
Extra Articular Pelvic Fractures with Concomitant Gastrointestinal Injury Caused by Ballistic Trauma are Harbingers of Intra-Abdominal and Retroperitoneal Abscesses
*Corresponding Author(s):
Joao B Rezende-NetoDepartment Of Surgery, Division Of General Surgery, Trauma And Acute Care Service, St. Michael’s Hospital, University Of Toronto, Toronto, Canada
Tel:+1 4168645284,
Fax:+1 416864581
Email:rezendenetoj@smh.ca
Abstract
Introduction
Gastrointestinal (GI) injuries with associated pelvic fractures caused by ballistic trauma result in local contamination. Recent literature has suggested that irrigation and debridement may not be necessary despite GI contamination. Although this approach my not alter the incidence of osteomyelitis, there is a lack of evidence that irrigation and debridement of bone fragments could alter the incidence of retroperitoneal and intra-abdominal abscesses. We hypothesize that contaminated and devascularized bone fragments from Extra-Articular Pelvic Fractures (EAPF) can become a nidus of recalcitrant intra-abdominal and retroperitoneal infections. The goal of this study was to examine the outcomes of contaminated EAPF in ballistic trauma managed without local irrigation and debridement.
Methods
A 1-year prospective study of consecutive adult patients presenting to a Brazilian level 1 trauma center with abdominopelvic gunshot wounds and EAPF or GI injury that did not undergo operative debridement and washout of the soft tissue neighboring the fracture site. The main outcome measure was development of soft tissue infectious complication defined as peritoneal or retroperitoneal abscess.
Results
A total of 82 patients were divided into 3 cohorts: A) EAPF with an associated GI injury (n=32, 39%), B) EAPF with a urological injury or no associated GI or urological injury (n=21, 26%), and C) isolated GI injury without an associated EAPF (n=29, 35%). Overall, 14 patients (17%) developed an infectious complication, 11 patients from cohort A (34%), 1 patient from cohort B (5%), and 2 patients from cohort C (7%). The odds of developing an infectious complication in cohort A were 10.5 times higher compared to cohort B and 7.1 higher compared to cohort C. Cohort A was found to have significantly higher readmission rates and lengths of stay. Compared to other areas of the gastrointestinal tract, the odds of developing an infectious complication were 6 times greater for an injury to the rectum.
Conclusion
GI injuries with pelvic fractures caused by ballistic trauma are associated with up to 10 fold increase in retroperitoneal and intra-abdominal abscesses. Future studies are needed to investigate whether, during the trauma laparotomy to repair GI injuries, irrigation and debridement of devascularized bone fragments embedded in the soft tissue would decrease the incidence of post-operative infection.
Keywords
LIST OF ABBREVIATIONS
• GSW: Gunshot wound
• GI: Gastrointestinal
• EAPF: Extra-articular pelvic fracture
• ICU: Intensive Care Unit
• PRBC: Packed Red Blood Cells
• LOS: Length of Stay
• CT: Computed tomography
INTRODUCTION
Firearm injuries continue to be a major cause of morbidity and mortality worldwide, in both civilian and military populations [1,2]. As a result, the shared understanding amongst trauma surgeons with regards to the management of specific patterns of Gunshot Wounds (GSW) has grown and resulted in less aggressive operative strategies [3-5]. However, ballistic trauma to the abdominopelvic region is frequently associated with injuries to the Gastrointestinal (GI) tract that lead to contamination [4,6]. Therefore, a conservative management of the local contamination of associated pelvic fractures in this setting could potentially result in infectious complications.
Expedited surgical debridement and antimicrobial therapy are advocated for high velocity ballistic injuries to the pelvis with an intra-articular (i.e., acetabular, sacro-iliac joints) component [4-7]. This approach potentially decreases the risk of fulminant joint infection and subsequent chronic complications [4,6-8]. Although infectious complications in isolated pelvic fractures caused by low-velocity GSW are uncommon, concurrent injuries to the GI tract could potentially result in recalcitrant intra-abdominal and retroperitoneal infections, particularly in the presence of devitalized bony fragments and devascularized/injured soft tissue [6-8]. However, previous studies suggest that irrigation and debridement of Extra-Articular Pelvic Fractures (EAPF) caused by low-velocity GSW may not be necessary despite concomitant GI injury [8,9]. Although this approach my not alter the incidence of osteomyelitis, there is a lack of evidence that irrigation and debridement of bone fragments could alter the incidence of retroperitoneal and intra-abdominal abscesses. Contaminated bone fragments embedded in devascularized soft tissue can become a nidus of recalcitrant intra-abdominal and retroperitoneal infections [10-13]. The goal of this study was to examine the outcomes of contaminated EAPF in ballistic trauma managed without local irrigation and debridement. We hypothesized that patients who sustained GSW with concomitant EAPF and GI injury would have higher soft tissue infectious complication rates compared to patients without associated GI injuries.
