Neurorehabilitation Algorithms in Parkinsonism: Impact of Electrical Stimulations and Deep Oscillation on Autonomy and Quality of Life
*Corresponding Author(s):
Ivet B KolevaDepartment Of Physiotherapy At The Medical University Of Sofia, Department Of Physical And Rehabilitation Medicine At The Long-term Care Hospital “Serdika”-Sofia, Bulgaria
Tel:+359 888-20 81 61,
Email:yvette@cc.bas.bg
Abstract
Introduction: Parkinsonism (Prk) is a neurodegenerative disorder, considered as a socially important disease with serious decline in autonomy and quality of life of patients.
Objective: During last years, we estimated the efficacy of application of different physical modalities and neurorehabilitation methods on independence in activities of daily living and on quality of life of these patients.
The GOAL of current study was to evaluate qualitatively and quantitatively the impact of some preformed physical modalities [as Electrical Stimulations (ES) and Deep Oscillation (DO)] in the complex neurorehabilitation (NR) program in Prk-patients.
Materials & Methods: We observed 170 Prk-patients, covering the criteria of the Unified Parkinson’s Disease Rating Scale (UPDRS); randomized into five therapeutic groups (gr). In gr-1 we applied traditional physiotherapy (control group); In gr-2 a complex NR-programme, including physiotherapy, Ergotherapy & patients’ education. In patients of next groups, we added preformed physical modalities: In gr-3-electrical stimulations (ES) for feet extensors and flexors; in gr-4-Deep Oscillation (DO) paravertebrally; in gr-5-ES and DO.
For database management we used parametrical analysis (t-test-analysis of variances ANOVA) and non-parametric distribution analysis (Wilcoxon signed rank test); performed using SPSS package. The treatment difference was considered statistically significant if the P value was<0.05.
Results: Results demonstrate statistically significant amelioration (in allexperimental groups) concerning: brady-hypo-kinesia; gaitstability, pulsionphenomena (especiallyretropulsio); Hoehn and Yahr scale; Depression and Anxiety. Paravertebral pain, Rigidity (muscular and articularstiffness) and Prk-posture were most significantly influenced in gr-4 and gr-5. In gr-3 and gr-5 weperceivedmostimportantimprovement of autonomy in differentactivities, Timed Up and Go test, etc.
Conclusion: We recommend our own NR programme, including Physiotherapy, Occupational therapy, ES and DO; useful for the autonomy in activities of daily living of Parkinsonic patients.
Keywords
Parkinsonism; Neurorehabilitation; Functional electrostimulation; Deep oscillation; Autonomy in activities of daily living, Quality of life
ABBREVIATIONS
ADL: Activities of daily living
DO: Deep Oscillation
ES: Electrical Stimulations
ICD: International Classification of Diseases
ICF: International Classification of Functioning
NR: Neurorehabilitation
PD: Parkinsonic Disease
Prk: Parkinsonism
PRM: Physical and Rehabilitation Medicine
TUG: Timed Up and Go test
UPDRS: Unified Parkinson’s Disease Rating Scale
QoL: Quality of Life
INTRODUCTION
Parkinsonism (Prk) is a Neurodegenerative disorder, first described by Dr James Parkinson in 1817 as Shaking Palsy or Paralysis Agitans [1] and nowadays considered as a socially important disorder with inevitable progression and serious impact on autonomy and quality of life of patients [2].
Primary clinical patterns of Parkinsonic disease (PD) include: Static tremor, Muscle rigidity (Muscular and articular stiffness), Bradykinesia and Hypokinesia (including Hypomimia or Amimia), typical Prk-posture and Prk-gait, postural instability with pulsion phenomena (Antepulsion, Retropulsion, Lateropulsion) and frequent falls; Dysarthria and Dystonia [3,4]. There is a lot of non-motor autonomic and psychic signs and symptoms, especially Anxiety, depression, Apathy, Day-time somnolence and Insomnia; Pain, Fatigue, and (in some cases) dementia [3,5]. In advanced Prk-cases many movement problems are observed, e.g. freezing and on-off phenomena; peek-of-dose-dyskinesias; etc.
