
Acetaminophen Poisoning: A Cause of Acute Liver Failure in Pediatrics (Clinical Case)
*Corresponding Author(s):
Pshenisnov Konstantin ViktorovichAssociate Professor Of Anesthesiology, Intensive Care And Emergency Pediatrics, Saint-Petersburg State Pediatric Medical University, Saint-Petersburg, Russian Federation
Abstract
Acetaminophen poisoning is one of the most common and most severe poisonings in pediatrics which should be treated in an intensive care units (ICU) due to life-threatening conditions can emerge.
Aim: Demonstration of the characteristics of the course and measures of intensive therapy in case of severe acetaminophen poisoning.
Patients and methods: The clinical case of enteral acetaminophen poisoning while pain healing in 16-year-old girl in whom liver failure was developed is considered. The main procedures to attain patient’s condition stabilization while in ICU in the shortest way were shown. Algorithm of differential diagnostics of liver lesion by remedies was provided. It can be used in any case of liver failure with unclear genesis. The special attention was paid to the earliest distinguishing and pathogenetic treatment of cerebral edema and multiple failure.
Conclusion: The distinctive feature of this clinical case is a highly severe course of poisoning with development of liver failure and multiple dysfunction which regressed while treatment in ICU with full recovery of our patient.
Keywords
Acetaminophen; Acute Liver Failure; Favorable Outcome; Pediatric; Poisoning
INTRODUCTION
Poisoning is one of the most common causes of the development of a critical condition in children, which are commonly found in young children and adolescents [1]. One of the most frequently and dangerous kind of poisonings in children is an overdose of acetaminophen, which is widely used as an antipyretic and NSAID with a mild analgesic effect [2-6].
There are a big range of publications about positive effects of acetaminophen, but side effects also should be noted, among which are acute liver failure development, methemoglobinemia while prolonged using, increased hemolysis in children’s with glucose-6-phospodehydrogenase deficiency, activation of lipid peroxidation, glutathione disruption and centrilobular necrosis of the hepatic parenchyma [7-9].
Despite many years of effective and relatively safe using of acetaminophen in clinical practice, it should be remembered that the unreasonable and uncontrolled administration of this drug can cause severe liver failure with a high risk of death [10-13].
When using therapeutic doses of paracetamol, it is being bio transformed in the liver into sulfates or glucuronides. These polar compounds are non-toxic and are easily excreted in the urine. There is predominance of the sulfate pathway of biotransformation in children under the age of 9-12 years, and the glucuronide pathway in children older than 12. Furthermore, an increasing in the toxicity of paracetamol was noted in children older than 12. About 4% of the drug is oxidized by cytochrome P-450 and bound to glutathione. With a decreased level or deficiency of glutathione, as well as an overdose of the drug, many oxidized reactive metabolites of paracetamol are produced in the liver, which covalently bind to the macromolecules of the liver and damage its cells, leading to necrosis [12, 13].
Toxic effects develop in the case of taking the drug at a dose of 150 mg/kg and above. A concentration of paracetamol in the blood above 50μg/ml (300μmol/l) is toxic and indicates a severe poisoning with the development of clinical signs of liver failure [12].
Paracetamol activates the production of reactive oxygen species (ROS) that are involved in the monoamine oxidase reactions. As a result of an oxidation and conjugation processes (glucuronidation and sulfation processes), acetiminoquinone (a hepatotoxic metabolite) is produced; the last one provokes methemoglobinemia. Detoxication of acetiminoquinone is performed by a conjugation with glutathione. Transformation glutathione to inactive form through losing cysteine leads to the state that it cannot protect hepatocytes from the necrotic effect of an excess of acetiminoquinone [7, 12, 13].
CLINICAL STUDY
With the aim to demonstrate possible toxic effects of acetaminophen in the case of overdosing, we present a clinical case of liver failure in 16 years old girl which required intensive care and extracorporeal replacement therapy.
In January, 2019 a girl of 16 years old was admitted at Children's Hospital No. 5 named after N.F. Filatov. It was the second day after the onset of symptoms of the disease, and main complaints were abdominal pain, nausea, single vomiting. Body weight=45 kg.
The child was examined by a pediatric surgeon and gynecologist, an ultrasound examination of the abdominal organs, clinical and biochemical blood analysis was performed. Acute surgical pathology was excluded. Urine was dark-yellow, stool was liquid and pale. Viral hepatitis was suspected, pathogenetic and symptomatic treatment was initialized. As there were no signs of viral hepatitis in the blood serum, infectious disease of liver was excluded.
