
Would the End of COVID-19 Infection as a Chronic Disease?
*Corresponding Author(s):
Kieu C D NguyenAmerican Stem Cell Hospital JSC & Euro Stem Cell, Vietnam
Email:drkieukaren@gmail.com
Abstract
Although highly transmissible due to its highly infectious nature, since a large proportion of cases are asymptomatic or mild, self-awareness which promotes the spread of the disease worldwide. The public health manages against Corona virus should reduce the numbers of people infected with influenza virus to avoid the two viruses infections will be interacted. The successful combination of using antiretroviral therapy and antibiotics in several inflammation in multi organs with supportive therapies in this case report in region Puglia ASL Taranto, PPI 118- emergency department and pneumonia department in Saint Giuseppe Moscati hospital, Taranto - Italy to develop achronic disease care model for “POST-COVID-19 “and taking epidemic preventing action for the winter season 2020 is coming.
Keywords
ASL Taranto; Arterial Blood Gas (ABG); COVID-19, Chronic Disease; SG Moscati Hospital; Sars-CoV-2; 118 Pre-Hospital Medical System-Emergency Department
THE FIRST ADMISSION
In March 16th 2020, an 86 years old Italian man living in Taranto with his wife were found positive to COVID-19 when he was admitted to Department of Emergency 118 , PPI S. G. Moscati hospital in Taranto, Italy . His medical history with diabetes, cardio-vascular disease. Symptoms at the admission time were mild dyspnea, respiratory distress, high fever (39°C), dry cough, general malaise, the ABG analysis showed a pH alkaline 7.52 with a PaO2 low 45 mmHg ( normal range 75-100), low PaCO2 33 mmHg ( normal range 35-100). He experienced a sudden deterioration accompanied by headache, and heavy fatigue.
In 118 Emergency Department, the both tampon throat swab buffers (oral - nasal-pharynx by RT-PCR) and CT - scan were suggestive for positive for SARS -CoV-2 infection . The increased level of C-reactive protein 116 mg /L (normal range 3.5). ESR 86 mm/H (normal range up to 10). Alfa 1 Antitripsina 202 mg/dl (normal at 90-200 ) . Electroforesi Sieroproteica : Low Albumine at 51.4% (normal at 54.70 - 69.66) . High Alfa 1 at 7.4% (normal at 2.63 - 5.0) ; Alfa 2 at the limit high 12.7% (4.87 -12.40) . The symptoms associated with acute respiratory failure was confirmed by X-Ray and lung CT scan positive with bilateral ground glass opacity that showed a significant increase in alveolar capillary permeability and subsequent interstitial edema . It was confirmed pulmonary embolism located with a chronic diffuse bronchopathy with emphysematous configurations. It was observed in the right lung the presence of extensive areas of parenchymal consolidation, irregularly distributed, mainly affecting the lower lobe and the apical and dorsal segments of the upper lobe. There were ground glass opacity areas of the pulmonary parenchyma surrounding the consolidations both apical-dorsal and lower lobe showed interstitial engagements. Circumscribed and consolidated outbreaks, also surrounded by ground glass opacity formations, where observed in the anterior part of the upper lobe of the right lung. In the left lung at the level of lower lobe it was observed a pseudo-nodular consolidation (23 mm) surrounded by ground glass opacities (Figures 1 & 2).
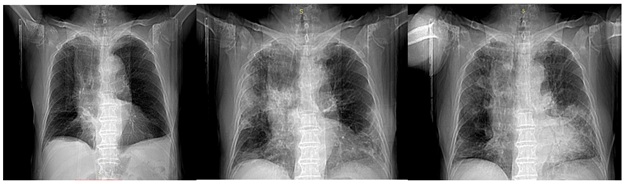
Figure1: X ray Images show the condition of the 86 year old male patient of March, May and June 2020. The images show the typical ground glass opacity which has been considered relevant in characterizing the Sars-CoV-2 invasive patterns. The patient was COVID-19 positive (both swab/RT-PCR and CT-scan).
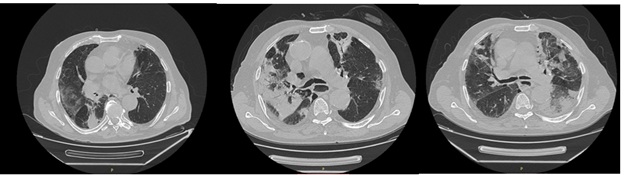 Figure 2: Axial CT-scan images performed in March, May and June 2020 of the 86-year-old man with clinical findings suggestive of COVID-19 infection.
