
Colorectal Cancer – An Emergency Room Diagnosis in African Americans
*Corresponding Author(s):
Derrick J. BeechDepartment Of Surgery, Morehouse School Of Medicine, Atlanta, Georgia, United States
Tel:+1 4047521414,
Fax:+1 6157521594
Email:dbeech@msm.edu
Abstract
Colorectal (CRC) cancer is the second leading cause of cancer related deaths in the United States. Current screening guidelines recommend colonoscopy beginning at age 50 years for the general population. Regardless of well published guidelines for CRC screening, a significant number of African American (AA) patients have their initial diagnosis and subsequent care co-ordinated through the hospital Emergency Rooms (ER).
Methods: Retrospective database review spanning 1998-2002, extracted individuals with first CRC diagnosis using International Classification of Disease, 9th Edition, Clinical Modifications (152.00 - 154.89) data analysis was performed using cross-tabulation and binary logistic regression.
Results: A statistically significant proportion of African Americans had their initial diagnosis of CRC through an ER visit compared to Caucasians (42.4% vs. 21.9%, p-value <0.001).
Conclusion: African Americans disproportionately received an initial dignosis of CRC cancer through the ER services, as opposed to primary care screening and diagnosis. Further work is needed to promote pro-active health practices and screening for colon and rectal cancer in the African American communities.
Keywords
INTRODUCTION
Cancers of the colon and rectum combined are the third most common type of cancer, and the second most common cause of cancer death in the United States [1-3]. The American Cancer Society estimates in 2016 the total US cancer deaths will total 595,690. Estimated deaths due to colon and rectum cancer will represent 8% of this total [2]. A disproportionate number of cancer deaths occur among racial/ethnic minorities, particularly African Americans, whom have a 33% higher risk of dying of cancer than non-Hispanic whites [4]. Colorectal cancer incidence and mortality rates are 35% higher in men than in women. When looking at incidence and mortality based on race, African American men and women have the highest rates. Incidence rates among African American men and women are about 15% higher than in non-Hispanic white men and women [1-3].
The data is disproportionately worse for the state of Tennessee. While Tennessee has an overall higher death rate for colorectal cancer than the United States (21.6 vs 20.8 per 100,000 persons), African Americans die in greater proportion to their non-Hispanic white counterparts, after adjusting for age. In the state of Tennessee, the death rate for non-Hispanic whites versus the national rate is 19.9 and 20.3 respectively. The same age-adjusted rate for African Americans in the state of Tennessee versus the national rate is 35.5 and 28.3 [5].
Healthcare disparities exist across a broad range of medical and healthcare systems. These disparities are associated with higher mortality among minorities, and occur even when controlling for clinical factors, such as co-morbidities and stage of disease presentation. Survival differences have been noted between black and white patients with many cancers, including colorectal cancers [1]. To better understand the etiology of such disparities, we focused on evaluating initial presentation and diagnosis of colon or rectal cancers among different groups based on race and ethnicity. We sought to identify factors that may contribute to racial disparities among different ethnic groups, by analyzing the patient population that had emergent admissions and emergency room diagnoses. Our data highlights concerning trends in the diagnosis and clinical presentation of patients with colon and rectal cancer, and is to formulate programs and policies toward eliminating factors contributing to disparities.
METHODS
A retrospective database review spanning 1998-2002 was performed using the Tennessee Hospital Discharge Data (HDD). Chart information was reviewed using the International Classification of Disease Clinical Modifications (ICD) codes (152.00 – 154.89) with a focus on patients first diagnosed with Colorectal Cancer (CRC). This provided the data to analyze the primary or secondary diagnosis of colon or rectal cancer and patients discharged from hospital facilities, throughout the state of Tennessee. In addition, the HDD included demographics (race/ethnicity, age and gender) and type of insurance. The total number of patients studied in our population was 16,913. There were 2,439 African Americans, 13,486 Caucasians, 988 cases of other ethnicities including Hispanic, Asian and American Indian. Gender distribution included 8,054 females (1,332 African Americans, 6,722 Caucasians) and 7,871 males (1,107 African Americans, 6,764 Caucasian). Cross-tabulation and binary logistic regression were used in the statistical analysis of the data. There was an adequate sample size of patients of Non-Hispanic African Americans and Non-Hispanic Caucasians ethnic groups. The Hispanic, Asian and other racial categories had limited sample sizes preventing adequate analysis.