On the second day after admission, a sharp deterioration was noted: consciousness was depressed to the level of stupor, pronounced icteric sclera, a significant increase in the enzymatic activity of alanine and aspartate aminotransferase, concentration of all bilirubin fractions, and the absence of coagulation were noted according to a biochemical blood test (Figure 1-3).
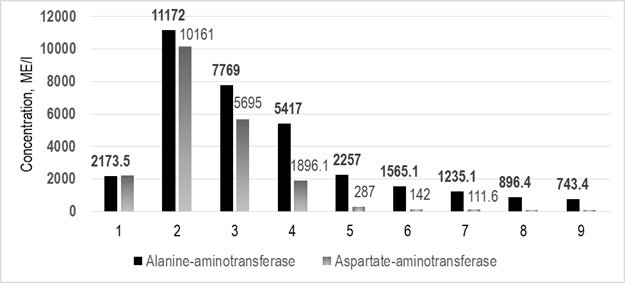
Figure 1: Alanine and aspartate aminotransferase concentration in dynamics.
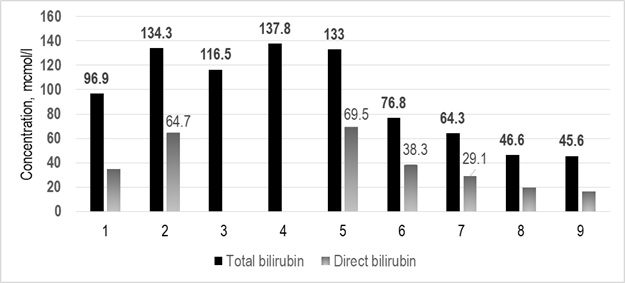
Figure 2: Total and direct bilirubin concentration in dynamics.
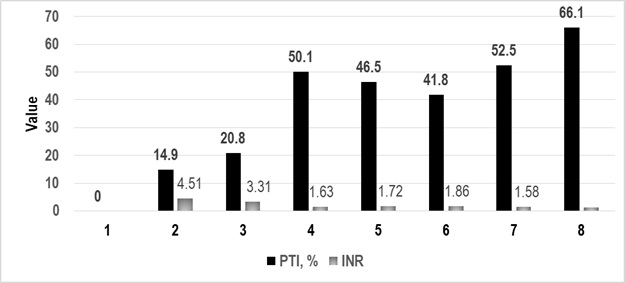
Figure 3: Prothrombin index and international normalized ratio in dynamics.
The child was transferred to the intensive care unit (ICU), where it was found that for three days the girl used fifteen 500 mg acetaminophen tablets to reduce pain during the menstrual cycle. Total dosage of acetaminophen was 167 mg/kg while frequency of taking the medicine was unknown.
Upon admission to ICU, the child’s condition was severe, there are signs of degree III hepatic encephalopathy: sluggish, adynamic, speech was inhibited, answers questions follow a long pause. Acute focal and meningeal symptoms were not revealed. Breathing was spontaneous and adequate, SpO2 = 100%, SpO2 / FiO2 = 500 mm Hg, respiratory rate = 18-22/minute; while lungs auscultation pathological changes were absent. The abdomen was of the normal form, symmetrical, soft, painless, hepatomegaly was revealed (the edge of the liver protruded about 3 cm from the edge of the costal arch). The urine color was dark yellow.
According to the analysis of the gas composition and the acid-base state of venous blood, decompensated acidosis (pH=7,32; pCO2=24 mm Hg; pO2=44 mm Hg; HCO3=12,8 mmol/ l; BE=-11,0 mmol/l), hypoglycemia (glucose=3,2 mmol/l), lactic acidosis (lactate=9,9 mmol / l), hyperkalemia (K+=5.6 mmol/l) were determined. A paracetamol concentration in the blood was not checked due to the lack of labs equipment.
Pathogenetic therapy was started, including infusion in the amount of physiological need, maintenance of «zero» balance of water, correction of metabolic acidosis and hypoglycemia according to European Association for the Study of the Liver (EASL) Clinical Practical Guidelines on the management of acute (fulminant) liver failure [14]. Corticosteroids (prednisolone) were prescribed for cytoprotection at a dose of 5 mg/kg. Correction of severe hypocoagulation was carried out by transfusion of fresh frozen plasma at a dose of 15 ml/kg. Specific therapy with the acetaminophen antidote (N-acetyl-cysteine) in this case was not carried out because of the prolonged using of the toxicant and the late admission of the child to the hospital, although it cannot be seen as the right option.