METHODS
Setting
Inclusion and exclusion criteria
Exclusion criteria encompassed patients with isolated lumbar spine or pelvic fractures deemed to be intra-articular (i.e., acetabular fractures or those extending into the sacroiliac joints). Moreover, patients who were hemodynamically unstable on arrival, who required admission to the Intensive Care Unit (ICU), underwent damage control surgery, and those who underwent parenteral nutrition were excluded given possible association between hemorrhagic shock, peri-operative transfusion of blood products, with postoperative infection and immunomodulation [14]. Hemodynamic instability was defined as systolic blood pressure < 90mmHg and the necessity for transfusion of Packed Red Blood Cells (PRBC) or any other blood product.
Data collection and follow up
Our main outcome measure was the development of infectious complications defined as peritoneal or retroperitoneal abscesses confirmed by surgery, percutaneous drainage of the collection, or microbiology results of specimens. Patients were followed from the time of admission until hospital discharge, and had two study follow-up visits at 15 and 30 days post-discharge. Any suspicion of intra-abdominal or retroperitoneal infection, including discharge of purulent secretion through bullet wounds, prompted investigation with abdominal and pelvic Computed Tomography (CT) with intravenous, oral, and rectal contrast if indicated (Siemens Somatom Balance CT57, Berlin, Germany).
Statistical analysis
RESULTS
|
Cohort A (n=32) |
Cohort B (n=21) |
Cohort C (n=29) |
p-value |
|
|
Age in years, mean (SD) |
28±13.5 |
26±12.8 |
29±11.2 |
|
| Male sex | 29 (91) | 21 (100) | 28 (97) | 0.27 |
|
ISS, median (IQR) |
15 (9-18) |
9 (4-9) |
9 (8-16) |
<0.001 |
|
Infectious complication |
11 (34) |
1 (5) |
2 (7) |
0.004 |
|
Readmission |
6 (19) |
1 (5) |
0 (0) |
0.027 |
|
Mortality |
1 (3) |
0 (0) |
0 (0) |
0.46 |
|
All values to be completed as n (%) unless otherwise stated |
||||
Table 1: Patient characteristics.
Cohort A: Extra-Articular Pelvic Fractures (EAPF) with associated GI injury caused by ballistic trauma; Cohort B: EAPF without GI injury plus or minus urological injury caused by ballistic trauma; Cohort C: GI injury caused by ballistic trauma without associated EAPF.
Infectious complications
The mean length of time between the initial operation and the diagnosis of the infectious complication was 13.9 (±5.7) days. Every patient received appropriate antimicrobial therapy regardless of the management strategy. Of those with infectious complications, abscesses were percutaneously drained under ultra-sound or CT scan guidance in 57% (n=8) of patients. The remaining 6 patients underwent a laparotomy for abscess drainage, all of those patients belonged to cohort A. In all cases treated through a laparotomy, the abscess cavity contained purulent secretion, necrotic tissue and bone fragments (Figure 1 and Figure 2). Fluid collected from the abscesses of 7 patients was subjected to culture. The most frequent bacterial isolates were Escherichia coli, Staphylococcus aureus, and Enterococcus faecalis (Table 2).
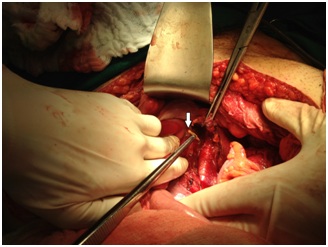 Figure 1: Intra-operative photograph depicting a displaced bone fragment (arrow) removed from an abscess cavity extending into the retro peritoneum in a cohort a patient (Extra-Articular Pelvic Fractures (EAPF) caused by ballistic trauma with associated GI injury).
