2016) Recent advanced endoscopic management of endoscopic retrograde cholangiopancreatography related duodenal perforations. Clin Endosc 49: 376-382.
- Nentwich MF, Reeh M, Uzunoglu FG, Bachmann K, Bockhorn M, et al. (2016) Non-trauma emergency pancreatoduodenectomies: A single-center retrospective analysis. World J Surg 40: 2261-2266.
- Lissidini G, Prete FP, Piccinni G, Gurrado A, Giungato S, et al. (2015) Emergency pancreaticoduodenectomy: When is it needed? A dual non-trauma centre experience and literature review. Int J Surg 21: S83-S88.
- Cruvinel Neto J, Pereira BM, Riberio MA Jr, Rizoli S, Fraga GP, et al. (2014) Is there a role for pyloric exclusion after severe duodenal trauma? Rev Col Bras Cir 41: 228-231.
- Velmahos GC, Constantinou C, Kasotakis G (2008) Safety of repair for severe duodenal injuries. World J Surg 32: 7-12.
- Ivantury RR, Gaudino J, Ascer E, Ramirez-Schon G, Stahl WM, et al. (1985) Treatment of penetrating duodenal injuries: primary repair vs. repair with decompressive enterostomy/serosal patch. J Trauma 25: 337-341.
- Alfieri S, Rosa F, Cina C, Tringali A, Perri V, et al. (2013) Management of duodeno-pancreato-biliary perforations after ERCP: outcomes from an Italian tertiary referral center. Surg Endosc 27: 2005-2012.
- Krishna RP, Singh RK, Behari A, Kumar A, Saxena R, et al. (2011) Post-endoscopic retrograde cholangiopancreatography perforation managed by surgery or percutaneous drainage. Surg Today 41: 660-666.
- Fujikuni N, Tanabe K, Yamamoto H, Suzuki T, Tokumoto N, et al. (2011) Triple-tube-ostomy: a novel technique for the surgical treatment of iatrogenic duodenal perforation. Case Rep Gastroenterol 5: 672-679.
- Ali WM, Ansari MM, Rizvi SAA, Rabb AZ, Mansoor T, et al. (2018) Ten-year experience of managing giant duodenal ulcer perforations with triple tube ostomy at tertiay hospital at north India. Indian J Surg 80: 9-13.
Citation: Masahide Hiyoshi, Takashi Wada, Takeomi Hamada, Koichi Yano, Naoya Imamura and Atsushi Nanashima (2023) Management and outcome of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations: How to Determine and What is Recommended for Surgical Treatment?. J Emerg Med Trauma Surg Care 9: 067.
Copyright: © 2023 Masahide Hiyoshi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.