
Congenital Diaphragmatic Hernia with Extra-Lobar Pulmonary Sequestration Presenting As Gastric Volvulus in a Healthy 24-Year-Old Female
*Corresponding Author(s):
Hannah R. MedeckDepartment Of Surgery, University Of Colorado Anschutz Medical Campus, Aurora, CO, United States
Tel:605-381-1848,
Email:Hannah.Medeck@coyotes.usd.edu
Abstract
Congenital diaphragmatic hernias (CDH) carry significant morbidity and mortality risk due to compressive effects in the thorax during organogenesis and impaired development of lung tissue and vasculature. Prenatal screening now often allows for diagnosis of CDH in utero and for subsequent coordination of neonatal medical and surgical therapies to limit the early mortality risk. Here we discuss delayed presentation in a healthy 24-year-old female with diffuse abdominal pain secondary to gastric volvulus. Intraoperatively, this patient was found to have a previously undiagnosed congenital diaphragmatic hernia and concurrent extralobar pulmonary sequestration which mimicked gastric perforation on preoperative imaging. Concurrent congenital abnormalities of organogenesis with CDH and pulmonary sequestration have been described. These concurrent pathologies must be in the differential for surgeons operating on adults with late presentation of CDH. Sequestered lung tissue has a risk of malignant transformation and chronic infection necessitating thorough exploration of the hernia sac for identification of this concurrent pathology and careful resection of sequestered pulmonary tissue during CDH repair.
Keywords
Congenital Diaphragmatic Hernia; Extralobar Pulmonary Sequestration; Gastric Volvulus
INTRODUCTION
Congenital diaphragmatic hernia (CDH) occurs in less than 5/10,000 births [1,2] with morbidity and mortality mainly related to its pulmonary effects secondary to muscular hyperplasia of the pulmonary vasculature and decreased arterial branching [3]. CDH is frequently syndromic with other malformations, most commonly of the gastrointestinal and genitourinary systems in 25% of cases, while the incidence of a coexisting pulmonary sequestration is much lower at around 5% according to the Congenital Diaphragmatic Hernia Study Group registry data [4]. While the majority of pulmonary sequestrations are found as intralobar malformations, approximately 25% manifest as extralobar sequestrations found within the thoracic or peritoneal cavity with their own pleural membranes and complete anatomic separation from the normal lung [5]. Due to increased availability of prenatal care and imaging, CDH is primarily diagnosed during the prenatal period or during early childhood [6]. Here we present a case of a healthy 24-year-old female presenting with gastric volvulus secondary to an undiagnosed CDH and the incidental finding of associated extralobar pulmonary sequestration mimicking gastric perforation.
CASE REPORT
This 24 year old previously healthy Somalian woman presented to the emergency department with 12 hours of worsening diffuse abdominal pain with nausea and emesis, initially attributed to reflux disease by patient. She was previously evaluated for similar symptoms in 2014 and was discharged after improvement with antiemetics and pain medication. On exam, the patient was tachycardic with abdominal distension and tenderness to palpation in left upper quadrant and epigastric region without rebound tenderness or involuntary guarding. Laboratory values were significant for lactic acidosis of 3.5 mmol/L and leukocytosis of 12,300/mm3. Chest X-ray showed thoracic herniation of the stomach (Figure 1), and commuted tomography of the abdomen and pelvis demonstrated a mesenteroaxial gastric volvulus in the left thoracic cavity and a small adjacent fluid collection with internal foci of air concerning for a contained gastric perforation (Figure 2a-c).
 Figure 1: Diaphragmatic herniation of stomach, pre-operative chest x-ray.
Figure 1: Diaphragmatic herniation of stomach, pre-operative chest x-ray. Figure 2a: Mesenteroaxial gastric volvulus with suspected contained perforation (arrow), commuted tomography coronal view.
Figure 2a: Mesenteroaxial gastric volvulus with suspected contained perforation (arrow), commuted tomography coronal view.