RESULTS
Our analysis focused on the racial disparities between African Americans and Caucasians. The initial component of our hypothesis was to confirm that African Americans were more likely to receive their initial diagnosis in the emergency department and require emergent admissions for CRC treatment. African Americans were 20% more likely to be diagnosed with CRC in the emergency department and 20% more likely to require emergent intervention. While Caucasians were 20% more likely to be admitted through physician referrals, and 20% more likely to have an elective intervention, with a 20% less likely chance to have an emergent intervention (Tables 1 and 2).
| African American | Caucasian | ||||
| Type of Admissions | Frequency | Percentage | Frequency | Percentage | p-value |
| Emergency Admission | 1,026 | 42.40% | 3,154 | 21.90% | <0.001 |
| Physician Referral | 1,352 | 55.90% | 10,808 | 75.10% | <0.001 |
| Clinic or HMO Referral | 11 | 0.40% | 36 | 0.30% | <0.001 |
| Transfer from Other Facility | 23 | 1.00% | 196 | 1.40% | <0.001 |
| Other | 8 | 0.30% | 188 | 1.30% | <0.001 |
| Total | 2,420 | 14,382 | |||
Table 1: Race Differences in Source of Admission.
The table demonstrates a significance (p-value <0.001) in CRC diagnosis, when comparing frequency of CRC diagnosis with source of admission, in respect to race.
Emergency admission: Patient was admitted for inpatient services or referred for outpatient services, upon the recommendation of this facilities emergency room physician.
Physician referral: Patient was admitted for inpatient services, referred for outpatient services upon the recommendation by his/her personal physician, the patient independently requested outpatient services.
Clinic referral/HMO referral: Patient was admitted for this facility for inpatient services or referred to the facility for outpatient services upon the recommendation for the facilities physician. HMO referral is defined as an admission for inpatient service or referred for outpatient services, upon recommendation of a health maintenance organization physician.
Transfer from other facility: Patient was admitted to this facility as a hospital transfer from either an acute care facility, skilled nursing facility or healthcare facility, where he/she was inpatient or referred to this facility for outpatient services.
| African American | Caucasian | |||||
| Type of Admissions | Frequency | Percentage | Frequency | Percentage | p-value | |
| Emergency | 1,011 | 41.40% | 3,121 | 20.90% | <0.001 | |
| Urgent | 416 | 17.0% | 2,807 | 18.80% | <0.001 | |
| Elective | 1,012 | 41.40% | 8,942 | 60.0% | <0.001 | |
| Other | 4 | 0.1% | 50 | 0.3% | <0.001 | |
| Total | 2,420 | 14,920 | ||||
Emergency: The patient requires immediate intervention, as a result of severe, life threatening or potentially disability condition.
Urgent: The patient requires immediate attention for the care and treatment of a physical or mental disorder.
Elective: The patient’s condition permits adequate time to schedule the availability of suitable accommodations.
The results further demonstrated that the racial disparities in diagnosis of CRC and level of intervention were independent of gender, age, and primary pay or type or zip-code. Gender, age, self-pay and Non-TNcare government pay or status all independently contributed to the risk of emergency department CRC diagnoses [6] (Table 3).
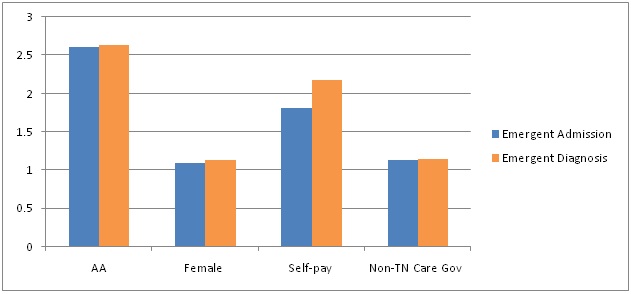
Neighborhood (measured by zip code) characteristics also affected the likelihood of emergent admissions or emergency diagnoses, and were associated with higher risk of emergency department diagnoses (Table 4). When controlling for these variables African Americans remained more than twice as likely to be diagnosed via the emergency department.
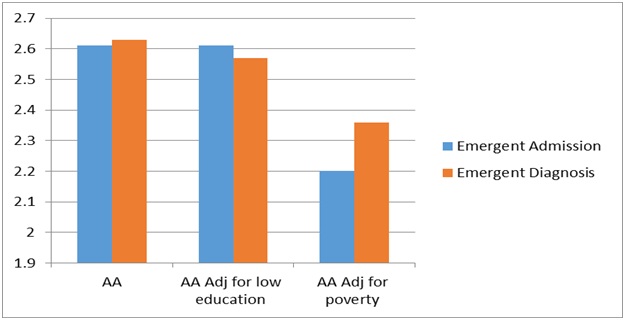
The data illustrates that African Americans were approximately 2.6 times more likely to receive their CRC diagnoses in the emergency room or emergent admissions for CRC. Poverty and low educational attainment compound these disparities. The findings for older adults are particularly surprising, since Medicare removed much of the financial barriers to treatment prior to 1998 by covering CRC screening procedures. Despite having access to Medicare as a primary source of health insurance, elderly patients (both African Americans and Caucasian) were 13% more likely to receive their diagnoses via the emergency department relative to privately insured or those patients with TNCARE coverage (Tennessee’s state Medicaid program). Our analysis of the Tennessee HDD demonstrate the disparity associated with African Americans and elderly patients’ greater need for emergent admissions, and the greater likelihood of an emergency department CRC diagnosis. The results are consistent with lower rates of screening among African Americans. Note that our findings in the Medicare population did little to illuminate racial disparities, since Medicare payor status increased the risk equally of emergency room diagnosis of CRC in all the patients in the database.