In the dynamics on the third day in ICU, deterioration of the patient condition was noted due to the progression of neurological disorders, the depression of consciousness to a coma level; hypernatremia (Na+=152 mmol/l) and increased osmolarity of blood plasma were revealed. That was why the decision to conduct extended veno-venous hemodiafiltration and membrane plasma sorption. Ornithine and succinates have been added to the infusion therapy which was carried out in a normal hydration mode.
Stabilization of the state and restoration of clear consciousness were achieved already in a day; persistent regression of the phenomena of acute liver failure and normalization of the coagulation indices were observed. Extended venous-venous hemodiafiltration was being carried out for five days, and on the ninth day after admission to the ICU the child was transferred to the specialized department. The patient was discharged from the hospital with full recovery.
DISCUSSION
One of the distinguishing features of acetaminophen poisoning is the staging of clinical manifestations. As a rule, in the first 24 hours after a single dose of toxic doses of the drug, there are signs of acute gastroenteritis: nausea, vomiting, abdominal pain, diarrhea, and only after a day or more clinical signs of liver damage emerge among which are ictericity of the skin and mucous membranes, increase concentration of liver enzymes, hypocoagulation [12, 13, 15]. The stage of acute acetaminophen poisoning in children is also evidenced by clinical observations of a number of authors [2, 3, 16].
In most cases, the symptoms of this phase of the disease do not progress further and restoration of the function of damaged organs is noted. However, in the case of severe poisoned patients writhe with a progression of liver failure and the development of hepatic encephalopathy with a high risk of manifestation of cerebral edema, which have such precursors as depression of consciousness and hypernatremia. Namely in this stage of the disease in most cases there are signs of kidney damage, the severity of which determines the outcome of the disease [17]. Thus, the key to successful treatment are timely diagnosis and the early implementation of specific pathogenetic therapy. At the same time, it should be noted that the diagnosis of drug damage to the liver is far from simple, which is clearly demonstrated by the presented case. This is especially true for adolescent children, who can independently take various drugs to eliminate the symptoms of the disease or with the aim of suicide. It is why a thorough anamnesis gathering and repeated its clarification are required. The differential diagnostic search algorithm for drug damage to the liver is presented in Figure 4 [18]. An increase in the activity of liver enzymes in the absence of other clinical manifestations of viral hepatitis allows you to immediately suspect the toxic effects of drugs, which is especially important for adolescents. For the same purpose, it is advisable to study the concentration of the protein that binds acetaminophen, which is an early marker of poisoning and toxic damage to the liver [19, 20].
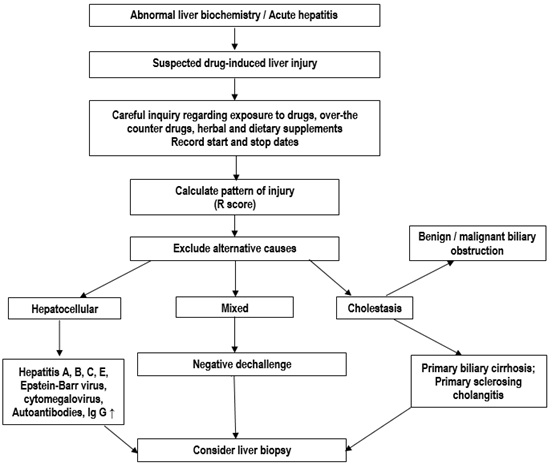
Figure 4: Diagram of diagnostic workup of drug-induced liver injury (Kullak-Ublick G.A. et al., 2017 with changes of authors).
In the presence of severe liver failure, early administration of balanced solutions containing ornithine and succinate is justified, as well as the use of extracorporeal replacement therapy, among which preference should be given to prolonged veno-venous hemodiafiltration, which avoids hyperhydration and prevents the progression of cerebral edema due to disturbances in water-electrolyte balance. It also should be noted that there is a high efficiency of the use of succinate preparations, which have a powerful cytoprotective, hepatoprotective and diuretic effect. That is why their purpose is pathogenetically justified in this situation [21]. It should also be noted that although specific therapy with the use of antidotes was not used in this case, it was reasonable even in the late stages of the disease, and for all poisonings that are characterized by liver damage.