Routinely, the management of Prk includes predominantly drugs, functional neurosurgery and physiotherapy [4, 6-10]. The progressive degeneration with the subsequent early death of Dopaminergic neurons in the region of substantia nigra and the accumulation of the protein alpha-synuclein with the subsequent formation of Lewy bodies are the targets of many pharmaceutics (applied as Monotherapy or in combination): Levodopa, Dopamine agonists, MAO-B inhibitors, COMT-inhibitors, cerebro-protectors, ultimately-Vitamin B12, homocysteine, etc. Other authors propose transplantation of Dopaminergic tissue, use of Stem-cells, Gene-therapy or growth factor delivery in specific brain regions; stereotaxic thalamotomy, Deep brain stimulation, etc.
For satisfaction of typical patients’ and families’ concern, some patients’ organizations and associations suggest supportive therapies (as physiotherapy, occupational therapy, speech therapy, specific diet) and complementary therapies without sufficient scientific evidence (art-therapy, music therapy, Shiatsu, Reiki, massage, aroma-therapy, homeopathy, Bowen technique, etc.) [11].
In this field, the holistic approach of Physical and rehabilitation medicine (PRM) and of Neurorehabilitation (NR) may be convenient. Traditionally, the rehabilitation in PD includes physiotherapy and, in some cases, training in everyday activities [12].
During last years, our interest was oriented to the potential of Neurorehabilitation (NR) [13]. We elaborated a NR-program, adapted to dysfunctions and everyday problems of Prk-patients. The program includes Physiotherapy, Ergotherapy & patients’ education: exercises for paravertebral muscles and for extremities; soft tissue techniques for rigid muscles; balance, transfer and coordination training; grasp and gait training; speech and mimic exercises; training in activities of daily living [14].
Our objective was to combine different natural and preformed physical modalities and to estimate the efficacy of application of different neurorehabilitation methods on independence in activities of daily living (ADL) and on quality of life (QoL) of these patients. We must underline that the NR in PD is a team work of many medical specialists (medical doctors-specialists in Neurology, PRM, Gerontology) and health professionals (nurse, physical therapist, occupational therapist, speech therapist, neuropsychologist).
The GOAL of current study was to evaluate qualitatively and quantitatively the impact of some preformed physical modalities [as Electrical Stimulations (ES) and Deep Oscillation (DO)] in the complex neurorehabilitation (NR) program in Prk-patients.
MATERIALS AND METHODS
Study design
Our controlled prospective randomized double-blind investigation was effectuated during last years on a total of 170 patients, divided into 5 groups (34 patients for each one),
Outcome measures
During the period of the study we checked all patients with PD, hospitalized in our PRM Department. A detailed clinical and functional examination was performed for every patient, including history of the disease, date of the diagnosis PD; signs and symptoms of the Prk-syndrome; presence of pain; functional status, pathokinesiological analysis, independence in activities of daily living [15,16]. Special attention was paid to Hoehn and Yahr stage, pain evaluation, depression and anxiety; gait instability and activities limitations.
Eligibility criteria for participants
Our 170 patients were with diagnosed PD (G20 according the International Classification of Diseases-ICD-revision 10), with impairments, activity limitations and participation restrictions (according the International Classification of Functioning-ICF); covering the criteria of the Unified Parkinsonic Disease Rating Scale (UPDRS). The mean value of Hoehn and Yahr staging before NR was 2,7. The mean value of the Timed Up and Go test (TUG) before NR was 12.6 seconds.
After detailed analysis of potential participants and with the objective to assure data uniformity, we decided To put strong inclusion and exclusion criteria, as follows:
Inclusion criteria
Neurological diagnosis of idiopathic PD, proved by an university Neurological Clinic with clinical data and results of neuro-imagery (CT-scan or MRI) and neuro-functional investigations (electrodiagnostic, electroneurography, electromyography, incl. tremorogram); Reduced autonomy in ADL [functional grip, gait, activities] and reduced quality of life.
