
Evaluation of Self-Monitoring Blood Glucose Practice and Associated Factors among Type-1 Diabetic Patients at St.Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
*Corresponding Author(s):
Halefom KahsayDepartment Of Pharmacy, College Of Medicine And Health Science, Adigrat University, Tigray, Ethiopia
Email:heleka94@gmail.com
Abstract
Background:Now a days Self-Monitoring Blood Glucose (SMBG) becomes the cornerstone in daily blood glucose management inType 1 Diabetic Patients (T1DM) and making them better able to adjust their insulin doses. Ithas the potential to improve problem-solving and decision making skills for both the person with diabetes and his or her health care professional to adjust therapy and assess the responses to therapy. Since the prevalence of diabetes increasing, successful management of blood glucose control could be very important. However, relatively little is known about current practice, pattern and barriers associated withSMBG in the hospital.
Objective: This study was aimed to assess the performance and factors associated with SMBG level among T1DM attended to diabetes outpatient clinics of St. Paul’s Hospital Millennium Medical College(SPHMMC).Data were collected using a structured questionnaire and chart reviewed. Multivariate logistic regression model was analyzed to find the association.
Methods:Data were collected using a structured questionnaire. Multivariate logistic regression model was analyzed to find the association.
Result:Nearly two-third (65.2%) of patients performed SMBG levelirrespective of frequency while only 68(42.2%) of them preformed three times daily. Being male was significantly associated with less performance of SMBG (AOR=0.43, 95%CI: (0.23-0.80)).Whereas, educational level (primary school, AOR=4.29, 95%CI: 1.24-14.90) and shorter duration with diabetes (<1years and 1-5years), (AOR=4.45, 95%CI: 2.19-9.05 and AOR=8.85, 95%CI: 3.45- 22.73) respectively, were found to be significantly associated with better performance of SMBG.
Conclusion: The findings indicated that the performance of SMBG was suboptimal, which warrants the need for health care providers engaged in diabetic care to aggressively address the issue. Furthermore, this study endorses the necessity of further support in performing SMBG and increased availability of other tools for glucose monitoring. We also advocate the inclusion of blood glucose meters, blood glucose test strips in health insurance program in Ethiopia to ease the burden of self- monitoring in diabetic patients.
Keywords
Blood Glucose Control;Self- Monitoring Blood Glucose; Type 1 Diabetes
BACKGROUND
Self-monitoring of Blood Glucose (SMBG) is an important component of modern therapy for diabetes mellitus [1]. Patients with type 1 diabetes (T1DM) started using instruments for self-monitoring of blood glucose (SMBG) in the early 1980s.This quickly became the cornerstone in daily blood glucose management in type 1 diabetes, making patients better able to adjust their insulin doses andto monitortheir blood glucose (BG) level [2]. Furthermore, it is recognized as an important tool that guides glycemic management strategies and has the potential to improve problem-solving and decision-making skills for both the person with diabetes and his or her health care professional to adjust therapy and assess the responses to therapy. The good performance of SMBG provides anacceptably accurate reflection of immediate plasma glucose levels which is commonly used currently in diabetic patients [3,4]. Therefore, People with diabetes can reduce or prevent the impairment of BGby monitoring their blood sugar levels frequently and learning to recognize the symptoms of low blood sugar and the situations that can trigger it [5].
One of the primary goals of diabetes management is to maintain the blood glucose levels becauseit is well established that frequent monitoring of blood glucose level delays the onset and retards the progression of microvascular and microvascular complications. So that, the International Society for Pediatrics and Adolescent Diabetes (ISPAD) recommended that SMBG at a frequency of usually four to six times a day, to optimize diabetes control, because frequency of SMBG correlates with glycemic control[6]. In addition to this, the American diabetic association (ADA) suggested that, although individual needs may vary, SMBG testing 6–8 times daily should be considered prior to meals and snacks, occasionally postprandial, at bedtime, prior to exercise, when they suspect low blood glucose, after treating low blood glucose until they are norm glycemic, and prior to critical tasks such as driving, vagarious exercises[7].Practically, one study conducted in a group of 30 voluntaries of T1DM patients at university ofVirginia to determine actual frequency of SMBG compared with self-report and physician’s recommendation. About 47% of the subjects obtained an average of three or more self-measurements per day, 23% averaged one daily measurement, 20% averaged two dailymeasurements and very few subjects averaged less than one self-measurement per day.It had also determined that peoples with higher education and thosewho had self-adjustment of insulin were associated with frequent SMBG[8]. Furthermore, a cross sectional study was done in 150 T1DM to estimatethe association between HbA1c andSMBG-frequency suggested that good diabetes control hasachieved in routine diabetes care with a minimum of 4 SMBGs per day [9].Another national survey in France determined SMBG in T1DM patientsshowed that 58% of participates took at least three tests a day [10].