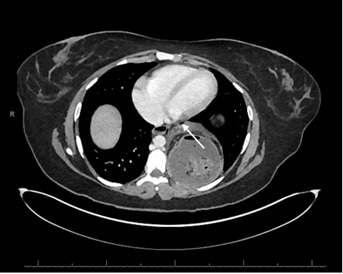 Figure 2b: Mesenteroaxial gastric volvulus with suspected contained perforation (arrow), CT axial view.
Figure 2b: Mesenteroaxial gastric volvulus with suspected contained perforation (arrow), CT axial view.
 Figure 2c: CDH with gastric volvulus, CT coronal view.
Figure 2c: CDH with gastric volvulus, CT coronal view.
The patient was promptly taken to the operating room for laparoscopic reduction of her presumed type IV posterolateral lumbar paraesophageal hernia with gastric volvulus. Intraoperatively, a 14 cm left sided diaphragmatic hernia containing the volvulized stomach and spleen was visualized. Reduction of hernia and reversal of the volvulus was easily achieved laparoscopically and neither the stomach nor spleen appeared ischemic. Due to the size of the defect and extent of the intrathoracic hernia sac the decision to convert to open laparotomy for complete sac excision and hernia repair was made. Careful exploration and excision of the complete hernia sac within the chest revealed no obvious gastric perforation, however, an extralobar pulmonary sequestration was discovered in the area concerning for fluid collection on the CT (Figure 3).
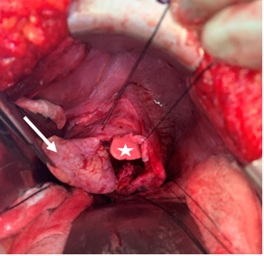 Figure 3: Left sided diaphragmatic hernia with normal lung (star) and extra lobar pulmonary sequestration (arrow).
Figure 3: Left sided diaphragmatic hernia with normal lung (star) and extra lobar pulmonary sequestration (arrow).
The pulmonary sequestration was then resected with ligation of the anomalous arterial supply originating from the supra-celiac abdominal aorta and venous drainage to the left inferior pulmonary vein (Figure 4). No anatomic communication between the sequestered lung tissue and the normal bronchial tree or adjacent lung was present. The diaphragmatic defect was too large for a primary closure, so the small amount of tissue surrounding the defect was first plicated and then repaired with a Gortex dual mesh on lay (Figure 5).
 Figure 4: Excised pulmonary sequestration (arrow) with hernia sac (star), silk suture on systemic artery coming directly from aorta.
Figure 4: Excised pulmonary sequestration (arrow) with hernia sac (star), silk suture on systemic artery coming directly from aorta.
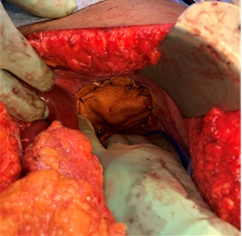 Figure 5: Diaphragmatic hernia repair with dual mesh.
Figure 5: Diaphragmatic hernia repair with dual mesh.
This hernia was due to a congenital absence of the patient’s entire left diaphragm and not due to trauma, so the hiatal crus was able to be repaired to a normal size and the patient’s gastroesophageal junction became fixed in the abdomen. Because of this, gastropexy or an anchoring gastrostomy tube, although considered, were not deemed necessary. In addition to the mesh, the spleen abutted this repair reducing the risk of recurrence of the hernia. A chest tube and abdominal drain were placed and the abdomen was closed. The patient was extubated post-operatively without complications and monitored in the ICU for pain control and respiratory status. Post-operative day one chest x-ray demonstrated stable repair of the diaphragm with recruitment of the normal left lung and left mediastinal shift related to flattening of the diaphragm with repair and removal of the previous volume of sequestered lung tissue (Figure 6). The patient was discharged in stable medical condition on room air on post-operative day six. At subsequent one month follow up, patient is recovering well with mild dyspnea while supine that has been improving.
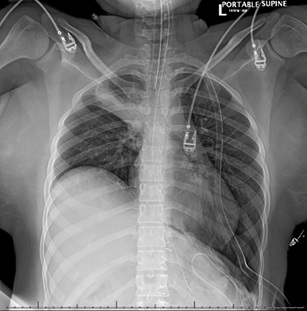 Figure 6: Diaphragmatic changes, post-operative day one post .CDH repair.