Exclusion criteria
We excluded Prk-patients with comorbidities, e.g.cerebro-vascular disease (after stroke); advanced cardiac insufficiency, severe osteoarthritis in hip or knee joints, levels 4 or 5 after Hoehn &Yahr staging (reduced physical capacity to realize physiotherapeutic training); cognitive impairments (dementia); changes in the medication in the period of the investigation (2 weeks before and 1 month after NR).
According the CONSORT (Consolidated Standards of Reporting Trials) 2010 statement [17], we present patients’ distribution and flow in the Table 1.
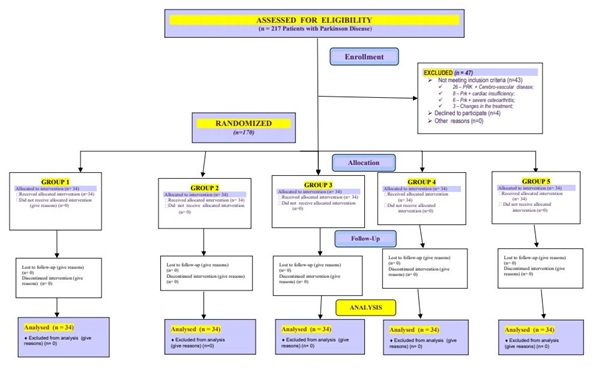
Table 1: Flow diagram.
We present the distribution of all 170 observed Prk-patients by age, by sex;by duration of the PD and by clinical syndrome in (figures 1-4).
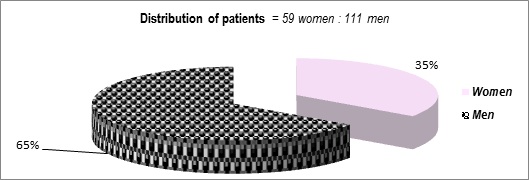
Figure 1: Distribution of patients (M:W).
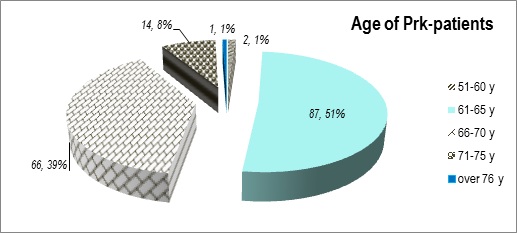
Figure 2: Distribution of patients (age).
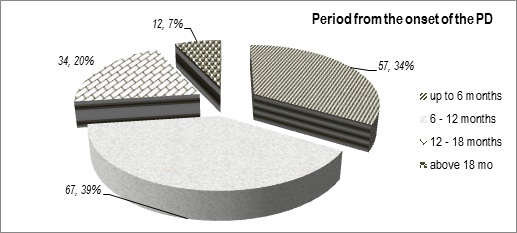
Figure 3: Duration of the PD (years from the onset).
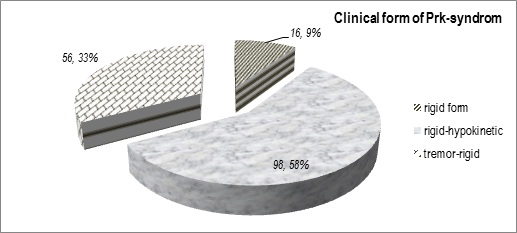
Figure 4: Distribution of patients (clinical form).
Our observed 170 Prk-patients were randomized into five therapeutic groups (gr)-one control group and four experimental groups.
In gr-1 we applied traditional physiotherapy (control group).
In patients of the experimental group we applied our own complex NR-program, including physiotherapy, Ergotherapy & patients’ education: analytic exercises for paravertebral muscles and for extremities; strengthening exercises and exercises for the range of motion of joints in upper and lower limbs; soft tissue techniques for rigid muscles; balance, transfer and coordination training; respiratory exercises; speech and mimic exercises; training in activities of daily living-postural control, position therapy, transfers, verticalization; grasp and gait training; self-service activities (bathing, eating, etc.).The complex NR-program must be exercised every day for 60 minutes, in front of a mirror; under the control of a physiotherapist.