Figure 2: Axial CT-scan images performed in March, May and June 2020 of the 86-year-old man with clinical findings suggestive of COVID-19 infection.
The CBC and laboratory analysis confirmed a general state of deterioration with high level of both inflammation and infectious markers suggestive of a multi-organ deterioration and infectious - inflammatory patterns especially referred to lungs, heart and kidneys. It was observed important high level D-Dimero 3.80 mg/L (normal range up to 0.5 mg/L FEU. Fibrinogen 754 mg/dl (normal range 200-400). High G.neutrofile 89.8% (normal range 35.0-75.0) and low lymphopenia 8.0% (normal range 20.0-55.0). VES 86 mm/h (normal range 1-10). Anti Chlamidia pn IgG 2,3 ( index up to 1.1). Mycoplasma pnIgG 13,7 (index up to 9). Moderate -severe disfuntioned kidney with low level of eGFR Filter Glomerular Stimulate (Eq. CKD-EPI) 32.46 ml/min (normal range over 90). Low level of Albumine 2744 mg/dL (3500-5200) High Creatinine 1.84 mg/dl (normal 0.6-1.3). Urea at 87 8 mg/dl (normal range 10-50). Urine proteuria 50 mg/dl (normal range up 25) and Ph 5.0 (normal 5.5-6.5). Glucose 190 mg/dL (normal adult 74-100). Clo 97 mEq/L (normal 98-108) Osmolalityplasmatic 322 mOsm/lt (normal290-300). Low Lipase 58 U/L (73-393). Significative high NT-pro BNP 354 pg/mL (normal range up to 130). Hb Glicata 6.9 % ( 4.0-6.4). This patient was transferred to pneumonia department and hospitalized with treatment by combined therapy following the S.G. Moscati hospital anti-COVID-19 protocol. This therapy strategy consisted on targeting viral and bacterial infection, associated with anti-thrombolytic drugs in order to arrest the worsening of the disease [1,2].
THE SECOND ADMISSION
In May 11th 2020 this patient was hospitalized for the second time with worse condition as fever 38oC, dyspnea, dry cough, fatigue, exhaustion and respiratory distress with mild hyperventilation [3,4]. The ABG showed a pH of 7.373 (normal range 7.35-7.45) with a pO2 at 59.4 l mmHg (normal range 75-100), high PaCO2 48.3 mmHg (normal range 35- 45).
His blood count (CBC) performed at the second time showed the degenerative process. The severe disfuntioned kidney was confirmed by low level of eGFR Filter Glomerular Stimulate (Eq. CKD-EPI) 29.34 ml/min (normal range over 90). Creatinine at 2.0 mg/dl (normal range 0.6-1.83). High level of Urea at 63 mg/dl (normal range 10-50). Glucose 249mg/dL (normal adult 74-100). High level of inflammatory features such as low level of 25OH-vitaminD 10.7 ng/ml( normal range 50-100) and severe high level of Troponine T hs Alta sensib 65.08 ng/L (normal range 14); high Interleukin 6 at 56.8 pg/mL ( normal range under 7); high D-Dimer 46.84 mg/L (normal range 0.5 ); high white blood cell total count (WBC) at 13.17 of 10^3/mm3 (normal range 3.50-10.00) revealing an important disparity in neutrophils-lymphocyte; low Hemoglobin 10.8 g/dL (12.0-18.0) ; low Hematocrit 32.4% (36.0 -54.0); low Lymphopenia 11.4% (normal range 20.0 -55.0 ); high G.neutrophopenia 8.87 of 10^3/ùL ( normal range 1.8-7.5), high Eosinophilia 12.5% ( normal range up to 7%) and high level of Fibrinogen 722 mg/dl (normal range 200 - 400) . High C Reactive Protein-CRP 166 mg/L (normal range 3.5). High VES/ESR 117 mm/H (normal range 1-10).
The CT scan revealed a worsening of lung condition [5]. The image showed the presence of multiple artifacts concomitant to incorrect respiratory apnea with a general worsening of lung functionality compared to the previous evaluation.