Figure 1: Intra-operative photograph depicting a displaced bone fragment (arrow) removed from an abscess cavity extending into the retro peritoneum in a cohort a patient (Extra-Articular Pelvic Fractures (EAPF) caused by ballistic trauma with associated GI injury).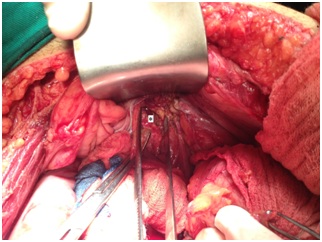 Figure 2: Intra-operative photograph of an abscess cavity (asterisk) extending into the retro peritoneum from a patient in cohort An Extra-Articular Pelvic Fractures (EAPF) caused by ballistic trauma with associated GI injury).
Figure 2: Intra-operative photograph of an abscess cavity (asterisk) extending into the retro peritoneum from a patient in cohort An Extra-Articular Pelvic Fractures (EAPF) caused by ballistic trauma with associated GI injury).|
Cohort A (n=32) |
Cohort B (n=21) |
Cohort C (n=29) |
|
|
Site of GI injury |
|
|
|
|
Stomach |
3 (9) |
- |
1 (3) |
|
Small bowel |
24 (75) |
- |
21 (72) |
|
Colon |
19 (59) |
- |
21 (72) |
|
Rectum |
14 (44) |
- |
2 (10) |
|
Bladder Injury |
6 (19) |
5 (23) |
2 (10) |
|
Site of pelvic fracture |
|||
|
Sacrum |
11 (34) |
3 (14) |
- |
|
Ilium |
16 (50) |
12 (57) |
- |
|
Pubis |
2 (6) |
3 (14) |
- |
|
Ischium |
3 (9) |
3 (14) |
- |
|
Coccyx |
2 (6) |
0 (0) |
- |
|
All values to be completed as n (%) unless otherwise stated |
|||
Table 2: Injury patterns.
Cohort A: Extra-Articular Pelvic Fractures (EAPF) caused by ballistic trauma with associated GI injury; Cohort B: EAPF caused by ballistic trauma without GI injury plus or minus urological injury; Cohort C: GI injury caused by ballistic trauma without associated EAPF.
Type of GI injury
There were no cases of leaks from GI anastomosis or suture repairs in any of the patients in cohorts A and C. Similarly, there were no bladder fistulas in patients who sustained bladder injuries in cohort B. A total of 12 patients in cohort A underwent a colostomy during the initial operation, 7 of them developed a pelvic abscess. One patient in cohort C underwent a colostomy and there were no complications. There were no colostomies performed in cohort B patients.
Readmission rates & length of stay
DISCUSSION
Our study prospectively documented intraabdominal and retroperitoneal infectious complications in patients with EAPF and had three main findings. Firstly, the odds of infectious complications in patients with EAPF and associated GI injuries (cohort A) was 10.5 times higher when compared to those with EAPF alone or with associated bladder injuries (cohort B, p=0.0312) and 7.1 times higher when compared to those with GI injuries without EAPF (cohort C, p=0.0494). These findings are in keeping with our hypothesis that the combination of contaminated and devascularized soft tissue with bone fragments displaced from pelvic fractures could become a nidus of intra-abdominal and retroperitoneal abscesses in the setting of gastrointestinal injuries. The lack of difference in the odds of abscess formation between cohorts B and C suggests that the combination of GI contamination and EAPF was a key factor (OR 1.48, 95% CI 0.13-17.50, p=0.755). Moreover, abscess fluid culture bacterial isolates from cohort A also suggest that the primary source of contamination was from the gastrointestinal tract (Table 3).
|
Bacterial isolate |
Cohort A |
Cohort B |
Cohort C |
|
Escherichia coli |
5 |
0 |
1 |
|
Staphylococcus aureus |
3 |
1 |
0 |
|
Enterococcus faecalis |
2 |
0 |
1 |
|
Proteus mirabilis |
1 |
0 |
0 |
Table 3: Abscess fluid culture isolates.
Cohort A: Extra-Articular Pelvic Fractures (EAPF) caused by ballistic trauma with associated GI injury; Cohort B: EAPF caused by ballistic trauma without GI injury plus or minus urological injury; Cohort C: GI injury caused by ballistic trauma without associated EAPF. All patients in cohort A and C had concomitantly 2 or more bacterial isolates in every culture. Fluid cultures were performed in the microbiology laboratory of the Risoleta Tolentino Neves Hospital.
