
A Lady with Unilateral Painful Orbital Swelling- Euthyroid Graves Ophthalmopathy
*Corresponding Author(s):
Mohammad Moin ShahidDepartment Of Endocrinology, Ad-din Women’s Medical College, Mogbazar, Dhaka, Bangladesh
Tel:+880 1817028202 ,
Email:dr.ms952@gmail.com
Introduction
Ophthalmopathy is one of the cardinal features of Graves ’ disease (GD) [1]. It is a condition where thyroid auto-antibodies react against thyroid gland, extraocular muscles, retro-orbital tissues like orbital fat, lacrimal glands resulting in orbitopathy - lid lag, lid retraction, chemosis, exophthalmos, extra-ocular muscle palsy and even blindness [2]. Interesting thing about thyroid associated ophthalmopathy is, to develop this condition patient does not need to be in hyperthyroid status - it can develop even in hypothyroid and euthyroid status of the patients [2,3]. Its’ peak incidence is in the twenties and thirties, but it can occur at any age, although it is uncommon before puberty. It is more common in women than men with a ratio over 5:1 [3,4]. Men are usually affected in the later stage of life and the presentations may be more severe.
Case Report
24 years unmarried, non-smoker old lady came to outpatient department of ophthalmology because of painful unilateral proptosis, for 4 months in her right eye. Her protrusion of right eye was gradually increasing and there was a continuous localized dull aching pain in her right eye which increased with the movement of eyeball but did not subside completely after taking rest and analgesics. She had no compliant regarding her left eye. Her previous personal and family history was negative for thyroid disorders. There was no preceding history of defective vision or blackouts or transient loss of vision or defective color perception. There was no history of neck swelling, weakness, palpitation, excessive sweating, weight loss or tremor. She denied of taking antithyroid drugs, thyroid surgery or radio-iodine ablation of thyroid gland.
On ocular examination, her visual acuity was not compromised (6/6 in both eyes), Hirschberg reflex was central in both eyes with unilateral axial proptosis of right eye of 3mm measured by Hertel Exophthalmometer. Dalrymple sign (lid retraction), Von Graefes’ sign (lid lag on down gaze), Mobius’ sign (convergence deficiency) and Kochers’ sign were positive in her right eye. Ocular motility was full in all cardinal position of gazes and there were no complaints of diplopia. The patient received 5/7 in CAS (Clinical Activity Score) due to her orbital pain, gaze evoked ocular pain, eyelid edema, conjunctival congestion, redness, inflammation of lacrimal caruncle in her right eye. In terms of left eye, she received 0/7 in CAS. Her intraocular pressure was normal in both eyes. Magnetic Resonance Imaging (MRI) of orbits revealed unilateral right sided exophthalmos predominantly caused by the thickening of medial rectus muscle figures 1&2.
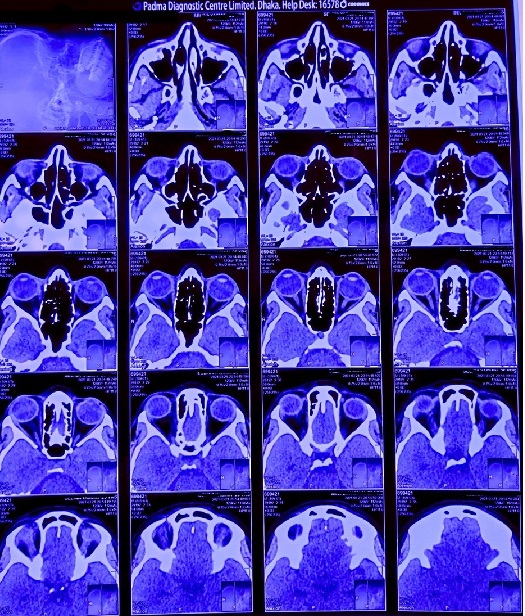 Figure 1: MRI scan 1.
Figure 1: MRI scan 1.