The experimental group was divided into four sub-groups (gr-2, gr-3, gr-4, gr-5).
Patients of gr-2 received only this complex NR-program.
In patients of next groups, we added preformed physical modalities:
- • in gr-3-electrical stimulations (ES) with pulses of low frequency electric currents for feet extensors and flexors; 10-20 mili-Ampers, 15-20 minutes;
- • in gr-4-Deep Oscillation (DOwith parameters: 5-7 micro-Ampers, 15-30 minutes; frequency 140-200 Hz) paravertebrally;
- • in gr-5-FES and DO.
The duration of the NR was one month (20 working days).
For database management we used parametrical analysis (t-test-analysis of variances ANOVA) and non-parametric distribution analysis (Wilcoxon signed rank test); performed using SPSS package. The treatment difference was considered statistically significant if the P value was
Ethical aspects
Investigations were realized in accordance with the requirements for defense of patients’ rights (Declaration of Helsinki, 1964) and were approved by the respective institutional and Ethical Committees. Before the investigations, we explained to every one of patients the correspondent elements of the NR-program and of the design of investigations. Every patient signed an informed consent for the NR-course and for respective investigations.
We investigated our patients before and after NR-program and one month later in accordance to the respective Protocol.
Details of organization of the study, randomization and blinding
A simple randomization was used. Patients were sequentially numbered and randomized into five treatment groups of 34 each one.
According recommendations [18,19] the investigation was realized by a multi-professional team; including: a medical doctor-specialist in Physical and rehabilitation medicine (PRM) and in Neurology (author 1). The physical therapy complex was performed by a physical therapist, with sub-specialization in the field of Neurological Rehabilitation (co-author 2). A specialist in Information Technologies performed the statistical analysis (co-author 3). The medical doctor provided the exams of patients (before, during and after treatment) without information concerning the NR-complex. The physical therapist oriented every first patient to gr 1, every second patient-to gr 2, etc. The mathematician had not information about patients’ personal data and the NR-complex; he had only investigations’ results. The details of the series were revealed to investigators after the end of the study.
RESULTS AND ANALYSIS
The comparative analysis of the results demonstrates statistically significant amelioration (in all experimental groups) concerning: brady-hypo-kinesia; gaitstability, pulsionphenomena (especially retropulsion); Hoehn and Yahr scale;depression and anxiety; autonomy and quality of life of Prk-patients. Paravertebral pain, rigidity (muscular and articular stiffness) and Prk-posture were most significantly influenced in gr-4 and gr-5. In gr-3 and gr-5 we perceived most important improvement of data of Timed Up and Go test (TUG) and of autonomy of patients in differentactivities.
During the evaluation of the dynamics in the severity of PD using the Hoehn and Yahr Staging before and after NR (Figure 5), we observed a translation of the Gauss curvature of distribution towards the minor levels, respecting the diminution of the Wilcoxon meridian.
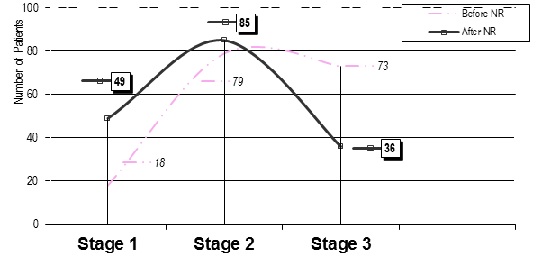
Figure 5: Functional assessment (Hoehn&YahrStaging Scale).
The most important result for us is the augmentation of patients’ autonomy in self-service activities (movements in bed, bathing, dressing, eating, mobility at home, etc.) and home-based and transport activities (food preparation, home hygiene, activities with upper and lower extremities, transportation, etc.). Next Figure 6 and Figure 7 present the efficacy of NR on patients’ autonomy. The scale of evaluation is between zero and five (complete dependence 0to complete independence 5). We can observe positive results in autonomy-in all experimental groups (gr-2 to gr-5).
