
Proximal Foot and Sole Soft Tissue Defect Reconstruction with Distally Based Pedicle Flaps: An Approach with Hyperbaric Oxygen Therapy as a Tool
*Corresponding Author(s):
Pradeoth Korambayil MukundanDepartment Of Plastic Surgery And Burns, Jubilee Mission Medical College & Research Institute, Consultant Plastic Surgeon, Thrissur, Kerala, India
Tel:+919048935409,
Email:pradeoth@gmail.com; drpvarkey@gmail.com; k.rameela@gmail.com
Abstract
Background: Soft tissue cover over the lower part of the leg, the ankle and the foot, is a difficult task for plastic surgeon especially with exposure of bones or tendons. Main options are distant tissue transfer, reverse distally based flaps available for covering soft tissue defect in these areas. The aim of the study is to know the effectiveness of hyperbaric oxygen therapy as an adjunct for flap coverage.
Methods: Sixteen patients with soft tissue defect of foot and lower third leg region were treated over a period of 7 months. The lateral supramalleolar flap was used in 11 cases and distally based sural flap was used in 5 cases for the reconstruction of skin defects of the ankle and foot that exposed the bone or tendons. Hyperbaric oxygen therapy was used as an adjunct in the management of soft tissue defects which requires a distally based flap cover.
Results: Of the 16 patients, 10 were males and 6 were females, with a range 13 to 72 years. The length of the flap varied from 4 cm to 14 cm (mean 6.5 cm) and the width varied from 4 cm to 5 cm (mean 4.1 cm). Superficial necrosis developed in one lateral supramalleolar flap, but this was successfully treated by debridement skin graft. Among the sixteen flaps, thirteen cases survived completely. The soft tissue defect was due to trauma in 13 cases, assault in one case, tumor in one case and osteomyelitis in one case. Out of sixteen cases, seven were islanded fasciocutaneous lateral supramalleolar, two was fasciocutaneous lateral supramalleolar, one was adipofasciallateral supramalleolar, one was propeller type lateral supramalleolar, three were extended reverse sural and two were island reverse sural flap in nature. Two cases had necrosis at the tip of the flap managed conservatively. The donor site morbidity was minimal.
Conclusion: The Lateral supramalleolar flap and distally based sural flap with hyperbaric oxygen therapy as an adjunct improves survival of medium sized soft tissue defects in these regions.
Keywords
Hyperbaric oxygen therapy; Lateral supramalleolar flap; Reverse sural flap; Soft tissue reconstruction
INTRODUCTION
Various techniques ranging from a skin grafting to free-tissue transfer, have been used to reconstruct the soft tissue defect of the sole and proximal foot regions although only few have yielded entirely satisfactory results[1].A safe, easy and reliable reconstructive option must be available for the reconstruction of thelower third leg and foot region. The lateral supramalleolar flap[2,3]is raised on the lateral aspect of the lower leg and the flap is vascularized by a perforating branch of the dorsal peroneal artery. The lateral supramalleolar flap is commonly used for coverage that includes the whole dorsum of the foot, the medial and the lateral arches and all the regions of the heel. The reverses Ural flap[4,5] is raised on the posterior aspect of the calf, and the anatomical structures included in the pedicle are the superficial and deep fascias, the sural nerve, the lesser saphenous vein and the superficial sural artery. Reverse sural flap is commonly used for coverage of the hind foot, dorsum and the region of the lateral malleolus. In this prospective study, along with the distally based flap cover for soft tissue defect over the lower third leg and foot region. Hyperbaric oxygen therapy was utilized as an adjunct to preserve marginal tissue, treat compartment syndrome and aid flap delay for the soft tissue reconstruction of foot and lower third leg. The aim of the study is to know the effectiveness of hyperbaric oxygen therapy as an adjunct for flap coverage.