CONCLUSION
A distinctive feature of this case was the favorable course of the disease in a teenage child, although the daily therapeutic dose of the drug was slightly exceeded, and the total dose was toxic. It is possible that the full healing was stemmed by the fact that the total dosage of acetaminophen was taken during three days but not like a shot, otherwise the risk of the severe liver injury could be much higher. The early implementation of complex therapy using efferent detoxification methods (prolonged venous-venous hemodiafiltration, membrane plasma sorption) made it possible to quickly achieve a therapeutic effect and prevent the development of multiple organ failure with subsequent complete restoration of liver function and recovery.
ACKNOWLEDGMENTS
The authors express their sincere gratitude to Andrei Lipin for his invaluable assistance in translating the manuscript into English.
REFERENCES
- Aleksandrovich YS, Pshenisnov KV, Gordeev VI (2014) Intensive therapy of critical states in children. pp. 976.
- Singh S, Hariram V, Jain S, Singh K (2000) Paracetamol (acetaminophen) poisoning: report of two cases. J Assoc Physicians India 48: 938.
- Filipovic-Grcic B, Novak M, Saric D (1995) Paracetamol poisoning--case report. Lijec Vjesn 117: 91-92.
- Kominek K, Paw?owska-Kamieniak A, Mroczkowska-Juchkiewicz A, Krawiec P, PacKo?uchowska E (2015) Intentional and accidental paracetamol poisoning in childhood-a retrospective analysis. Postepy Hig Med Dosw 69: 452-456.
- Nadler A, Fein DM (2018) Acetaminophen Poisoning. Pediatr Rev 39: 316-318.
- Bertrand X, Brasseur E, Ghuysen A, D'Orio V (2008) How I treat... paracetamol poisoning. Rev Med Liege. 63: 465-468.
- Rowden AK, Norvell J, Eldridge DL, Kirk MA (2006) Acetaminophen poisoning. Clin Lab Med 26: 49-65.
- Ramachandran A, Jaeschke H (2018) Oxidative stress and acute hepatic injury. Curr Opin Toxicol 7: 17-21.
- Rianprakaisang T, Blumenberg A, Hendrickson RG (2019) Methemoglobinemia associated with massive acetaminophen ingestion: a case series. Clin Toxicol 1-3.
- Sahu KK, Mishra AK, Lal A, George SV (2019) Acetaminophen induced methemoglobinemia. Clin Toxicol 17: 1.
- Star K, Choonara I (2015) How safe is paracetamol? Arch Dis Child 100: 73-74.
- Mund ME, Quarcoo D, Gyo C, Brüggmann D, Groneberg DA (2015) Paracetamol as a toxic substance for children: aspects of legislation in selected countries. J Occup Med Toxicol 10: 43.
- Markova IV, Afanas'ev VV, Cybul'kin JeK, Nezhencev MV (1999) Clinical toxicology of children and adolescents. Intermedica pp. 400.
- Vereshhagin EI, Dyrul AK, Kol'cov OV (2012) Clinical physiology in intensive pediatrics: teaching manual. In: Shmakov AN, Kohno VN. Novosibirsk: Sibmedizdat Novosibirsk State Medical University pp. 488.
- European Association for the Study of the Liver (2017) EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. J Hepatol 66: 1047-1081.
- Farrell SE (2020) Acetaminophen Toxicity. Medscape.
- Le Vaillant J, Pellerin L, Brouard J, Eckart P (2013) Acetaminophen (paracetamol) causing renal failure: report on 3 pediatric cases. Arch Pediatr 20: 650-653.
- Kullak-Ublick GA, Andrade RJ, Merz M, End P, Benesic A, et al. (2017) Drug-induced liver injury: recent advances in diagnosis and risk assessment. Gut 66: 1154-1164.
- Heard K, Anderson V, Dart RC, Kile D, Lavonas EJ, et al. (2017) Serum acetaminophen protein adduct concentrations in pediatric emergency department patients. J Pediatr Gastroenterol Nutr 64: 533-535.
- Alonso EM, James LP, Zhang S, Squires RH; Pediatric Acute Liver Failure Study Group (2015) Acetaminophen adducts detected in serum of pediatric patients with acute liver failure. J Pediatr Gastroenterol Nutr 61: 102-107.
- Aleksandrovich YS, Pshenisnov KV (2014) Infusion antihypoxants in children with critical conditions. General resuscitation 10: 59-74.
Citation: Aleksandrovich Yu S, Pshenisnov KV, Kaziakhmedov VA, Lodyagin AN, Udaltcov MA, et al. (2020) Acetaminophen Poisoning: A Cause of Acute Liver Failure in Pediatrics (Clinical Case). J Emerg Med Trauma Surg Care 7: 039.
Copyright: © 2020 Aleksandrovich Yury Stanislavovich, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