Figure 6: Diaphragmatic changes, post-operative day one post .CDH repair.
DISCUSSION
A congenital diaphragmatic hernia is defined as abdominal contents found in the thoracic cavity due to a congenital absence of diaphragmatic tissue. The association of extralobar pulmonary sequestrations with congenital diaphragmatic hernia is thought to be due to the timing of organogenesis [7]. An extra pulmonary sequestration forms when an accessory lung bud branches from the primitive foregut during weeks 5-17 of the pseudoglandular stage of lung development [8]. The presence of extra pulmonary tissue could mechanically inhibit fusion of the pleuroperitoneal folds around week 10, preventing diaphragm closure [9].
In this report, we present a rare case in which a congenital diaphragmatic hernia with extrapulmonary sequestration was discovered in an adult presenting as gastric volvulus. Due to early detection screening and the high mortality associated with CDH, 59% of cases are diagnosed within 24 hours of birth [10,11]. Late detection of congenital diaphragmatic hernias can present as gastric volvulus and wandering spleen, both of which were present in this patient. This is thought to be due to abnormal laxity of the diaphragm and/or abnormal or absent of peritoneal attachment to the stomach and spleen [12,13].
This patient’s asymptomatic medical history may be explained by the combination of limited prenatal screening and the presence of her pulmonary sequestration. It is hypothesized that pulmonary sequestrations may have a protective effect on congenital diaphragmatic hernias because the presence of extra-lobar tissue prevents herniation of abdominal contents into the chest cavity [14]. Additionally, the presence of a hernia sac in CDH cases is a risk-reducing prognosticator, with greater fetal lung growth, less visceral herniation, and better outcomes seen in infants with a hernia sac compared to those without [15]. This case highlights the need for providers to maintain a high index of suspicion for these concurrent pathologies and for complete surgical exploration of the intrathoracic hernia sac in patients presenting with possible congenital diaphragmatic hernia. These pulmonary sequestrations also warrant surgical excision even if asymptomatic and found incidentally. Extralobar pulmonary sequestration carries the risk of chronic infection, hemothorax, torsion, infarction, and potential for malignant degeneration [16-19]. Though the risk of infection of an extralobar pulmonary sequestration (14%) is lower than that of an intralobar pulmonary sequestration (91%), the presence of chronic inflammatory cells in an ELS is 35%. More than half of extralobar pulmonary sequestrations have co-exiting congenital cystic adenomatous malformations, and 8.6% of malignant pleuropulmonary blastomas in infants and bronchoalveolar carcinomas in adults were associated with congenital cystic lung malformations [20]. Careful dissection must be used as the systemic vasculature supply can be quite large and may originate from either the thoracic or abdominal aorta posing risk for significant operative risk and blood loss if not precisely identified and controlled [21-23].
REFERENCES
- Torfs CP, Curry CJ, Bateson TF, Honoré LH (1992) A population-based study of congenital diaphragmatic hernia. Teratology 46: 555-565.
- Tovar JA (2012) Congenital diaphragmatic hernia. Orphanet J Rare Dis 7: 1-1.
- Bloss RS, Aranda JV, Beardmore HE (1981) Congenital diaphragmatic hernia: pathophysiology and pharmacologic support. Surgery 89: 518-524.
- Askin FB, Gilbert-Barness E (2007) Respiratory system. In: Gilbert-Barness E, Kapur RP, Oligny LL, Siebert JR, eds. Potter's Pathology of the Fetus, Infant and Child. (2nd edn), Mosby Elsevier, Philadelphia, USA, pp. 1108-1132.
- Frazier AA, Rosado de Christenson ML, Stocker JT, Templeton PA (1997) Intralobar sequestration: radiologic-pathologic correlation. Radiographics 17: 725-745.
- Bouchqhoul H, Senat MV, Storme L, de Lagausie P, Begue L, et al. (2015) Congenital diaphragmatic hernia: does gestational age at diagnosis matter when evaluating morbidity and mortality? Am J Obstet Gynecol 213: 535.e1-7.
