
Wide Spread Arterial and Venous Thrombosis in a Case of Hyperglycemic Hyperosmolar State (HHS)
*Corresponding Author(s):
Ganaw ADepartment Of Anesthesia, ICU And Perioperative Medicine, Hamad Medical Corporation, Weil Cornell Medical College, Doha, Qatar
Tel:+ 97433605110,
Email:AGanaw@hamad.qa
Abstract
A case is presented with a patient in a Hyperglycemic Crisis (HC), complicated by widespread thrombo ischemia including the left upper and lower limb, and the aortic arch. Extreme hyperglycemia and dehydration added to the pro-thrombotic state of diabetes and resulted in lower limb ischemia with ultimate limb loss. Current guidelines provide for thrombo-prophylaxis against Deep Venous Thrombosis (DVT) in HHS. Further development of the guidelines is needed to cover the risk of an arterial thrombosis as well.
Keywords
INTRODUCTION
Diabetes mellitus is regarded as a pro-thrombotic state [1]. Extreme hyperglycemia and dehydration in the Hyperglycemic Hyperosmolar State (HHS), a subtype of Hyperglycemic Crisis (HC), add to the risk for thrombo-ischemic events [2]. Lower limb ischemia and occlusion of the femoral arteries in HHS is a distinct association, but its development may be hard to recognize due to its infrequent occurrence in daily practice [3,4]. Prompt recognition is important, since the window of opportunity to prevent irreversible damage is narrow. For teaching purposes, the following case is reported.
CASE PRESENTATION
| Characterstics | Clinical Parameters | Normal Range |
| Age | 50 years | |
| Gender | female | |
| BMI | 31.1 Kg/m² | |
| Heart rate | 126 beats/min | |
| Blood pressure | 93/40 mm Hg. | |
| Temperature | 38°C | |
| Resp. rate | 28 breaths/min | normal range |
| Blood sugar | 84.4 mmol/L | 3.3-5.5 mmol/L |
| Calculated osmolarity | 348.4 mOsm/Kg | 275-295 mOsm/Kg |
| Sodium | 132 mmol/L | 135-145 mmo/L |
| Potassium | 6.1 mmol/L | 3.5-5.5mmol/L |
| Urea | 18 mmol/L | 2.5-7.1 mmol/L |
| Creatinine | 312 µmol/L | 50-98 µmol/L |
| Leucocytes | 23X109/L | 4-10X109 |
| Platelets | 425 x10³ | 150-400x10³ |
| Serum Lipase | 1400 IU/L | 13-60 IU/L |
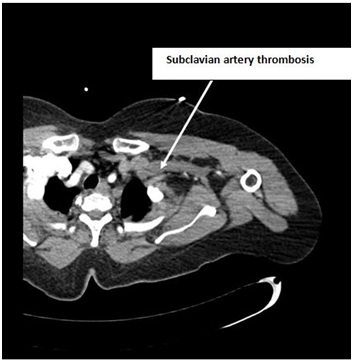
Figure 1: CT angiogram is showing subclavian artery thrombosis.
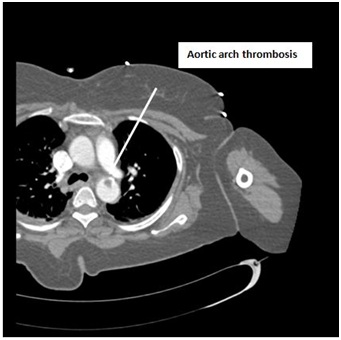
Figure 2: CT Angiogram is showing Aortic arch thrombosis.

Figure 3: CT angiogram is showing Aortic arch thrombosis.
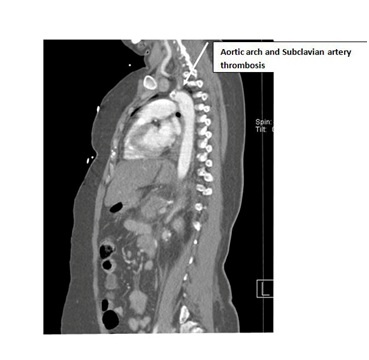
Figure 4: CT angiogram is showing Aortic arch and Subclavian artery thrombosis.
| Item (Normal range) | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 |
| Platelets (150-400x10.3/µL) | 415 | 226 | 99 | 32 | 19 | 17 | 48 | 106 |
| INR (1-1.1) | 1.1 | 1.2 | 1.3 | 2.9 | 3 | 2.4 | 1.7 | |
| D-Dimer (less than 0.46 mg/L) | 4.48 | 23.26 | 35.2 | |||||
| Fibrinogen (1.8-3.5 g/L) | 2.6 | 2.3 | 2.2 |
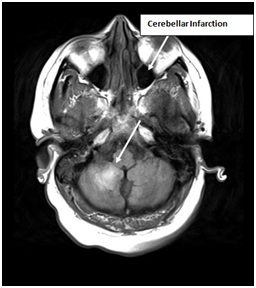
Figure 5: MRI is showing cerebellar infarction.