THE THIRD ADMISSION
In June 25, 2020 this patient was hospitalized third time in 118 Emergency Department with high fever (39°C), dyspnoea and severe respiratoty distress [3,4]. The ABG analysis showed a pH 7.423 (normal range 7.35-7.45) with pO2 38.5 mmHg (normal range 75-100) and PaCO2 at 51.7 (normal range 35-45).
The blood count (CBC) and laboratory analysis showed a progressive deteriorating with multi-organ involvement. Chronic severe kidney dysfunction remained substantially unvaried with low level of eGFR Filter Glomerular Stimulate (Eq. CKD-EPI) 33.55ml/ min( normal range over 90); Creatinine at 1.79 mg/dl (normal range 0.6-1.3 ); high level of Urea 63 mg/dl (normal range 10-50); low Creatine Phospho-kinase (CPK) 15 U/L (normal range 39-308); Glucose 176 mg/dL (normal adult 74-100). High level of inflammatory state characterized by low level of 25OH-vitaminD 9.1 ng/ml ( normal range 50-100) ; high C Realtiva Proteinae-CRP 146.0 mg/L ( normal range 3.5); High ESR/VES 126 mm/H ( normal range 1-10); high D-Dimer at 60.80 mg/L (normal range 0.5 mg/L FEU) ; high level of Fibrinogen 694 mg/dl (normal range 200 - 400); severe high level of Troponine T hs Alta sensib 51.340 ng/L (normal range 14); low level of 25OH-vitaminD 9.1 ng/ml ( normal range 50-100) ; high Interleukin 6 at 61.9 pg/mL (normal range under 7). The CBC revealed a mild anemia profile confirmed by low level of Red Blood Cells (RBC) at 3.23 of 10^6/mm3 ( normal range 4.00-6.00); low Hemoglobin 9.8 g/dL (normal 12.0-18.0) ; low level of Hematocrit 30.1% (normal range 36.0% -64.0%) . In addition, the total white blood cell total count (WBC) was elevated at 15.79 of 10^3/mm3 (normal range 3.50-10.00) and revealing an important disparity in neutrophils-lymphocy; low Linfociti 13.4% (normal rang 20.0% -55.0%); high G.neutrofili 10.36 of 10^3/ùL (normal range 1.8-7.5); Eosinophilia 10.6% (normal range up to 7%).
The CT scan confirmed a worsening of lung condition with multiple respiratory artifacts from incorrect respiratory apnea and multiple bilateral parenchymal consolidations with contextual air Broncho gram images next to adjacent areas with ground glass opacities, the major consolidations were reported at the RSL, LIL levels and lingual [5].
MEDICATION
The treatment was based on the use of azithromycin, ceftriaxone, ketoprofen, enoxaparin sodium, methilprednisone, acetylcysteine, hydroxychloroquine, clarithromycine and high flow oxygen therapy and high restrictive fluid management.
CONCLUSION
With the promptly admission into 118 Emergency Department in Saint Giuseppe Moscati hospital, Taranto- Italy, he recovered after six weeks with other ten patients.
DECLARATION OF INTERESTS
The authors declare no conflict of interests in this case report.
REFERENCES
- Shi H, Han X, Jiang N, Cao Y, Alwalid O, et al. (2020) Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 20: 425-434.
- Wang Y, Dong C, Hu Y, Li C, Ren Q, et al. (2020) Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology 296(2): 55-64.
- Wu X, Dong D, Ma D (2016) Thin-section computed tomography manifestations during convalescence and long-term follow-up of patients with severe acute respiratory syndrome (SARS). Med SciMonit 22: 2793-2799.
- Kruser JM, Prescott HC (2016) Dysphagia after Acute Respiratory Distress Syndrome: Another Lasting Legacy of Critical Illness. Ann Am Thorac Soc 14: 307-308.
- Inui S, Fujikawa A, Jitsu M, Kunishima N, Watanabe S, et al. (2020) Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19). Radiol Cardiothorac Imaging 2: 200110.
Citation: Balzanelli MG, Distratis P, Lazzaro R, Cefalo A, D'angela G, et al. (2020) Would the End of COVID-19 Infection as a Chronic Disease? J Stem Cell Res Dev Ther 6: 057.
Copyright: © 2020 Mario G Balzanelli, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