- Panda S (2018) Left Side Congenital Diaphragmatic Hernia with Sac and Broncho-Pulmonary Sequestration: A Report to Reinforce The Need to Excise the Hernia Sac. Biomedical Journal of Scientific & Technical Research, 6: 1-2.
- Correia-Pinto J, Gonzaga S, Huang Y, Rottier R (2010) Congenital lung lesions--underlying molecular mechanisms. Semin Pediatr Surg 19: 171-179.
- Clugston RD, Greer JJ (2007) Diaphragm development and congenital diaphragmatic hernia. Semin Pediatr Surg 16: 94-100.
- Peetsold MG, Heij HA, Kneepkens CMF, Nagelkerke AF, Huisman J, et al. (2009) The long-term follow-up of patients with a congenital diaphragmatic hernia: a broad spectrum of morbidity. Pediatr Surg Int 25: 1-17.
- Garne E, Haeusler M, Barisic I, Gjergja R, Stoll C, et al. (2002) Congenital diaphragmatic hernia: evaluation of prenatal diagnosis in 20 European regions. Ultrasound Obstet Gynecol 19: 329-333.
- Cantone N, Gulia C, Miele V, Trinci M, Briganti V (2016) Wandering spleen and organoaxial gastric volvulus after morgagni hernia repair: a case report and review of the literature. Case Rep Surg 2016: 6450765.
- Flores-Rios E, Mendez-Diaz C, Rodriguez-Garcia E, Pérez-Ramos T (2015) Wandering spleen, gastric and pancreatic volvulus and right-sided descending and sigmoid colon. J Radiol Case Rep 9: 18-25.
- Lee MY, Won HS, Shim JY, Lee PR, Lee BS, et al. (2012) Protective effect of fetal pulmonary sequestration in two cases of postnatal manifestation of congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 39: 719-722.
- Zamora IJ, Cass DL, Lee TC, Welty S, Cassady CI, et al. (2013) The Presence of a Hernia Sac in Congenital Diaphragmatic Hernia Repair is Associated with Better Fetal Lung Growth and Outcomes. J Pediatr Surg 48: 1165-1171.
- Sato S, Kitahara A, Koike T, Hashimoto T, Ohashi R, et al. (2016) A Case of Ectopic ACTH-Producing Pulmonary Carcinoid Arising in an Extralobar Pulmonary Sequestration. Int J Surg Pathol 24: 130-134.
- Kao MW, Tsai JH, Lee JM (2013) Pulmonary sequestration presenting as an esophageal submucosal tumor. Thorac Cardiovasc Surg 61: 510-512.
- Hall NJ, Stanton MP (2017) Long-term outcomes of congenital lung malformations. Semin Pediatr Surg 26: 311-316.
- Hertzenberg C, Daon E, Kramer J (2012) Intralobar pulmonary sequestration in adults: three case reports. J Thorac Dis 4: 516-519.
- Laberge JM, Puligandla P, Flageole H (2005) Asymptomatic Congenital Lung Malformations. Semin Pediatr Surg 14: 16-33.
- McGivern MR, Best KE, Rankin J, Wellesley D, Greenlees R, et al. (2015) Epidemiology of congenital diaphragmatic hernia in Europe: a register-based study. Arch Dis Child Fetal Neonatal Ed 100: F137-144.
- Corbett HJ, Humphrey GM (2004) Pulmonary sequestration. Paediatr Respir Rev 5: 59-68.
- Grethel EJ, Farrell J, Ball RH, Keller RL, Goldstein RB, et al. (2008) Does congenital diaphragmatic hernia associated with bronchopulmonary sequestration portend a better prognosis? Fetal Diagn Ther 23: 250-253.
Citation: Medeck HR, Svete L, Lai SH, Hilton S, Peltz E (2019) Congenital Diaphragmatic Hernia with Extra-Lobular Pulmonary Sequestration Presenting As Gastric Volvulus in a Healthy 24-Year-Old Female. J Emerg Med Trauma Surg Care 6: 037.
Copyright: © 2019 Hannah R. Medeck, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