CONCLUSION
These findings reveal significant racial disparities in emergency department CRC diagnoses and need for emergent admissions. Our analysis demonstrates the higher rates of emergency room CRC diagnosis and admissions for African Americans were not due to confounding effects of gender, age, type of insurance, zip code or level of education. The data supports our hypothesis that there are disproportionate numbers of emergent and urgent visits with respect to socioeconomic status. Patients whose primary payer was TNCARE or private insurance were least likely to receive emergency CRC diagnoses. Patients without any insurance (self-pay) were most likely to receive emergency CRC diagnoses. Government pay, which was primarily Medicare, also had an increased risk of CRC diagnosis via the emergency room, even after controlling for age. We find it intriguing that these patients were not undergoing routine screening despite the coverage for such procedures. Limitations of our study are secondary to the use of the Tennessee Hospital Discharge Data, which does not contain information regarding tumor characteristics or stage of disease. Further, our study relied on zip code, as a surrogate marker of level educational attainment and poverty rather than explicit income information for the individual patient. Lastly, our analysis did not include measures of co-morbid physical or mental diagnoses. Future studies should include co-morbidity index.
DISCUSSION
There are currently several federally sponsored campaigns focused on health disparity reduction. The publication, “Healthy People 2010, Objectives for the Nation”, has set 437 objectives for this decade with two overarching goals: longer years of healthy life and the elimination of health disparities [7,8]. The Institute of Medicine identified six aims for healthcare, which include equitable in finance, access, and outcomes [2,3]. Cancer surveillance can make a significant contribution to cancer prevention and care, as well as to reducing cancer disparities, related to mortality [9]. Colorectal cancer screening allows for both prevention and early detection of cancer, with early detection often resulting in improved prognosis [10]. Despite these benefits, the proportion of the US population aged 50 and older that has been screened remains low.
In 1996, Cooper and associates examined the survival of 81,579 Medicare beneficiaries with an initial diagnosis of colorectal cancer in 1987. Their data found that black patients were less likely than white patients to undergo surgical resection (68% vs 78%), even after age, co-morbidity, location and extent of tumor were controlled [11]. Among those who underwent resection, black patients were more likely to die (a two-year mortality of 40.0% vs 33.5% in white patients), even after confounders had been controlled. These disparities were similar in teaching and non-teaching hospitals, and in private and public hospitals. The authors suggested the observed differences might be related to deficiencies in access and quality of care. Again, a substantial number of African American patients diagnosed with CRC in the emergency room setting are an example of unfavorable trends in screening and access to care.
Studied the survival of colorectal cancer patients in what he described as an “equal access” medical system, the nationwide Veterans Affairs Medical Centers” [11,12]. After adjusting for patient demographics, co-morbidities, distant metastases, and tumor location there was no difference found in the percent of black and white patients undergoing surgical resection (70% vs 73%), chemotherapy (23% vs 23%) or radiation therapy (17% vs 16%). The authors concluded that when there is equal access to care, there are no differences with regard to race in the comprehensive management of colorectal cancers in their cohort. It is unclear why two of these population based studies had different conclusions.
A Medline search of English language article published between 1980 and 2000 was performed by, and yielded 46 relevant multi-institutional or population based studies [13,14]. This meta-analysis concluded that in the United States, black patients with colorectal cancer receive less aggressive therapy and are more likely to die of the disease than white patients. Patients of low Socioeconomic Status (SES) have worse survival than patients of higher SES. Additionally, it has been suggested that surgeon expertise and case volume are associated with improved tumor control. Variations in treatment may arise from inadequate physician knowledge of practice guidelines, treatment decisions based on unmeasured clinical factors or patient preferences.
