
The Laryngeal Mask Was Useful in a Patient with Cervical Spondylosis Placed in a Cervical Collar during Electroconvulsive Therapy
*Corresponding Author(s):
Yuji KadoiOperating Room, Gunma University Hospital, Maebashi, Japan
Tel:+81 272208454,
Fax:+81 272208473
Email:kadoi@gunma-u.ac.jp
Abstract
Introduction: Airway management during ECT (Electroconvulsive Therapy) is a concern in patients with cervical spine disease. We describe a case of airway management using a laryngeal mask and cervical collar during ECT in a patient with cervical spondylosis.
Case description: A 74-year-old man with cervical spondylosis and depression was scheduled for ECT. He had been wearing a cervical collar to minimize exacerbation of paresthesia and numbness prior to surgical repair of the spondylosis. We planned to use a laryngeal mask for airway management during ECT. No mask ventilation was selected before insertion of the laryngeal mask. After providing 100% oxygen, anesthesia was induced. Ventilation was not initiated until muscular relaxation was judged adequate, and then the laryngeal mask was inserted. No change in symptoms of cervical spondylosis was observed after ECT.
Conclusion: In addition to no mask ventilation, a laryngeal mask appeared effective for avoiding deterioration of cervical symptoms.
Keywords
Cervical spondylosis; Electroconvulsive therapy; Laryngeal mask; Mask ventilation
INTRODUCTION
Electroconvulsive Therapy (ECT) lasts only a few minutes, so manual mask ventilation is a standard procedure in clinical practice [1]. However, a laryngeal mask is needed in some cases for airway management, such as in morbidly obese patients or in cases needing adequate hyperventilation during ECT [2-5]. Manual mask ventilation is usually performed using a face mask with a standard circle during ECT. However, manual mask ventilation with a head tilt-chin lift maneuver or jaw thrust maneuver risks further injury to the cervical spinal cord in patients with cervical spine disease [6]. As a result, airway management is of great concern in such patients during ECT. To date, few reports have described airway management in patients with cervical spine disease during ECT [7-9]. We describe a case of airway management during ECT in a patient with cervical spondylosis wearing a cervical collar.
CASE PRESENTATION
ECT was scheduled for a 74-year-old, 56-kg man with depression. He had complained of paresthesia and numbness in the upper limbs, and muscle weakness in both upper and lower limbs. Symptoms of paresthesia and numbness of the upper limbs were aggravated on cervical flexion and extension. Magnetic Resonance Imaging (MRI) showed severe stenosis of the cervical spine between the C5 and C6 vertebrae (Figure 1). Cervical spondylosis was diagnosed by orthopedic surgeons. A cervical collar was being worn to avoid exacerbation of paresthesia and numbness. The cervical spondylosis required surgical repair, but symptoms of depression were markedly worsening, so ECT was given priority.
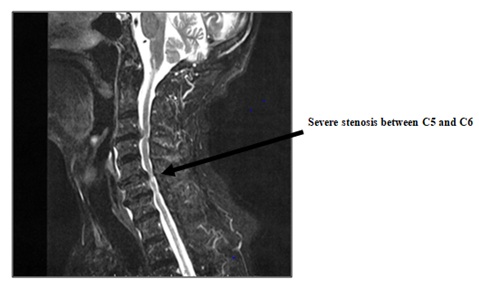 Figure 1: MRI indicates severe stenosis in the cervical spine between vertebrae C5 and C6.
Figure 1: MRI indicates severe stenosis in the cervical spine between vertebrae C5 and C6.
Head tilt position and cervical flexion and extension were prohibited by the orthopedic surgeons to avoid deterioration of paresthesia and numbness of the upper limbs. ECT with the cervical collar in place was therefore planned to protect against further cervical spine cord injury.