MATERIALS AND METHODS
Sixteen patients with soft tissue defect of foot and lower third leg region were treated over a period of 7 months (December 2012 to June 2013). Ethical clearance for the study was obtained from the Institution. Proper Informed consent was obtained from the patient participating in the study. Patients were informed about the line of management, possible treatment modalities, need for additional surgical procedures pertaining the pattern of injuries. Thorough wound debridement, fixation of fractures and planning of reconstruction was done. If the wound was fit for flap cover then immediate reconstruction was performed. Hyperbaric oxygen therapy was initiated during the immediate post-operative period. A session of six hyperbaric oxygen therapy, one session extending to 1hr for six days was administered to the patients post operatively. Severity of injury, time of referral, comorbid condition, age of the patients, reach of the flap were considered as factors to subject the patient for flap delay with associated hyperbaric oxygen therapy. In case of extended reverse sural flap, after initial debridement, priming was planned with hyperbaric oxygen therapy. On post debridement day 2, flap delay was done and flap inset was completed on post debridement day 4. Hyperbaric oxygen therapy sessions were administered extending to 6-12 sessions accordingly depending on the flap healing status.Immobilization of the limb was done all patients for three weeks. Outcome following different types of management and secondary procedures performed were noted.
Surgical technique
The perforating branch of the peroneal artery for lateral supramalleolar fasciocutaneous flap pierces the interosseous membrane at the distal tibio-fibular angle about 5 cm proximal to the tip of the lateral malleolus. The lateral supramalleolar flap contains the superficial peroneal nerve, the perforating branch from the peroneal artery and the venae comitantes.
The reverse sural flap was outlined at the junction of the two heads of the gastrocnemius muscle. A line of incision was marked over the presumed course of the sural nerve and the lesser saphenous vein. The pivotal point of the pedicle was 5-7cm proximal to the tip of the lateral malleolus. Marking up the perforators with handheld Doppler will help in adjusting the pivotal point at appropriate level to preserve vascularity to the flap. The flap was raised including the fascia. When planned for extended reverse sural flap, fascia in between the gastrocnemius muscle was preserved. Extended reverse sural flaps done in the series were always delayed. Flap was delayed if the territory of the flap exceeds the middle or lower third marking of the reverse sural flap or if the flap was based on upper most perforator due to the extension of zone of injury. During the first stage of delay, the flap was raised till the pedicle region and kept in position. During the second stage, flap inset was completed.
OBSERVATION AND RESULTS
The soft tissue defect was due to trauma in 13 cases, assault in one case, tumor in one case and osteomyelitis in one case (Table 1). Of the 16 patients, 10 were males and 6 were females, with a range 13 to 72 years (mean 36.12yrs).Two patients had diabetes mellitus as co-morbid illness. Among the sixteen cases, five were chronic wounds and 11 were acute wounds. The lateral supramalleolar flap was used in 11 cases and distally based sural flap was used in 5 cases for the reconstruction of skin defects of the ankle and foot that exposed the bone or tendons. The length of the flap varied from 4 cm to 14 cm (mean 6.5 cm) and the width varied from 4 cm to 5 cm (mean 4.1 cm).. Out of sixteen cases, seven were islanded fasciocutaneous lateral supramalleolar, two was fasciocutaneous lateral supramalleolar, one was adipofascial lateral supramalleolar, one was propeller type lateral supramalleolar, three were extended reverse sural and two were island reverse sural flap in nature. Two cases had necrosis at the tip of the flap managed conservatively. Superficial necrosis developed in one lateral supramalleolar flap, but this was successfully treated by debridement and skin grafting. Except for two flaps with tip and superficial necrosis, rest of the flaps survived completely (Table 1). Functional recovery and bony union was adequate in all treated patients. We present four crucial cases which were salvaged by combination of hyperbaric oxygen therapy to flap cover. In case 1, the flap with onset of tip necrosis was salvaged.In the second case, an extended flap with association of flap delay process was salvaged using hyperbaric oxygen therapy. In third case, a patient with compartment syndrome where the chances of flap failure is high was salvaged by hyperbaric oxygen therapy and in final case, an adipofascial flap was salvaged by adjunct hyperbaric oxygen therapy.