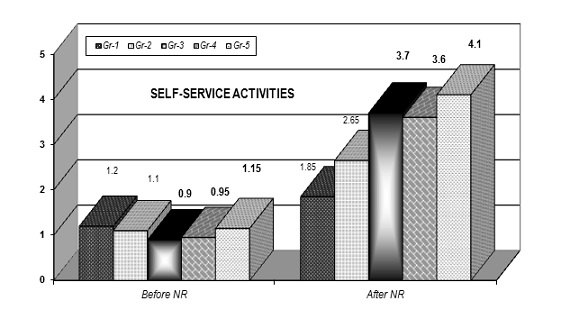
Figure 6: Evaluation of autonomy in self-service activities (0-5).
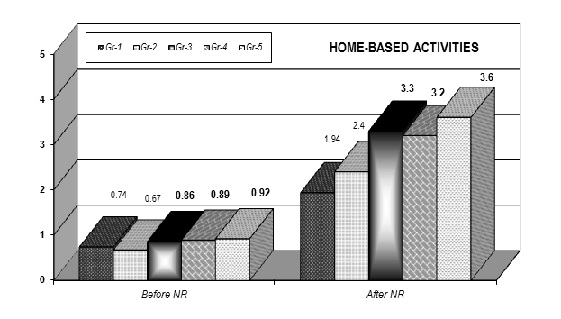
Figure 7: Evaluation of autonomy in home-based activities (0-5).
The paravertebral pain, due to specificity of Prk-posture, interferes with for patient’s quality of life. We evaluated the intensity of paravertebral pain by the Visual Analogue Scale (VAS 0-10). The next Figure 8 presents the decrease of pain sensation, most important in gr-4 and gr-5 (treated with Deep Oscillation).
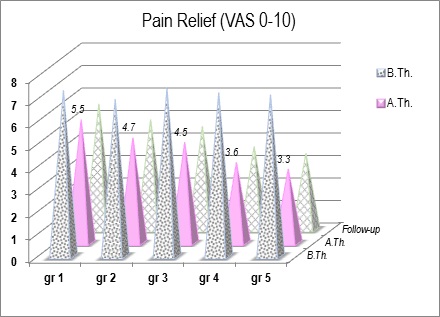
Figure 8: Pain relief (VAS 0-10; no pain, to worst pain).
Psychological condition of PRK-patients was assessed through the Express Scales of Zung-for Depression (D) and Anxiety (A). Next Figure 9 presents the values of Zung-D-before NR (B.NR) and after NR (A.NR). Before NR the results of Zung-D were in the field of moderate depression (48-55 points). In experimental groups we observed a translation of results of Zung-D to the levels of mild depression (41-47 points) or no depression (under 40 points). Reduction of depression was stable during the follow-up (one month after the end of the NR-course). The observed correlation with the pain relief probably objectivizes the efficacy of pain reduction.
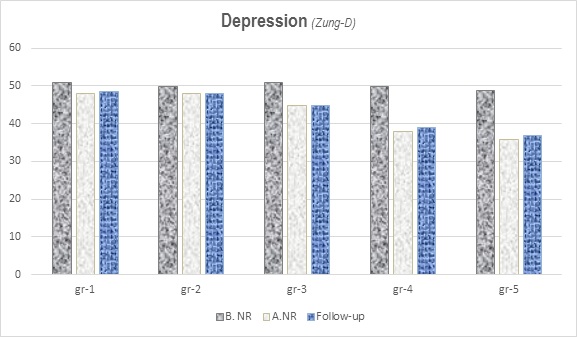
Figure 9: Depression (Zung-D).
The gait stability, the velocity of reaction and of gait were significantly improved in all experimental groups, especially in gr-3 and gr-5 (with electrical stimulations) (Table 2) (Figure 10).
|
TUG Test |
Before NR |
After NR |
Mean Difference , Standard deviation (B.NR-A.NR) |
|
Gr 1 |
12.4 |
10.4 |
2.0/SD 1.38 |
|
Gr 2 |
12.6 |
9.7 |
2.9/SD 1.47 |
|
Gr 3 |
12.5 |
8.3 |
4.2/SD 1.46 |
|
Gr 4 |
12.8 |
9.4 |
3.4/SD 1.37 |
|
Gr 5 |
12.7 |
8.1 |
4.6/SD 1.42 |
Table 2: Values of the Timed Up and Go test (before and after NR) (in seconds).