Factors associated with self-monitoring of blood glucose level have been supported with differentmarkers. A population based cross sectional study in North California reported that longer timesince diagnosis, less intensive therapy, male sex and older age were associated with non-adherence to perform SMBG [11]. On the other hand, a survey-based cross-sectional study conducted at Swedenin five diabetes sites, which determined adherence to SMBG among T1DM patients showed that older age and female gender were significantly associated with frequent (≥4 per day) SMBG [12].Furthermore, one retrospective cohort study conducted in Germany and seen an association between SMBG and T1DM demographic characteristics revealed that only younger age were associated with frequent (at least 4.4 per day) performance of SMBG[13].Another cross-sectional study assessed SMBG practice among insulin treated patients in Jos, Nigeria reported that high level of education, high income, long duration of diabetes and male sex were found significantly associated with better performance of SMBG [14].
According to the current International Diabetes Federation report (IDF) 425 million people havediabetes in the world. If nothing is done, the number of people with diabetes may rise to 693 million in 2045. The estimates of children and adolescents below age 19 with type 1 diabetes has risen to over a million since the prevalence of diabetes increasing, successful management of BG control could be very important[15]. People with T1DM, with proper daily insulin treatment, regular bloodglucose monitoring and maintenance of a healthy diet and lifestyle can live a healthy life and delay or avoid many of the complications associated with diabetes[16,17].Although, Diabetes selfmanagement and SMBG are encouraged in health institutions, relatively little is known about current practice, pattern and barriers associated withSMBG in our environment. Therefore, we were assessed the performance of SMBG as well as the factors associated with it among T1DM patients attending to the outpatient diabetic specialty clinics a SPHMMC.Besides, high level of concern should be given to the contributing factors for SMBG that leads the patient to additional morbidity. Based on the compelling evidence of thepotential harms associated with impairment of BG level in T1DM patients, the size of the problem, assessing the performance of SMBG with its possible contributing factors that were investigated in the past studies are not enough.Thus, this further research, may dig out a significant outcomes regarding SMBG practice in the study area. Additionally, it could have an inputto initiate further studies on SMBGperformance of diabetic patients, advanced home care self-management the complications of diabetes mellitus and educationalprograms for health care professionals.
MATERIAL AND METHODS
This cross sectional study design was conducted to assess the performance of SMBG and its associated factors among ambulatory T1DM patients attending at the diabetic clinics of SPHMMC. An average of 20 T1DM patients under 18years old is followed every Monday afternoon in the pediatric diabetes site. Besides, adults above 19 years’ age were attended to the main outpatient room every Wednesday and Thursday working hours with average 10 TDM1 patients each day. An average of 5 T1DM patients was also attended every Friday morning. Patient interview and retrospective patient chart review for the same patient was conducted from 1st of June to 1st of August 2017.Study population were selected among all T1DM patients having follow up at the study area during the study period who fulfilled the inclusion criteria. Patients 5years and above who were diagnosed as T1DM were eligible for inclusion. Whereas thoseT1DM patients who were pregnant, with other chronic comorbidities (Cirrhosis, heart and kidney failure infectious diseases) and those with incomplete/inaccessible medical chart were excluded.
The sample size (n) was calculated assuming a 50% proportion (p) of hypoglycemia prevalence, a5% marginal error (d) and a confidence interval (CI) of 95%. Based on this assumption the samplesize was calculated by a single population proportion formula.