|
No. |
Age/Sex |
Trauma /Etiology |
Site & duration of wound |
Defect Size |
Flap Size |
Details |
Type of flap |
Complications& secondary procedure |
|
1 |
27/M |
Road traffic accident |
Anterior aspect Medial side ankle region (Acute) |
6×4cm |
7×4 |
Defect exposing the tibialis anterior tendon |
Islandfasciocutaneous flap Lateral supra malleolar |
nil |
|
2 |
43/M |
Road traffic accident |
Proximal foot dorsal aspect medial side(Acute) |
6×4cm |
7×4 |
Defect exposing the base of first metatarsal bone |
Island fasciocutaneous flap Lateral supra malleolar |
Tip discloration + No secondary intervention |
|
3 |
45/F |
Tumor |
Lateral malleolarregion(Acute) |
5×4cm |
6×4 |
Defect exposing lateral malleolus |
Propeller type flap Lateral supra malleolar |
nil |
|
4 |
36/F |
Road traffic accident |
Midfoot dorsum (Acute) |
4×4 cm |
5×4 |
Defect exposing the second metatarsal bone shaft |
Island fasciocutaneous flap Lateral supra malleolar |
nil |
|
5 |
40/F |
Road traffic accident |
Mid-distal junction of dorsum of foot (Acute) |
6×4cm |
NA |
Defect exposing the extensor tendons of 2nd , 3rd , 4th, 5th toe |
Adipofascial flap Lateral supra malleolar |
nil |
|
6 |
54/M |
Road traffic accident |
Mid - distal junction of dorsum of foot (chronic) |
4×4cm |
5×4 |
Defect exposing the extensor tendons of 2nd , 3rd , 4thtoe |
Island fasciocutaneous flap Lateral supra malleolar |
nil |
|
7 |
45/M |
Assault |
Tibial bone distal end (chronic) |
4×3cm |
7×5 |
Osteomyelitis of tibila bone,curettage done |
Fasciocutaneous Lateral supra malleolar |
nil |
|
8 |
21/M |
Road traffic accident |
Proximal foot dorsal aspect medial side (acute) |
4×5cm |
5×5 |
Defect exposing the EHL tendon and ligaments |
Island fasciocutaneous flap Lateral supra malleolar |
nil |
|
9 |
26/M |
Road traffic accident |
Mid - distal junction of dorsum of foot (Acute) |
4×3cm |
4×4 |
Defect exposing the extensor tendons of 2nd , 3rd , 4thtoe |
Island fasciocutaneous flap |
Necrosis tip region managed conservatively |
|
10 |
32 /F |
Road traffic accident |
Medial malleolar region (Acute) |
5×4cm |
5×5 |
Defect exposing the medial malleolar region with compartment syndrome |
Lateral supra malleolar |
Superficial flap necrosis Managed by skin grafting |
|
11 |
13yr /F |
Osteomyelitis |
Medial malleolarregion(chronic) |
4×3cm |
4×4 |
Defect exposing the medial malleolar region |
Island reverse sural artery flap cover |
nil |
|
12 |
34yrs/M |
Road traffic accident |
Heel pad calcaneal and tendoachillesregion(chronic) |
13×5 cm |
14×5 |
Defect exposing calcaneum and heel pad region |
Extended reverse sural artery flap cover |
nil |
|
13 |
24yrs/M |
Road traffic accident |
Lateral malleolus and dorsum of foot (Acute) |
12×5cm |
13×5 |
Defect over lateral malleolus and dorsum of foot |
Extended reverse sural artery flap cover |
nil |
|
14 |
43yrs/F |
Road traffic accident |
Calcaneal and tendoachilles region (chronic) |
5×4cm |
6×4cm |
Defect over the calcaneal and tendoachilles region |
Extended reverse sural artery flap cover |
nil |
|
15 |
23yrs/M |
Road traffic accident |
Calcaneal and tendoachilles region ( Acute) |
6×4 cm |
7×4cm |
Defect over the calcaneal and tendoachilles region |
Reverse sural artery flap cover |
nil |
|
16 |
72 yrs/ |
Road traffic accident |
Medial malleolar region (acute) |
4×3cm |
4×4 |
Defect exposing the medial malleolar region |
Lateral supra malleolarfasciocutaneous |
nil |
Table 1: Representing the patients participated in the study, Flap utilized for reconstruction and outcome
Case 1
A 43yrs male admitted with crush injury to the right ankle and foot region due to road traffic accident. Patient presented with soft tissue loss over the medial aspect of the right ankle and foot region exposing the base of the first metatarsal bone and tarsometatarsal joint (Figure 1).
 Figure 1: Soft tissue loss over the medial aspect of the right ankle and foot region exposing the base of the first metatarsal bone and tarsometatarsal joint.
Figure 1: Soft tissue loss over the medial aspect of the right ankle and foot region exposing the base of the first metatarsal bone and tarsometatarsal joint.