Oral olanzapine at 10 mg was continued on the day of ECT. No premedication was administered. No abnormalities were apparent on Electrocardiogram (ECG), plain chest X-ray or laboratory analyses. We planned the airway management to use a laryngeal mask (i-gel®; Intersurgical, Nihon Medical Co. Osaka) for airway management during ECT, with no manual mask ventilation before insertion of the laryngeal mask. In addition to the usual pulse oximeter, Oxygen Reserve Index (ORi) was monitored using a Radical-7R pulse oximeter (Masimo Co., Irvine, CA) to ensure the oxygenation state remained normal during no manual mask ventilation [10]. A tight-fitting mask was used for 5 min to provide 100% oxygen at 6 L/min to achieve a maximal pre-oxygenation state, as previously reported [11]. After 5 min of 100% oxygen, anesthesia was induced using propofol at 1.0 mg/kg, and then suxamethonium was administered at 1.2 mg/kg body weight. After inducing anesthesia, 100% oxygen was continued at 6 L through a tight-fitting mask without ventilation until muscular relaxation was judged as adequate, based on when all muscle fasciculation was finished down to the toes. Adequate muscular relaxation was achieved in about 90-100 s (apneic period; time between induction of anesthesia and time muscular relaxation was judged as adequate: mean apnea time was 94 ± 8 s from eight ECT procedures) (Figure 2). The laryngeal mask was then inserted (Figure 3). After insertion of the i-gel® laryngeal mask, hyperventilation was achieved by manual ventilation with 100% oxygen for 10-15 s. Bilateral electrodes were then placed and the electrical stimulus for ECT was delivered using a Tymatoron system IV® (Somatics; LLC, Lake Buff, IL) via bifrontal-temporal electrodes. After seizure termination, spontaneous breathing resumed within several minutes. After emergence from anesthesia, the laryngeal mask was removed.
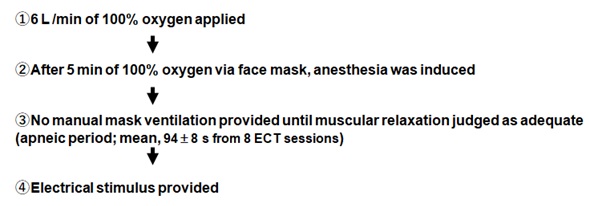 Figure 2: Schematic of the ECT procedure.
Figure 2: Schematic of the ECT procedure.
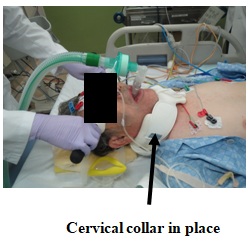 Figure 3: ECT is performed with the cervical collar in place.
Figure 3: ECT is performed with the cervical collar in place.
Eight sessions of ECT were performed. Airway management in all ECT procedures was performed using the same strategy. No hypoxemic state was observed during the 8 sessions of ECT (Table 1). Symptoms of depression were dramatically improved after the 8 sessions of ECT, to the point where no further ECT was required. No significant changes in symptoms of paresthesia and numbness in the upper limbs were observed.
|
Time point |
SpO2 (%) |
ORi |
mBP (mmHg) |
HR (beats/min) |
|
Before preoxygenation |
92 |
0 |
88 ± 2 |
91±3 |
|
1 min after preoxygenation |
97 |
0.07 ± 0.07 |
87 ± 4 |
91 ± 2 |
|
2 min after preoxygenation |
99 |
0.26 ± 0.02 |
88 ± 4 |
90 ± 3 |
|
5 min after preoxygenation |
99 |
0.29 ± 0.03 |
89 ± 3 |
91 ± 2 |
|
Pre-electrical stimulation |
99 |
0.27 ± 0.07 |
81 ± 3 |
92 ± 2 |
|
1 min after seizure termination |
99 |
0.28 ± 0.05 |
109 ± 8 |
112 ± 7 |
|
At resumption of spontaneous breathing |
99 |
0.29 ± 0.06 |
91 ± 3 |
98 ± 4 |
Table 1: Average data for hemodynamic and oxygenation state during eight sessions of ECT.
Data are expressed as mean ± SD.
ORi: Oxygen Reserve Index; mBP: Mean Blood Pressure; HR: Heart Rate.