The second main finding of our study was that patients in cohort A with rectal injuries were 6 times more likely to develop an infectious complication than patients with an injury in another location of the GI tract. The anatomical locations of the colon and the rectum render these organs more susceptible to injuries in ballistic pelvic trauma. In our series, only the small bowel was injured more frequently. In general, the complication rate of traumatic rectal injuries is greater than 50% and septic related complications occur in approximately 15% of the patients. It has been well documented in previous studies that the incidence of abscess formation in penetrating abdominal/pelvic trauma with multivisceral injuries increases with concomitant colorectal injury [15,16]. Comparably, our results showed that the odds infectious complications were also augmented with concurrent rectal injuries. This notion was further supported by the results of the abscess fluid culture isolates in our study.
Lastly, patients who developed infectious complications had significantly higher readmission rates and longer hospital lengths of stay. Previous studies have shown an association between infectious complications in trauma patients with a more prolonged stay in the hospital [14,17,18]. Although extended stay in hospital can be linked to several factors, the higher readmission rate in our study population was directly linked to the formation of intra-abdominal and retroperitoneal abscesses.
Our findings show that given the higher likelihood of soft tissue infectious complications and its associated prolonged length of stay and readmissions, the rationale for local debridement and washout of these injuries seems logical. Nonetheless, this approach remains poorly defined mainly because previous studies were limited by three important factors: retrospective nature, small sample size, and large variability in patient population and surgical management. We compiled data obtained from contemporary publications to validate those limitations. Our analysis revealed that in those studies only 37 patients’ unequivocally sustained injuries to the GI tract with concurrent EAPF caused by ballistic trauma [9,19-21]. The studies by Watters J, et al. and Muhdi S, et al. describe a total of 10 patients who underwent debridement and or washout of contaminated tissue and fracture site, none of them developed an infection. An additional seven patients in the studies by Bartkiw MJ, et al. and Demirbas S, et al. underwent similar procedure, only one patient developed local infection. Collectively in those studies, 20 patients with GI tract injury and concurrent EAPF caused by ballistic trauma did not undergo debridement or washout, 5 of those patients developed local infection [9,19-21]. An additional retrospective study by Rehman S, et al., showed no cases of intra-abdominal or retroperitoneal abscesses postoperatively in patients who underwent laparotomy for repair of GI injury with concurrent EAPF caused by ballistic trauma [8]. According to this study, however, washout of the contaminated area was performed at the discretion of the surgeon. Therefore, the actual role of debridement and washout of those injuries cannot be determined by their results. Moreover, data pertaining to the clinical condition of the patients and the severity of the injuries were not reported [8]. Lastly, in a more recent systematic review of 58 articles pertaining to debridement practices in gunshot-induced fractures the authors conclude that EAPF with bowel injury have conflicting evidence for debridement [7]. The authors of that study did not recommend for or against washout and debridement of gunshot-induced EAPF with bowel injury given the limited number of studies on this topic, and concluded that prospective trials for extensive versus superficial debridement of bowel-contaminated ballistic fractures are needed [7].
Our study has a series of limitations. This was a prospective observational study; we are not able to ascertain if washout and debridement of the area of the fracture and adjacent tissue can potentially reduce the rate of abscess formation postoperatively. However, our findings support additional investigation into the role of this approach. Secondly, this was a single-centre trial and results may not be extrapolated to all centers. Lastly, our sample was limited to patients without hemodynamic instability on arrival; thus, findings may not be extrapolated to all patients with trans-cavitary GSW. The rationale of excluding hemodynamically unstable patients was to reduce confounding risk factors for infection (i.e., received blood products, required intensive care unit admission, and underwent damage control procedures). Hence, the incidence of abscesses reported herein can be primarily attributed to local factors at the site of the injury involving contaminated devascularized soft tissue and bone fragments displaced from pelvic fractures.
CONCLUSION AND IMPLICATIONS
Gastrointestinal and colon injuries with concomitant pelvic fractures caused by ballistic trauma are associated with up to 10 fold increase in retroperitoneal and intra-abdominal abscesses. Future studies are needed to investigate whether, during the trauma laparotomy to repair GI injuries, irrigation and debridement of devascularized bone fragments embedded in the soft tissue would decrease the incidence of post-operative infection.
STATEMENT
- Consent to Publish was obtained from all patients involved in this study as per study protocol registration number: CAAE 39504714.3.0000.5149. Registered October 1, 2010. A copy of the consent form is available upon request
- Ethics Approval: approved by the Research Ethics Committee of the Risoleta Tolentino Neves Hospital (Belo Horizonte, Brazil), and was in accordance with research ethics resolution number 196/96 of the Brazilian Ministry of Health. Study Registration: CAAE 39504714.3.0000.5149. Registered October 1, 2010
- Study Registration: CAAE 39504714.3.0000.5149. Registered October 1, 2010
REFERENCES
- Gun violence in the United States (2016) A call to action. J Trauma Acute Care Surg 80: 847-848.