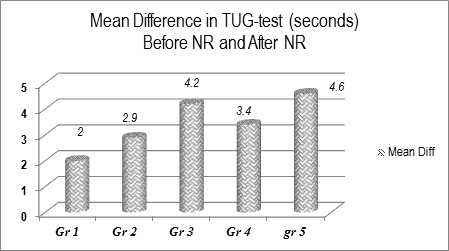
Figure 10: Mean Difference in data before and after NR of the Timed Up and Gotest (in seconds).
DISCUSSION
Neurorehabilitation and use dependent neuroplasticity
We made a composition, clinical application and approbation of complex neurorehabilitation algorithms in Prk-patients. The goal was to evaluate the efficacy of application of different natural and preformed physical modalities and NR-methods on independence in activities of daily living (ADL) and quality of life of patients with this socially important neurodegenerative disease.
The comparative analysis of our results demonstrates a statistically significant amelioration (in all experimental groups) concerning: Prk-signs and symptoms, especially gaitstability, Hoehn and Yahr scale; depression and anxiety; autonomy in everydayactivities. The pain relief was most important in groups with Deep Oscillation.Wedetectedsignificantimprovement of data of TUG-test and of autonomy of patients in differentactivities in groups with electricalstimulations. No efficacy of NR on Static tremor.
We observed significant efficacy of our NR-algorithms on functional autonomy of Prk-patients, without medication modifications. This is an approval of the law “Use and Disuse” of Jean Baptiste Lamarck: “The more frequent and continuous use of any organ gradually strengthens and develops that organ…”. Probably this is the training of use-induced and activity-dependent neuronal plasticity, similarly as in NR after stroke [13, 15,20].
We proved that neurorehabilitation can be useful in Prk-patients, but only in case of systematic and prolonged NR-courses, adapted to the individual patient, in the concrete moment of progression of this neurodegenerative disease. In these cases, we must apply the SMART-approach (Specific, Measurable, Achievable, Realistic and Timebound).We must choose the NR tools with potential to rewire cerebral functions and to excite the formation of new connections and pathways, respectively to stimulate the brain reorganization and adaptation to the ‘new’ situation (appearance of a damaged locus in the cerebral tissue), in other terms - to help functional recovery through potentiation of use-induced and use-dependent neuroplasticity. We must apply the “neurorehabilitation puzzle”-a synergic combination of different physical modalities (electric currents, movement, activities, etc.). For functional evaluation in NR we must apply neurological scales and the International Classification of Functioning (ICF).
Practical Issues from our Study
Rehabilitation is a functional therapy, based on detailed functional assessment.
NR is a cheap and useful option for increase the patients’ quality of life.
Electrical stimulations are useful for gait stability of Prk-patients and for their autonomy in ADL.
Deep Oscillation is an effective preformed physical modality with significant anti-pain effect.
The patient education must be adapted to the needs of every concrete patient, including other types of patients, excluded from our study (e.g. Prk due to other causes: cerebro-vascular disease, etc.).
FUTURE DIRECTIONS
We consider that, in the future, investigators must observe the efficacy of other preformed physical modalities on Prk-cases. A comparison between different physical factors can be useful for the management protocol in this type of patients.
CONCLUSION
Physiotherapy and Ergotherapy are useful for the autonomy of Prk-patients. Preformed physical modalities can ameliorate the efficacy of NR: Electrical Stimulations are useful for gait stability, Deep Oscillation-for pain relief and correction of depression.
The complex NR-program is effective for improvement of the neuromuscular coordination, respectively for the autonomy of patients in everyday life.
In conclusion, we recommend our own NR program, including physiotherapy, occupational therapy, patient education, electro stimulations and deep oscillation.