After bony stabilization, soft tissue coverage was done with island lateral supramalleolar flap and donor site covered with split thickness skin grafting (Figure 2,3).
 Figure2: Soft tissue coverage was done with island lateral supramalleolar flap.
Figure2: Soft tissue coverage was done with island lateral supramalleolar flap.
 Figure 3: Donor site covered with split thickness skin grafting.
Figure 3: Donor site covered with split thickness skin grafting.
Hyperbaric oxygen therapy was administered for 12 sessions postoperatively. Patient developed discoloration of the tip of the flap which settled down without any secondary intervention (Figure 4,5).
 Figure 4: Discoloration of the tip of the flap due to venous congestion.
Figure 4: Discoloration of the tip of the flap due to venous congestion.
 Figure 5: Tip discoloration settled down with conservative management with hyperbaric oxygen therapy.
Figure 5: Tip discoloration settled down with conservative management with hyperbaric oxygen therapy.
Case 2
A 34 yrs male with crush injury to the right heel pad and ankle region was referred to our center after three weeks following injury. Patient presented with necrotic heel pad region with multiple lacerations over the ankle region both on medial and lateral aspect (Figure 6-8).
 Figure 6: Crush injury to the right heel pad and ankle region with multiple laceration medial aspect of foot.
Figure 6: Crush injury to the right heel pad and ankle region with multiple laceration medial aspect of foot.
 Figure 7: Picture showing necrotic heel pad tissue.
Figure 7: Picture showing necrotic heel pad tissue.
 Figure 8: Crush injury to the right heel pad and ankle region with multiple laceration lateral aspect of foot.
Figure 8: Crush injury to the right heel pad and ankle region with multiple laceration lateral aspect of foot.
Wound was debrided (Figure 9) and hyperbaric oxygen therapy sessions were started. On post debridement day 2, Extended reverse sural flap elevated and flap delay done (Figure 10, 11) continuing the hyperbaric sessions.
 Figure 9: Extended reverse sural artery flap was elevated on day 2 following debridement.
Figure 9: Extended reverse sural artery flap was elevated on day 2 following debridement.
 Figure 10: Extended reverse sural artery flap delay done.
Figure 10: Extended reverse sural artery flap delay done.
 Figure 11: Flap inset was completed on day 4 following debridement.
Figure 11: Flap inset was completed on day 4 following debridement.
On post debridement day 4, flap inset completed. Donor area covered with split thickness skin graft.Hyperbaric oxygen therapy was administered for 12 sessions. Post-operative period was uneventful (Figure 12).
 Figure 12: Picture showing the flap position over the heel pad region- late post-operative period.
Figure 12: Picture showing the flap position over the heel pad region- late post-operative period.
Case 3
A 32 yrs female admitted with crush injury of the right foot and lower third leg exposing the medial malleolus (Figure 13). Patient had an associated compartment syndrome of the leg. Wound was debrided and fasciotomy done. Island lateral supramalleolar flap was used to cover the defect over the bony region (Figure 14) and rest of the raw area was covered with skin grafting. Hyperbaric oxygen therapy was administered for 12 sessions. There was superficial tissue necrosis of the flap which was later managed by split thickness skin grafting(Figure 15).
 Figure 13: Crush injury of the right foot and lower third leg exposing the medial malleolus with compartment syndrome.
Figure 13: Crush injury of the right foot and lower third leg exposing the medial malleolus with compartment syndrome.
 Figure 14: Island lateral supramalleolar flap was used to cover the defect over the bony region.
Figure 14: Island lateral supramalleolar flap was used to cover the defect over the bony region.
 Figure 15: Post-operative picture following skin grafting over the area of superficial necrosis of flap.
Figure 15: Post-operative picture following skin grafting over the area of superficial necrosis of flap.
Case 4
A 40 yrs female admitted with crush injury of the right foot dorsum with soft tissue loss exposing the extensor tendons (Figure 16). Wound was debrided and adipofascial lateral supramalleolar flap was used to cover the defect. Split thickness skin graft was used to cover adipofascial flap. Hyperbaric oxygen therapy was administered for six sessions following the procedure. Post-operative period was uneventful (Figure 17).
 Figure-16: Crush injury of the right foot dorsum with soft tissue loss exposing the extensor tendons.
Figure-16: Crush injury of the right foot dorsum with soft tissue loss exposing the extensor tendons.