- Kalesan B, Mobily ME, Keiser O, Fagan JA, Galea S (2016) Firearm legislation and firearm mortality in the USA: a cross-sectional, state-level study. Lancet 387:1847-1855.
- Ball CG (2014) Current management of penetrating torso trauma: nontherapeutic is not good enough anymore. Can J Surg. 57: 36-43.
- Navsaria PH, Edu S, Nicol AJ (2011) Nonoperative management of pelvic gunshot wounds. Am J Surg. 201: 784-788.
- Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, et al. (2010) Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 68: 721-733.
- Miller AN, Carroll EA, Pilson HT (2013) Transabdominal gunshot wounds of the hip and pelvis. J Am Acad Orthop Surg 21: 286-292.
- Sathiyakumar V, Thakore RV, Stinner DJ, Obremskey WT, Ficke JR, et al. (2015) Gunshot-induced fractures of the extremities: a review of antibiotic and debridement practices. Curr Rev Musculoskelet Med. 8: 276-289.
- Rehman S, Slemenda C, Kestner C, Joglekar S (2011) Management of gunshot pelvic fractures with bowel injury: is fracture debridement necessary? J Trauma 71: 577-581.
- Watters J, Anglen JO, Mullis BH (2011) The role of debridement in low-velocity civilian gunshot injuries resulting in pelvis fractures: a retrospective review of acute infection and inpatient mortality. J Orthop Trauma 25:150-155.
- Najibi S, Matta JM, Dougherty PJ, Tannast M (2012) Gunshot wounds to the acetabulum. J Orthop Trauma. 26: 451-459.
- Poret HA 3rd, Fabian TC, Croce MA, Bynoe RP, Kudsk KA (1991) Analysis of septic morbidity following gunshot wounds to the colon: the missile is an adjuvant for abscess. J Trauma. 31:1088-1094.
- Cornwell EE 3rd, Dougherty WR, Berne TV, Velmahos G, Murray JA, et al (1999) Duration of antibiotic prophylaxis in high-risk patients with penetrating abdominal trauma: a prospective randomized trial. J Gastrointest Surg. 3: 648-653.
- Velmahos G, Demetriades D (1994) Gunshot wounds of the spine: should retained bullets be removed to prevent infection? Ann R Coll Surg Engl. 76: 85-87.
- Papia G, McLellan BA, El-Helou P, Louie M, Rachlis A, et al. (1999) Infection in hospitalized trauma patients: incidence, risk factors, and complications. J Trauma 47: 923-927.
- Rush DS, Nichols RL (1986) Risk of infection following penetrating abdominal trauma: a selective review. Yale J Biol Med. 59: 395-401.
- Blackwood JM, Hurd T, Suval W, Machiedo GW (1988) Intra-abdominal infection following combined spleen-colon trauma. Am Surg. 54: 212-216.
- Fabian TC (2002) Infection in penetrating abdominal trauma: risk factors and preventive antibiotics. Am Surg. 68: 29-35.
- Dellinger EP, Oreskovich MR, Wertz MJ, Hamasaki V, Lennard ES (1984) Risk of infection following laparotomy for penetrating abdominal injury. Arch Surg. 119:20-27.
- Muhdi MM, Hamdam TA (2003) Marginal wedge resection for chronic osteomyelitis of the iliac bone. Int Orthop. 27: 254-256.
- Bartkiw MJ, Sethi A, Coniglione F, Holland D, Hoard D, et al (2010) Civilian gunshot wounds of the hip and pelvis. J Orthop Trauma. 24: 645-652.
- Demirba? S1, Yildiz M, Uluutku AH, Kalemo?lu M, Kurt Y, et al. (2004) Surgical treatment of ano-rectal gunshot injuries caused by low-velocity bullets. Ulus Travma Acil Cerrahi Derg 10:17-21.
Citation: Rezende-Neto JB, De Abreu RNES, Gomez D, Tanoli OS, Campos VM, et al. (2019) Extra Articular Pelvic Fractures with Concomitant Gastrointestinal Injury Caused by Ballistic Trauma are Harbingers of Intra-Abdominal and Retroperitoneal Abscesses. J Emerg Med Trauma Surg Care 6: 027.
Copyright: © 2019 Joao B Rezende-Neto, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