This yields a sample size of 384. The expected number of source population in the study period (N), based on the average number of patients coming to the diabetic sites during the diabetic days of the study period were given us 540. It was calculated by the total sum of 12*10,12*10, 12*5 for those who were averagely attend every Wednesday, Thursday working hours and Friday morning respectively. Additionally, 12*20 for those who attend every Monday afternoon. The sample size was adjusted and calculated using the following formula:Corrected sample size=.
Due to the fact that there is a non- response (with an acceptable level of 10%), 10% of the calculated sample size was added to the estimated sample size making the final sample size of 248.A systematic random sampling technique was used to recruit samples for the study in each day of the data collection process. The actual sampling fraction (kth) was calculated through dividing the total number of source population attending during the study period (540) by the corrected sample size (248). Thus, every other patient was interviewed after physician visit and his/her medical record was reviewed in the same day after the interview until the total sample size was reached. Six nurses who had taken a one day training regarding objective, relevance, confidentiality, respondent’s right, informed consent and techniques of interview for the study using the structured questionnaire prior to data collection were recruited for data collection. Data was collected using interview supported by structured questionnaire which was originally prepared in English then translated to the local language, Amharic which had two components. Part I: was aimed to collect information on basic sociodemographic variables. Part II: had consisted of questions required to gather information on the performance and frequency of SMBG.Maximum effort had been taken to maintain quality of data through the different steps like data entry, analysis, interpretation and representation. Incomplete questionnaires were excluded while completed were coded and entered in to Epi Data entry version 4.2.0. Then, it was exported to and analyzed by Statistical Package for the Social Sciences (SPSS) version 20.0 package. Socio demographic characteristics and clinical characteristics were summarized using frequency tables. Mean and standard deviation was calculated for continues data. Multivariate linear regression analysis was carried out to determine factors independently associated with SMBG with a p-value of less than or equal to 0.05 was considered as statistically significant.
ETHICAL ISSUES
Ethical clearance was granted by the ethical review committee of School of Pharmacy of Addis Ababa University and approved by ethical review board of SPHMMC.Prior to data collection, Children who were able to provide assent were requested along with consent from care takers while informed verbal consent was obtained from the study participants.
RESULTS
In the present study, a total of 247 T1DM patients were involved. Females comprised 135(54.7%)of the sex category. Majority of the patients were in the age group of 5-15 years, which accounted for 129(52.2%) and 192(77.7%) had formal educational back ground. Regarding the EDA membership, 134(54.3%) has a membership identification card.
SOCIO-DEMOGRAPHIC CHARACTERISTIC OF AMBULATORY T1DM PATIENTS ATTENDING TO DIABETIC CLINICS OF SPHMMC IN JUNE 01 TO AUGUST 01, 2017
Health related characteristics
Among participants of the study majority (61.5%) had a healthy weight, while only one patient was found with obese BMI. Regarding the duration of diabetes, 54 (21.9%) had insulin treatment history of less than one year, 130 (52.6%) have been laid between one and five years duration. Most 168(68%) of the respondents were taking both regular and Lente insulin (NPH) while 75(30.4%) were on Lente insulin (NPH) and 4(1.6%) were taking only regular insulin.
Clinical characteristics of ambulatory T1DM patients attending to diabetic clinics of SPHMMCinJune 01 to August 01, 2017
Assessment of SMBG level of the respondents revealed that out of the total 247 T1DM patients one hundred sixty-one (65.2%) of them were performed SMBG irrespective of the frequency. Out of those who performed SMBG level, one hundred fifty-two (61.5%) were monitored by themselves/families and nine (3.6%)were monitored with health care professional in addition to their regular follow up. But, about one third (34.8%) were monitored their blood glucose level with regular follow up at diabetic clinics of SPHMMC. Specifically, among the sub-total (161) respondents who had SMBG, 68(42.2%) patients were monitored blood glucose level three times daily by themselves/families with their glucometer. Again, among seventy-two (44.7%) patients who had monitored twice daily, 70(97.2%) were themselves/families and two (2.8%) respondents were monitored withhealth care professional. As shown, in figure1, ninety-two (49.7%) respondents were not monitored their blood glucose level even once weekly.