Several studies have shown other barriers to CRC screening. These barriers include the following: inadequate communication between health care providers and patients about screening, physician attitude and beliefs about the effectiveness of CRC screening tests, familiarity with screening guidelines, perception of patient preferences and adherence, lack of healthcare insurance, patients’ lack of interest, cost, embarrassment, unpleasantness of test, or patient unawareness regarding the importance and benefits of screening [2]. While each of these factors has been recognized as potentially important, given the magnitude of the problem, and lack of progress over the last three decades, closing this disparity gap requires renewed focus on this issue, and careful analysis of patient and physician variables. Given the increasing disparities in mortality for minority populations with colorectal cancer, examination of the data in this population based study demonstrated that African Americans have a disproportionately higher rate of emergent and urgent admissions.
There were limitations to our use of Tennessee HDD. While administrative data sets or population-based studies provide important information regarding the treatment outcomes of care, these sources often lack important variables that may determine ultimate survival (i.e., extent of resection, tumor margins of resection, completion of initiated adjuvant therapy and post treatment surveillance). In the present study, such limitations will be overcome due, in part, to the unique nature of the American College of Surgeons National Cancer Data Base. Additionally, the institutions that have agreed to allow their NCDB data to be reviewed are renowned for the quality of their clinical expertise and documentation. The availability of this resource provides an important opportunity to gain new knowledge about how best to provide optimal, safe care for colon cancer to all patients; particularly, to patients from the minority populations.
Upon complete review of the data, if we are correct in our hypotheses, then we must prepare a plan of action to first discover the etiology, and then eliminate these disparities in the state of Tennessee. Further work is needed to promote pro-active health practices and screening for CRC in the African American communities. The use of targeted community outreach approaches such as informational lectures (churches, community centers in disadvantaged neighborhoods) and invitations for screening through public service radio announcements should be investigated. Funding colonoscopy screening at no or low cost co-pay in hopes of increasing willingness to screen should perhaps be studied. Pursuit of further research toward understanding why Medicare reimbursement for CRC screening has not led to optimal utilization should also be taken into consideration. This study highlights the need to enhance programs that promote CRC screening in African Americans.
ACKNOWLEDGMENT
This research was supported by Morehouse School of Medicine and the NIH U54 CA 118638.
REFERENCES
- American Cancer Society (2014) Colorectal Cancer Facts and Figures. American Cancer Society, Atlanta, GA, USA.
- American Cancer Society (2016) Cancer Facts and Figures 2016. American Cancer Society, Atlanta, GA, USA.
- Bezold C (2006). Disparities, cancer surveillance, and next steps. J Cancer Educ 21: 61-68.
- Brawley OW, Freeman HP (1999) Race and outcomes: is this the end of the beginning for minority health research? J Natl Cancer Inst 91: 1908-1909.
- Cairns CP, Viswanath K (2006) Communication and colorectal cancer screening among the uninsured: data from the Health Information National Trends Survey (United States). Cancer Causes Control 17: 1115-1125.
- Dayal H, Polissar L, Yang CY, Dahlberg S (1987) Race, socioeconomic status, and other prognostic factors for survival from colo-rectal cancer. J Chronic Dis 40: 857-864.
- American Cancer Society (2005) Colorectal Cancer Facts and Figures - Special Edition 2005. American Cancer Society, Atlanta, GA, USA.
- CDC (2012) Healthy People 2010. US Department of Health and Human Services Office of Disease Prevention and Health Promotion, CDC, Atlanta, GA, USA.
- Chu KC, Tarone RE, Chow WH, Alexander GA (1995) Colorectal cancer trends by race and anatomic subsites, 1975 to 1991. Arch Fam Med 4: 849-856.
- Cooper GS, Yuan Z, Landefeld CS, Rimm AA (1996) Surgery for colorectal cancer: race-related differences in rates and survival among Medicare beneficiaries. Am J Public Health 86: 582-586.
- Dominitz JA, Samsa GP, Landsman P, Provenzale D (1998) Race, treatment, and survival among colorectal carcinoma patients in an equal-access medical system. Cancer 82: 2312-2320.
- Mayberry RM, Coates RJ, Hill HA, Click LA, Chen VW, et al. (1995) Determinants of black/white differences in colon cancer survival. J Natl Cancer Inst 87: 1686-1693.
- Hodgson DC, Fuchs CS, Ayanian JZ (2001) Impact of patient and provider characteristics on the treatment and outcomes of colorectal cancer. J Natl Cancer Inst 93: 501-515.
- Polite BN, Dignam JJ, Olopade OI (2005) Colorectal Cancer and Race: Understanding the Differences in Outcomes Between African Americans and Whites. Med Clin North Am 89: 771-793.
Citation: Stokes M, Husaini BA, Kilbourne B, Cain V, McGarity D, et al. (2017) Colorectal Cancer - An Emergency Room Diagnosis in African Americans. J Emerg Med Trauma Surg Care 4: 020.
Copyright: © 2017 Myron Stokes, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