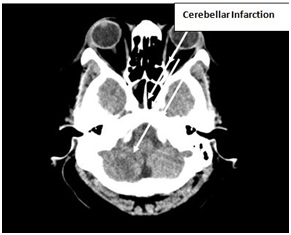
Figure 6: CT scan is showing cerebellar infarction.
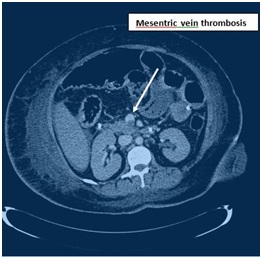
Figure 7: CT Angiogram is showing mesenteric vein thrombosis.
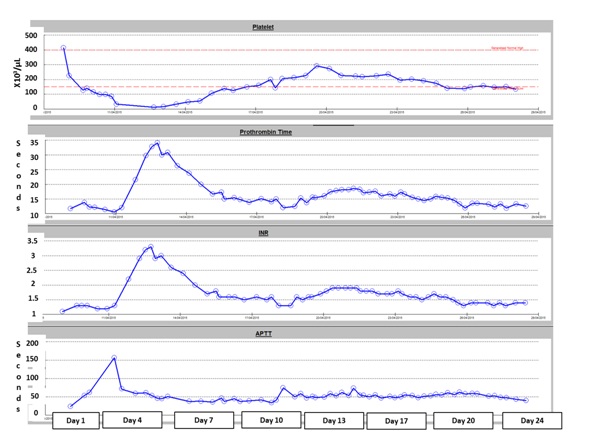
Figure 8: Coagulation during stay in intensive care unit.
DISCUSSION
REFERENCES
- Pomero F, Di Minno MN, Fenoglio L, Gianni M, Ageno W, et al. (2015) Is diabetes a hypercoagulable state? A critical appraisal. Acta Diabetol 52: 1007-1016.
- Lemkes BA, Hermanides J, Devries JH, Holleman F, Meijers JC, et al. (2010) Hyperglycemia: a prothrombotic factor?. J Thromb Haemost 8: 1663-1669.
- Megarbane B, Marsanne C, Meas T, Medeau V, Guillausseau PJ, et al. (2007) Acute lower limb ischemia is a frequent complication of severe diabetic hyperosmolarity. Diabetes Metab 33: 148-152.
- Milano A, Tadevosyan A, Hart R, Luizza A, Eberhardt M (2016) An uncommon complication of hyperosmolar hyperglycemic state: bilateral above knee amputations. Am J Emerg Med 34: 341.
- Fayfman M, Pasquel FJ, Umpierrez GE (2017 ) Management of Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Med Clin North Am 101: 587-606.
- Li MF, Ren Y, Zhao CC, Zhang R, Li LX, et al. (2014) Prevalence and clinical characteristics of lower limb atherosclerotic lesions in newly diagnosed patients with ketosis-onset diabetes: a cross-sectional study. Diabetol Metab Syndr 3: 6-71.
- Shah B, Rockman CB, Guo Y, Chesner J, Schwartzbard AZ, et al. (2014) Diabetes and vascular disease in different arterial territories. Diabetes Care. 37: 1636-1642.
- Verma H, Meda N, Vora S, George RK, Tripathi RK (2014) Contemporary management of symptomatic primary aortic mural thrombus. J Vasc Surg 60: 1524-1534.
- Caron F, Anand SS (2017) Antithrombotic therapy in aortic diseases: A narrative review. Vasc Med. 22: 57-65.
- Scott AR; Joint British Diabetes Societies (JBDS) for Inpatient Care; JBDS hyperosmolar hyperglycaemic guidelines group 2015) Management of hyperosmolar hyperglycaemic state in adults with diabetes. Diabet Med 32: 714-724.
- Butt T, Gottsater A, Apelqvist J, Engstrom G, Acosta S (2017) Outcome of intra-arterial thrombolysis in patients with diabetes and acute lower limb ischemia: a propensity score adjusted analysis. J Thromb Thrombolysis 44: 475-480.
- Kruger T, Liske B, Ziemer S, Lindemann S, Ziemer G (2011) Thrombolysis to treat thrombi of the aortic arch. Clin Appl Thromb Hemost 17: 340-345.
Citation: Ganaw A, Shaikh N, Marcus AE, Soekarman D (2018) Wide Spread Arterial and Venous Thrombosis in a Case of Hyperglycemic Hyperosmolar State (HHS). J Anesth Clin Care. 5: 027.
Copyright: © 2018 Ganaw A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