 Figure17: Adipofascial lateral supramalleolar flap was used to cover the defect. Skin grafting done over the flap.
Figure17: Adipofascial lateral supramalleolar flap was used to cover the defect. Skin grafting done over the flap.
DISCUSSION
Venous congestion appears to be the common complication in the distally based flap from the lower extremity. Its seems to be related to the compression of the pedicle due to lack of elasticity in the skin over the roof of the tunnel in islanded variety, valvular incompetence, edema at the pedicle region or compartment syndrome, or compression of the pedicle by a hematoma. Almeida et alreported on the complications in their 71 cases of a reverse-flow island sural flap, including partial (22.1%) or total (4.2%) flap necrosis, infection (8.5%) and venous congestion (4.1%)[4]. Ehab et al. described five out of twenty five lateral supramalleolar flaps suffered venous congestion, two of them managed conservatively, two required suturing after excision of necrotic tissue and one required hemisoleus muscle flap to cover the defect[7]. Vocheet alreported venous congestion and partial flap necrosis (5 to 30%) in 41 cases of using the lateral supramalleolar flap for ankle and foot defects[3].
Kneser et al.suggested a delayed neurofasicocutaneous sural flap, which is initially completely elevated and it is then fixed again at the donor site using running sutures for 7 to 15 days[5]. After confirming the flap’s survival, the reverse sural flap was raised again and transposed into the soft tissue defect. This delayed procedure could be an alternative to overcome these problems and to increase the reliability and viability of the distally based fasciocutaneous flap. Tan et al.[8] treated three patients with a supercharged reverse flow sural flap to reduce venous congestion and edema, and the venous drainage was achieved by end-to-end anastomosis between the free end of the lesser saphenous vein and a superficial vein on the medial site of the ankle.
Principle of utilizing hyperbaric oxygen therapy in vascular insufficiency ulcers and radiation induced wounds could well be applied in salvaging this distally based fasciocutaneous flaps. Hyperbaric oxygen therapy utilizes 100% oxygen at pressures greater than atmospheric pressure. In our unit, Hyperbaric Oxygen was administered in a Monoplace chamber wherein a single patient is placed in a chamber which is then pressurized with 100% Oxygen. Vasoconstriction reduces edema and tissue swelling while ensuring adequate oxygen delivery and is thus useful in acute trauma wounds. Hyperoxygenation of the crush injury, compartment syndrome and flap salvage causes immune stimulation by restoring WBC function and enhancing their phagocytic capabilities and neo-vascularization in hypoxic areas by augmenting fibroblastic activity and capillary growth[9]. Adequate shock management, debridement and repair of soft tissues and stabilisation of bony elements are of paramount importance. Hyperbaric oxygen therapy as an adjunct should be administered as early to prevent large expanses of ischaemic necrosis, minimise the frequency and extent of tissue necrosis, reduce oedema, control infection, support healing and prevent reperfusion injury[10]. Ersin et al. [11] illustrating the usefulness of hyperbaric oxygen treatment during the delay period of the flap which can lessen the time period needed for the delay procedure and increase the effect of the flap delay will aid us in administrating hyperbaric therapy for heel pad avulsion injuries. We utilized this principle for extended distally based flaps where we did a delay procedure and shortened the duration of delay to obtain a better outcome. We experienced fewer complications to the flaps following this approach. However, more data and series of study are required to determine additional indications as well as optimal timing and dosing for hyperbaric oxygen therapy for delay procedures of distally based flaps.
At our institution, we have developed a strategy to overcome these difficulties and successfully manage these patients with lower third leg and foot defect by a combined approach that maximizes tissue perfusion and oxygenation, allowing for optimal surgical correction which requires distally based flap cover for proximal foot injuries. Our treatment algorithm begins with surgical debridement and initiation of hyperbaric oxygen therapy at the earliest. Monoplace chamber is provided with adequate space for leg elevation by means of pillow postoperatively. Combination of the modalities possibly allows preservation of marginal tissue, prevention of ischemic and hypoxic advancement, reduction of tissue edema or congestion and maximum preservation of transferred distally based flap.