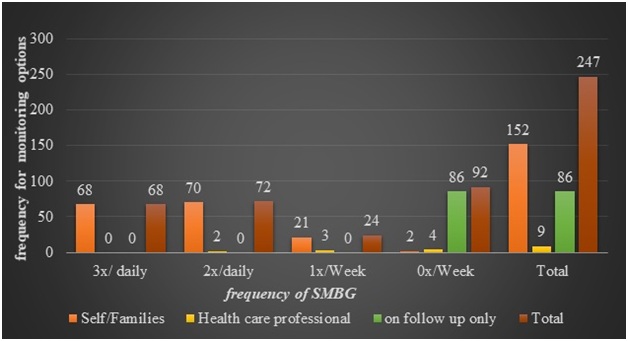 Figure 1: Blood glucose monitoring options versus frequency distribution of SMBG level among ambulatory T1DM patients attending to diabetic clinics of SPHMMC in June 01 to August 01, 2017.
Figure 1: Blood glucose monitoring options versus frequency distribution of SMBG level among ambulatory T1DM patients attending to diabetic clinics of SPHMMC in June 01 to August 01, 2017.
The multivariate analysis of this study was fitted and showed that gender, educational back ground and duration of DM since diagnosed had significant association with SMBG. Accordingly, male patients were nearly to 0.6 (AOR=0 .43, 95% CI :(0.23-0.80)) times less likely to perform SMBG compared to female patients. On the other hand, patients who had an educational back ground of primary school were about four and quarter (AOR=4.29,95%CI:1.24-14.90) times more likely preformed SMBG compare to those who were at university/college level. Shorter (5years).Multivariate logistic regression analysis results of factors associated with SMBG among ambulatory T1DM patients attending to diabetic clinics of SPHMMC in June 01 to August 01, 2017.
DISCUSSION
In this study, we also attempted to determine how patients with type 1 diabetes had been monitoring their blood glucose level. Thus, our study found that 65.2% of the patients were practiced SMBG in addition to their regular follow up. This is similar to what was found in USA (75% and 66%) and Norway (70%)[18-20].This might be due to the free glucometers and strips provided to majority of our study participants which made them comparable to T1DM patients in developed countries. However, SMBG found in this study was higher than what found in some studies in in Nigeria ranging from 11% to 47.8% and in Malaysia whereSMBG of 15.3% was reported [14, 21, 22]. This could be possible that, our clinics provided optimally better patient education on SMBG compared to the other studies carried out in government owned hospitals. On the other hand, two findings in Australia reported higher values (88.4% and 81.7%) of SMBG performance than what we found [23, 24]. This could be implies, patients in our studies had lack of motivation and knowledge in monitoring, fear of need and pain, unconducive work place which verified as barriers for self- monitoring by different quantitative and qualitative studies[22,25,26,27].
According to the ADA standard of SMBG level our study found less optimal than what isrecommended. Almost 57.8% of those who practiced SMBG performed less frequently than whatADA recommended (testing blood glucose three and above times daily). Inadvertently, this finding was in agreement with other studies which carried out in Nigeria and America [14,18,21,28].However, a France study reported about 42%, and a population based study in USA found only 7% of the participants performed SMBG level less frequently than the ADA recommendation which were better than this finding[10,29]. Based on our study, availability of glucometer with its test strips has a direct impact on the frequency of SMBG. Thus, cost of test strips and variance of participantsincluded in donation may be leads to inadequate presentation of SMBG.
Multivariate logistic regression analysis of this study showed that being female gender, participantwith primary level of education and shorter (<5 years) duration diabetes were significantlyassociated with SMBG performance. This was similar with other studies; whereby femalegenderwere frequently performed SMBG than males. In fact, our study indicated males were less performance of self-monitoring compared to females (58% verses 71%)[12,30].This could be suggested that, most male participants were away from home several days in a week. Thus, males had subjected to poor SMBG practice. Taken together, due tofewer studies conducted regarding to gender difference, relationship between gender and SMBG could not be adequately described. However, our results suggest that individual differences, such as gender, should be considered as a targeted outcome of interest for research or a consideration in clinical intervention.
Participants with primary level of education were also found to be another factor significantly associated with good performance of SMBG compared to higher educational level. This could be due to provision of free glucometer donation to this age group. However, good performance ofSMBG seems to be achieved in well-educated T1DM patients as it could be easy to understand theprocess of glucose testing and confident in their ability to carry out glucose testing [31].