DISCUSSION
The current case shows that airway management using a laryngeal mask during ECT can effectively protect against further cervical spinal cord injury in patients with cervical spondylosis placed in a cervical collar. Airway management during ECT is of great concern for patients with cervical spine disease. Manual mask ventilation with a face mask is the standard during ECT, because each session lasts only a few minutes [1]. However, in our case, manual mask ventilation posed a danger for deterioration of paresthesia and numbness in the upper limbs. Hauswald et al., examined the effects of various types of airway management on cervical spine movement, and showed that ventilation by mask caused more displacement of the cervical spine than other procedures [12]. Prasarn, et al., compared the effects of head tilt-chin lift and jaw thrust maneuvers on movement and angulation of the spine in the setting of unstable upper cervical spine injury, and found that the jaw thrust maneuver resulted in less motion as compared with the head tilt-chin lift maneuver [6]. They recommended use of the jaw thrust maneuver to improve airway patency in trauma patients with suspected cervical spine injury. Therefore, first, we considered that a jaw thrust maneuver alone with manual mask ventilation was not overly risky in terms of further injury to the cervical spinal cord. However, the cervical collar caused a relative disturbance in manual mask ventilation with a jaw thrust maneuver, and we found that we could not achieve adequate airway patency.
In some cases, a laryngeal mask is useful for achieving adequate hyperventilation or maintaining airway patency in morbidly obese patients during ECT [2-5]. A laryngeal mask is not always used for airway management during ECT, but may be effective to keep the airway patent in patients with cervical spine disease. In addition, hyperventilation is needed for adequate seizure duration after short-time apnea duration; insertion of laryngeal mask was needed even though oxygenation state was preserved in this case [1].
A small number of reports have described airway management in patients with cervical spine disease during ECT [7-9]. Musgrave, et al., reported the safety of ECT in a patient with recent cervical fusion [8]. However, cervical flexion and extension were not disturbed in their case, so manual mask ventilation was easily achieved. Our case is the first to report airway management for a patient with cervical spondylosis in a cervical collar during ECT.
Several other options for airway management were available in this case. Because of the severity of the depressive condition, collaboration with the patient was not considered feasible for the option of awake tracheal intubation in the first and second sessions of ECT. Second, standard tracheal intubation using a video-assisted laryngoscope is most effective to maintain airway patency. However, manual mask ventilation represented a danger to this patient, so the apneic period would be present even in tracheal intubation management. This apneic period would be the same as with use of the laryngeal mask. A review by Li, et al., found that compared with tracheal intubation, a laryngeal mask significantly reduced the incidence of postoperative cough, pulmonary rales and infection [13]. We therefore selected the laryngeal mask for airway management in this case. Finally, a recent report described the use of a High-Flow Nasal Cannula (HFNC) as an alternative to mask ventilation during ECT. HFNC might have been useful in this case [14].
We did not use a muscle relaxation monitor in this case due to technical problems. Such devices should be used where possible to ensure adequate muscular relaxation. Our previous study showed that the average onset time for a 1.0 mg/kg dose of suxamethonium during ECT was 90 ± 17 s (range, 58-124 s). We speculated that the apneic period would have been within 2 min in this case, so 5 min of preoxygenation before induction of anesthesia would have been sufficient to avoid hypoxemia (SpO2 < 90%) during a 2 min apneic period.
Szmuk, et al., reported that monitoring OR i can detect a hypoxemic state (SpO2 <90%) earlier than the standard pulse oximetry. ORi by Radical-7® was used to detect hypoxemia early during the apneic period when no manual mask ventilation was being performed, and the preoxygenation time (5 min in this case) was good enough to avoid hypoxemia (SpO2 <90%) [10]. A review by Nimmagadda, et al., found that preoxygenation > 5-6 min could prevent SpO2 < 90% during a 5 min apneic state among non-obese patients [11].
CONCLUSION
We have reported a case of airway management using laryngeal mask during ECT in a patient in a cervical collar for cervical spondylosis. In addition to avoiding manual mask ventilation, use of a laryngeal mask might be effective to further protect the cervical spinal cord from injury in such cases.