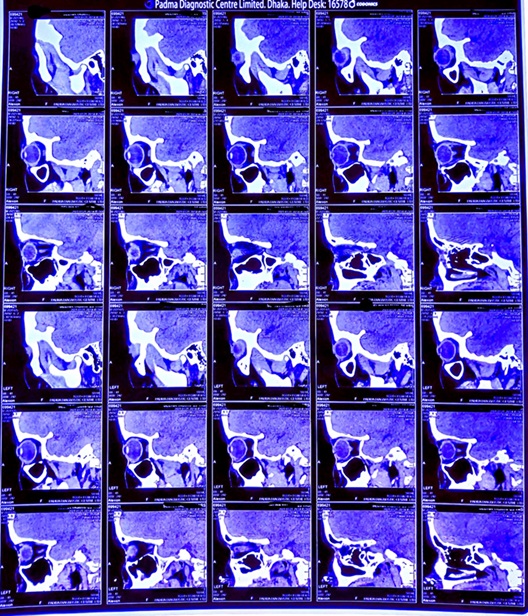 Figure 2: MRI scan 2.
Figure 2: MRI scan 2.
On systemic examination, she had no thyroid gland swelling, pulse was 76 beats/minute. Her Complete Blood Count (CBC) revealed no abnormality. Thyroid function tests showed she was in euthyroid state (F.T3 - 3.22 pg/ml, reference value - 1.45 - 3.48 pg/ml; F.T4 - 0.963 ng/dl, reference value - 0.7 - 2 ng/dl; TSH - 1.08 µIU/ml, reference value - 0.350 - 5.50 µIU/ml). CT scan of orbit showed abnormality. But her Thyroid stimulating hormone receptor antibody (TRab) level was in favor of GD (TRab - 2.33 Units/L; reference value - negative ≤1 Units/L, borderline ? 1 – 1.5 Units/L, positive ? 1.5 Units/L). Since TRab is highly specific for GD, she was diagnosed as a case of Euthyroid Graves’ Ophthalmopathy.
She was prescribed lubricants such as carboxy-methylcellulose 1% eye drop at day time and ointment at night along with topical NSAIDS with a plan to start systemic corticosteroid (Prednisolone) if her condition does not improve. She came for follow up visit after one month. Her proptosis regressed significantly and pain disappeared. During her following visit after 3 months her eye swelling was found completely gone and she has been without any medication since then.
Discussion
Thyroid associated ophthalmopathy is an organ specific auto immune process resulting from a complex interplay of genetic (e.g., HLA) and environmental factors. Patient’s susceptibility may be determined by the genetic factors but its course is influenced by the environment [5]. GO development usually a slow process but can develop within weeks [3].
In patients with GD, thyroid autoantibodies (circulating T cells directed against certain antigens on thyroid follicular cells) detects same antigenic epitopes that are shared by preadipocytes and fibroblasts tissues in the orbital space and extraocular muscles [6,7]. Adhesion molecules like ICAM-1, VCAM-1, CD4 helps in recruitment of T cells and activation of lymphocytes. Facilitating interactions between immunocompetent cells, connective tissue cells and extracellular matrix components, adhesion molecules take active participation in various inflammatory processes, many of which result in amplification of the cellular immune process in active GO [5]. Increased level of thyroid auto antibodies (e.g. TRab) stimulates orbital tissue differentiation either directly or through cytokines and chemokines (e.g. oxygen free radicals). Inflamed cells in orbit release cytokines, chemokines and various growth factors (e.g. fibroblast growth factor) which act upon orbital preadipocytes stimulating adipogenesis, fibroblast proliferation, glycosaminoglycan synthesis, and the expression of immunomodulatory molecules [5-8].
According to Bahn RS, et.al. more than 90% of the GO cases are associated with hyperthyroidism [9]. Patients with euthyroid Graves' disease typically have high levels of both stimulating and blocking TSH receptor antibodies (TRAb) (Figure 3). Though these antibodies cancel each other’s effect but they are both capable of eliciting an immune response in orbital tissue resulting in development of ophthalmopathy [9].