We did not face any complications for the transferred flaps except in one patient with compartment syndrome who experienced superficial necrosis which was salvaged by skin grafting procedure. In patients with early compartment syndrome due to crush injury, hyperbaric oxygen therapy may reduce the penumbra of cells at risk which may be subjected for delayed necrosis and secondary ischemia [12].The patients in our series did not experience the common side effects of hyperbaric oxygen therapy like aural or pulmonary barotraumas, transient reversible myopia during the treatment. Measures that could improve the outcome of distally based flaps with the adjunctive use of hyperbaric oxygen therapy should be considered at the earliest. When the defects are larger, free tissue transfer is often required[13].An algorithm for management of injuries involving the foot requiring distally based flap cover with hyperbaric oxygen therapy as an adjunct is enumerated in Figure 18.
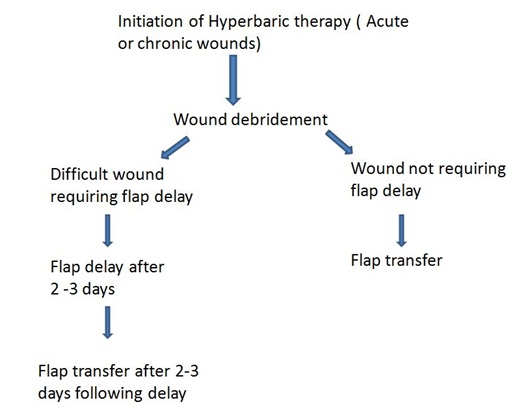 Figure 18: Algorithm for the management for Flap cover with hyperbaric oxygen therapy as an adjunct.
Figure 18: Algorithm for the management for Flap cover with hyperbaric oxygen therapy as an adjunct.CONCLUSION
REFERENCES
- Sommerlad BC, McGrouther DA (1978) Resurfacing the sole: long-term follow-up and comparison of techniques. Br J PlastSurg 31:107-116.
- Demiri E, Foroglou P, Dionyssiou D, Antoniou A, Kakas P, et al. (2006)Our experience with the lateral supramalleolar island flap for reconstruction of the distal leg and foot: a review of 20 cases. Scand J PlastReconstrSurg Hand Surg 40:106-110.
- Voche P, Merle M, Stussi JD (2005) The lateral supramalleolar flap: experience with 41 flaps. Ann PlastSurg 54:49-54.
- Almeida MF, da Costa PR, Okawa RY (2002) Reverse-flow island sural flap. PlastReconstrSurg 109:583-591.
- Kneser U, Bach AD, Polykandriotis E, Kopp J, Horch RE (2005) Delayed reverse sural flap for staged reconstruction of the foot and lower leg. PlastReconstrSurg 116:1910-1917.
- Donski PK, Fogdestam I (1983) Distally based fasciocutaneous flap from the sural region: a preliminary report. Scand J PlastReconstrSurg17:191-196.
- ZAYED EF (2011) LateralSupramalleolar Flap for Reconstruction of the Distal Leg and Foot, Clinical Experience with 25 Cases. JPlastReconstrSurg 35: 279-286.
- Tan O, Atik B, Bekerecioglu M (2005) Supercharged reverse-flow sural flap: a new modification increasing the reliability of the flap. Microsurgery 25:36-43.
- BhutaniS, Vishwanath G (2012) Hyperbaric oxygen and wound healing.Indian J PlastSurg 45: 316–324.
- Kemmer A (2006) Crush injury and other traumatic ischemia. In: Mathieu D ed. Handbook on hyperbaric medicine. Netherlands: Springer, pp. 311–312.
- Ulkür E, Karagoz H, Ergun O, Celikoz B, Yildiz S, et al. (2007) The Effect of Hyperbaric Oxygen Therapy on the Delay Procedure. PlastReconstr Surg. 119:86-94.
- Greensmith E (2004) Hyperbaric Oxygen Therapy in Extremity Trauma. J Am AcadOrthopSurg12:376-384.
- May JW, Rohrich RJ (1986) Foot reconstruction using free microvascular muscle flaps with skin grafts. Clin PlastSurg13:681-689.
Citation: Mukundan PK, AmbookanPV, Karangath RR (2019) Proximal Foot and Sole Soft Tissue Defect Reconstruction with Distally Based Pedicle Flaps: An Approach with Hyperbaric Oxygen Therapy as a Tool. J Emerg Med Trauma Surg Care 6: 030.
Copyright: © 2019 Pradeoth Korambayil Mukundan, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