Short duration of diabetes history (below 5 years) was also found to be independently associatedwith SMBG in this study. This could be possible that patients with short duration of diabetes hadsuffered with frequent hypoglycemia due to inexperience in the prevention and immediatemanagement of hypoglycemia. Therefore, patients with short duration of diabetes history could30able to develop the chance of fear for hypoglycemia and inadequate glycemic control which makethem to do there SMBG level regularly. However, other studies reported that performance ofSMBG had associated with long duration of diabetic. These evidences suggested that patients withlong diabetes duration had develop experience as they educated on SMBG over the years [14,22].Thus, these findings highlight the complex experience of engaging in SMBG and barriers to perform SMBG level. Individual patient factors might be extremely important in theexperience of SMBG. On the other hand, one survey indicated that socio-demographic variables are poor indicators to show the performance of SMBG. Thus, such variables are an unreliable tool to use in targeting patients for educational intervention in the area of SMBG [32].But, this study provides a clue for further studies to work out on the association of demographic characteristics of T1DM patients with performance of SMBG.
The cross-sectional nature of the study design prevents us from drawing causalinferences about the relationship between the chosen covariates and outcome variables. SMBG rates also might be misjudged. Therefore, further investigation of the reliability and validity of self-reported hypoglycemia and SMBG is needed. The study looked at only a single facility and hence caution should be well-thought-out in extrapolating the results. However, this study gave some useful insight into the magnitude of the hypoglycemia and SMBG approach among the study population and provides useful baseline information for consultative, comparative and future research purposes in the study center
This study has revealed that the performance of SMBG among patients attending tothe outpatient diabetic clinics of SPHMMC is suboptimal as at least one third of them were foundto be monitor their blood glucose level in follow up only to the clinics. Besides, less than 50% ofpatients who had practiced SMBG were not committed to perform as frequent as it recommendedin ADA. We also found factors associated with better performance of SMBG included female sex,primary level of education, shorter(≤5years) duration of diabetes. Majority of T1DM patients in SPHMMC did not follow guidelines of SMBG ≥3 times per day, despite glucose meters and strips being generally available at no cost to most of them. So, this study endorses the necessity of further support in performing SMBG and increased availability of other tools for glucose monitoring. We also advocate the inclusion of blood glucose meters, blood glucose test strips in health insurance program in Ethiopia to ease the burden of self- monitoring in diabetic patients.
ACKNOWLEDGEMENT
We want acknowledge the data collectors for their tireless effort in the data collection process. We also express our deepest gratitude for respondents giving their precious time during interview.
REFERENCES
- Benjamin EM (2002) Self-monitoring of blood glucose: the basics. Clinical diabetes 20:45-47.
- Skeie S, Kristensen GB, Carlsen S(2009) Self-monitoring of blood glucose in type 1 diabetes patients with insufficient metabolic control: Focused self-monitoring of blood glucose intervention can lower glycated hemoglobin A1C. Journal of diabetes science and technology3:83-88.
- Saudek CD, Derr RL, Kalyani RR(2006) Assessing glycaemia in diabetes using self-monitoring blood glucose and hemoglobin A1C. Jama 295:1688-1697.
- Parkin CG, Davidson JA (2009) Value of self-monitoring blood glucose pattern analysis in improving diabetes outcomes. Journal of diabetes science and technology 3:500-508.
- Dinsmoor RS (2014) Diabetes definitions. Diabetes self-management 3:46.
- American Diabetes Association. Standards of medical care in diabetes (2014) Diabetes care 37:14-80.
- Gonder-Frederick LA, Julian DM, Cox DJ, ClarkeWL (1998) Self-measurement of blood glucose: accuracy of self-reported data and adherence to recommended regimen. Diabetes Care 11:579-585.
- Minder AE, Albrecht D, Schäfer J, Zulewski H (2013) Frequency of blood glucose testing in well-educated patients with diabetes mellitus type 1: How often is enough. Diabetes research and clinical practice 101:57-61.
- Lecomte P, Romon I, Fosse S, Simon D(2008) Self-monitoring of blood glucose in people with type 1 and type 2 diabetes living in France: The Entred study 2001. Diabetes & metabolism 34:219-226.