FUNDING
This study was supported in part by a grant to Dr. Kadoi (no. 19K09345) from the Japanese Ministry of Education, Culture, Sports, Science and Technology.
ACKNOWLEDGEMENT
The authors wish to thank Forte Science Communications KK (Tokyo, Japan) for assistance with manuscript preparation in English.
REFERENCES
- Kadoi Y, Saito S (2009) Anesthetic considerations for electroconvulsive therapy -especially hemodynamic and respiratory management. Curr Psychiatry Rev 5: 276-286.
- Koyama Y, Nishioka H, Ibaraki T, Ozawa A, Kamoshida N, et al. (2017) Successful Anesthetic Management of Morbidly Obese Patients During Electroconvulsive Therapy With the ProSeal Laryngeal Mask Airway in a Head-up Position: A Report of 2 Cases. J ECT 33: 30-31.
- Buj-Alvarez I, Pifarré J, Marco G, de Sousa-Duso M, Martínez M, et al. (2016) Can the laryngeal mask play a role in electroconvulsive treatment? A pilot study. Rev Psiquiatr Salud Ment 9: 203-209.
- Bryson EO, Hermida AP, Kellner CH (2017) Should the laryngeal mask airway play a role in electroconvulsive therapy? Rev Psiquiatr Salud Ment 10: 126-127.
- Chow TK (2012) Titration of electroconvulsive therapy: the use of rocuronium and sugammadex with adjunctive laryngeal mask. Br J Anaesth 108: 882-883.
- Prasarn ML, Horodyski M, Scott NE, Konopka G, Conrad B, et al. (2014) Motion generated in the unstable upper cervical spine during head tilt-chin lift and jaw thrust maneuvers. Spine J 14: 609-614.
- Kellner CH, Tolhurst JE, Burns CM (1991) ECT in the Presence of Severe Cervical Spine Disease. Convuls Ther 7: 52-55.
- Musgrave N, Madden A, Mehta M, Singh E, Reeves K (2020) The Safety of Electroconvulsive Therapy in Cervical Fusion. J ECT 36: 43:44.
- Briggs MC, Popeo DM, Pasculli RM, Bryson EO, Kellner CH (2012) Safe resumption of electroconvulsive therapy (ECT) after vertebroplasty. Int J Geriatr Psychiatry 27: 984-985.
- Szmuk P, Steiner JW, Olomu PN, Ploski RP, Sessler DI, et al. (2016) Oxygen Reserve Index: A Novel Noninvasive Measure of Oxygen Reserve--A Pilot Study. Anesthesiology 124: 779-784.
- Nimmagadda U, Salem MR, Crystal GJ (2017) Preoxygenation: Physiologic Basis, Benefits, and Potential Risks. Anesth Analg 124:507-517.
- Hauswald M, Sklar DP, Tandberg D, Garcia JF (1991) Cervical spine movement during airway management: cinefluoroscopic appraisal in human cadavers. Am J Emerg Med 9: 535-538.
- Li L, Zhang Z, Yao Z, Wang H, Wang H, An H, et al. (2019) The impact of laryngeal mask versus other airways on perioperative respiratory adverse events in children: A systematic review and meta-analysis of randomized controlled trials. Int J Surg 64: 40-48.
- Zhu Y, Kang Y, Wei J, Hu J, Wang C, et al. (2019) Effect of high-flow nasal cannula versus conventional facemask ventilation for patients undergoing modified electroconvulsive therapy: A randomised controlled, noninferiority trial. Eur J Anaesthesiol 36: 309-310.
- Matsumoto N, Tomioka A, Sato T, Kawasaki M, Kadoi Y, et al. (2009) Relationship between cardiac output and onset of succinylcholine chloride action in electroconvulsive therapy patients. J ECT. 25: 246-249.
Citation: Kadoi Y, Mieda R, Nakasone C, Ota J, Saito S, Sameshima T (2020) The Laryngeal Mask Was Useful in a Patient with Cervical Spondylosis Placed in a Cervical Collar during Electroconvulsive Therapy. J Anesth Clin Care 7: 58.
Copyright: © 2020 Rie Mieda, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