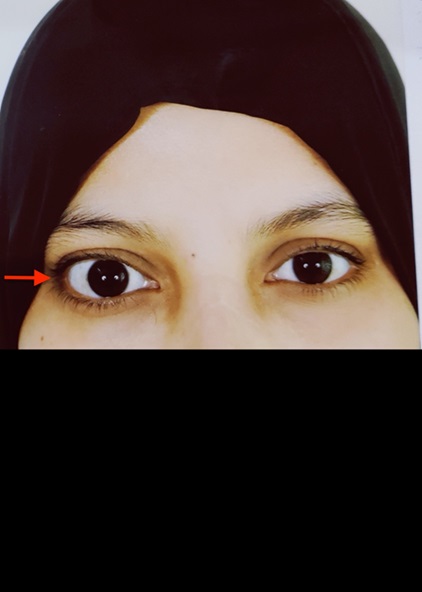 Figure 3: Development of ophthalmopathy.
Figure 3: Development of ophthalmopathy.
Euthyroid GO is a self-limiting condition which may last from months to years. It is usually consisting of two phases - acute phase which is followed by a resolution phase. Low titer of TRab is associated with milder form of ophthalmopathy and early recovery, which possibly happened in case of this patient, too [10]. Thyroid associated ophthalmopathy in euthyroid state is not a common phenomenon [9,11]. So, there is a very good chance of being misdiagnosed. If properly managed then significant recovery is very common reducing the risk of developing scar tissue. Otherwise, it may warrant surgical decompression [9].
Conclusion
Euthyroid GO is a self-limiting condition yet it can be vision threatening. Proper evaluation and early management must not be neglected in this regard.
References
- Jang SY, Lee SY, Lee EJ, Yoon JS (2012) Clinical features of thyroid-associated ophthalmopathy in clinically euthyroid Korean patients. Eye (Lond) 26:1263-1269.
- Gardner D, Shoback D (2004) Greenspans Basic and Clinical Endocrinology, Ninth Edition. 9th ed. Page no: 198-201.
- Rabbani S, Rashid M, Rehena A, Hossain M. Atypical Presentation of Thyroid Ophthalmopathy - A Case Report. Med Today 25: 50-51.
- Wawhal M, Mogal V, Patil P, Ahire P, Yadav S (2013) Euthyroid Ophthalmopathy: A Rare Case Report and a Brief Review of Literature. International Journal of Science and Research Page no: 529-531.
- Heufelder AE, Joba W (2000) Thyroid-associated eye disease. Strabismus 8: 101-111.
- Bahn RS (2003) Pathophysiology of Graves’ Ophthalmopathy: The Cycle of Disease. J Clin Endocrinol Metab 88: 1939-1946.
- Garrity JA, Bahn RS (2006) Pathogenesis of Graves Ophthalmopathy: Implications for Prediction, Prevention, and Treatment. Am J Ophthalmol 142: 147.
- Shen J, Li Z, Li W, Ge Y, Xie M, et al. (2015) Th1, Th2, and Th17 cytokine involvement in thyroid associated ophthalmopathy. Dis Markers 15:609593.
- Wawhal M, Mogal V, Patil P, Ahire P, Yadav S (2013) Euthyroid Ophthalmopathy: A Rare Case Report and a Brief Review of Literature. International Journal of Science and Research.
- Eckstein AK, Plicht M, Lax H, Neuhäuser M, Mann K, et al. (2006) Thyrotropin receptor autoantibodies are independent risk factors for graves’ ophthalmopathy and help to predict severity and outcome of the disease. Journal of Clinical Endocrinology and Metabolism 91: 3464-3470.
- Mourits Ph, Koornneef L, Wiersinga WM, Prummel MF, Berghout A, et al. (1989) Clinical criteria for the assessment of disease activity in Graves’ ophthalmopathy: a novel approach. Br J Ophthalmol 73: 639-644.
Citation: Shahid MM, Rahat EH (2023) A Lady with Unilateral Painful Orbital Swelling- Euthyroid Graves Ophthalmopathy. J Diabetes Metab Disord 10: 049.
Copyright: © 2023 Mohammad Moin Shahid, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