REFERENCES
- Parkinson J (1817) An Essay on the Shaking Palsy. London: Sherwood, Neely and Jones.
- Gómez Esteban JC, Zarranz JJ, Lezcano E, Tijero B, Luna A, et al. (2007) Influence of motor symptoms upon the quality of life of patients with Parkinson’s disease. Eur Neurol: 57: 161-165.
- De Maagd G, Philip A (2015) Parkinson's Disease and Its Management: Part 1: Disease Entity, Risk Factors, Pathophysiology, Clinical Presentation, and Diagnosis. PT 40: 504-532.
- Smith Y, Wichmann T, Factor SA, Delong MR (2011) Parkinson’s disease therapeutics: New developments and challenges since the introduction of levodopa. Neuropsychopharmacology 37: 213-246.
- Argüelles JL, Carvajal ABR, Alba GG, Aguila LMS, Manso LM (2019) Factors Related with Frontal Dysfunction in Early Stages of Parkinson Disease. J Alzheimers Neurodegener Dis 5: 018.
- Jankovic J, Poewe W (2012) Therapies in Parkinson’s disease. Curr Opin Neurol 25: 433-447.
- Mc Carter SJ, Teigen LM, McCarter AR (2019) Low Vitamin B12 and Parkinson Disease. Mayo Clinic Proceedings 94: 757-762.
- Green R, Christine CW (2019) Linking vitamin B12 and a trembling disorder. Cell Research 29: 343-344.
- Murray LK, Jadavji NM (2019) The role of one-carbon metabolism and homocysteine in Parkinson’s disease onset, pathology and mechanisms. Nutrition Research Reviews 32: 218-230.
- Kim SN, Wang X, Park HJ (2019) Integrative Approach to Parkinson's Disease. Front Aging Neurosci 11: 339.
- https://www.parkinsons.org.uk/sites/default/files/2018-11/B102%20Complementary%20therapies%20WEB.pdf
- Pellechia MT, Grasso A, Bincardi LG, Squillante M, Bonavita V, et al. (2004) Physical therapy in Parkinson’s disease: An open long-term rehabilitation trial. J Neurol 251: 595-598.
- Koleva IB, Yoshinov BR, Yoshinov RR. (2019) Clinical Neurorehabilitation. Monograph. Edited by I Koleva. - Sofia: ‘SIMEL Press’, 678 pp.
- Yoshinov BR, Koleva IB, Same M, Krastav N (2019) Clinical approval of our own neurorehabilitation programme for parkinsonic patients. Journal of Physiotherapy & Physical Rehabilitation 4: 58.
- Koleva IB, Avramescu ET (2017) Grasp and gait rehabilitation (bases). Monograph- Sofia: ‘SIMEL Press’, 396 p
- Koleva I, Yoshinov R, Yoshinov B (2018) Physical Analgesia. I Koleva. Saint-Denis (France): Connaissances et Savoirs-Sciences Sante,146 pp. Monograph.
- Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 340: c332.
- European Physical and Rehabilitation Medicine Bodies Alliance (2018) White Book on Physical and Rehabilitation Medicine in Europe. Chapter 4. History of the specialty: Where PRM comes from. Eur J Phys Rehabil Med 54: 186-197.
- European Physical and Rehabilitation Medicine Bodies Alliance (2018) White Book on Physical and Rehabilitation Medicine in Europe. Introductions, Executive Summary, and Methodology. Eur J Phys Rehabil Med 54: 125-155.
- Koleva I (2009) Neurorehabilitation algorithms for functional recovery and amelioration of independence in everyday activities of patients with socially important invalidating neurological diseases. Thesis for Doctor in Medical sciences. Sofia.
Citation: Koleva IB, Yoshinov BR, Yoshinov RR (2020) Neurorehabilitation Algorithms in Parkinsonism: Impact of Electrical Stimulations and Deep Oscillation on autonomy and quality of life. J Alzheimer’s Neurodegener Dis 6: 043.
Copyright: © 2020 Ivet B Koleva, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.