- Karter AJ, Ferrara A, Darbinian JA (2000) Self-monitoring of blood glucose: Language and financial barriers in a managed care population with diabetes.Diabetes care 23: 477-483.
- Moström P, Ahlén E, Imberg H (2017) Adherence of self-monitoring of blood glucose in persons with type 1 diabetes in Sweden. BMJ Open Diabetes Research and Care 5: 000342.
- Ziegler R, Heidtmann B, Hilgard D (2011) DPVWissInitiative. Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatric diabetes 12:11-17.
- Edah JO, Odoh G, Kumtap CY (2016) Self-monitoring of blood glucose in Jos, Nigeria. Journal of Medicine in the Tropics 18:28.
- Cho NH, Shaw JE, Karuranga S(2018) IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes research and clinical practice 138:271-81.
- American Diabetes Association. Glycemic targets: Standards of medical care in diabetes. Diabetes Care (2018) Diabetes journal 41:55-64.
- IDF Diabetes Atlas 8th Edition - International Diabetes Federation.
- Karter AJ, Ferrara A, Darbinian JA (2000) Self-monitoring of blood glucose: Language and financial barriers in a managed care population with diabetes. Diabetes care 23:477-483.
- Adams AS, Mah C, Soumerai SB (2003) Barriers to self-monitoring of blood glucose among adults with diabetes in an HMO: a cross sectional study. BMC health services research 3:6.
- Kjome RL, Granas AG, Nerhus K (2010)The prevalence of self-monitoring of blood glucose and costs of glucometer strips in a nationwide cohort. Diabetes technology & therapeutics 12:701-705.
- Unachukwu CN, Young EE, Uchenna DI (2011) Self-blood glucose monitoring among diabetic patients in Port Harcourt, Nigeria. Afr J Diabetes Med 19:19-20.
- Wijesinha S. (2007) Self-monitoring of blood glucose among diabetes patients attending government health clinics. Med J Malaysia 62:147.
- Chubb SP, Van Minnen K, Davis WA (2011)The relationship between self-monitoring of blood glucose results and glycated hemoglobin in type 2 diabetes: TheFremantle Diabetes Study. Diabetes research and clinical practice 94:371-376.
- Bruce DG, Davis WA, Cull CA (2003) Diabetes education and knowledge in patients with type 2 diabetes from the community: The Fremantle Diabetes Study. Journal of Diabetes and its Complications 17:82-89.
- Snoek FJ, Malanda UL (2008) Self-monitoring of blood glucose: Psychological barriers and benefits 112-115.
- Nagelkerk J, Reick K, Meengs L (2006) Perceived barriers and effective strategies to diabetes self?management. Journal of advanced nursing 54:151-158.
- Hortensius J, Kars MC, Wierenga WS, Kleefstra N, Bilo HJG, et al. (2012) Perspectives of patients with type 1 or insulin-treated type 2 diabetes on self-monitoring of blood glucose: A qualitative study. BMC Public Health 12:167
- Harris MI, Cowie CC, Howie LJ (1993) Self-monitoring of blood glucose by adults with diabetes in the United States population. Diabetes care 16:1116-11123.
- Miller KM, Beck RW, Bergenstal RM (2013) T1D Exchange Clinic Network. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes care: 121770.
- Ward JE, Stetson BA, Mokshagundam SP (2015) Patient perspectives on self-monitoring of blood glucose: Perceived recommendations, behaviors and barriers in a clinic sample of adults with type 2 diabetes. Journal of Diabetes & Metabolic Disorders 14:43.
- Austin MM (2013) The two skill sets of self-monitoring of blood glucose education: The operational and the interpretive. Diabetes Spectrum 26:83-90.
- Vincze G,Barner JC, Lopez D (2004) Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. The Diabetes Educator 30:112-125.
Citation: Kahsay H, Tesfay D, Demoz GT,Araya H (2019) Evaluation of Self-Monitoring Blood Glucose Practice and Associated Factors among Type-1 Diabetic Patients at St.Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. J Diabetes MetabDisord 6:027.
Copyright: © 2019 Halefom Kahsay, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

