
Fahr Syndrome and Dysparathyroidism
*Corresponding Author(s):
Chadli ADepartment Of Endocrinology Diabetes And Metabolic Diseases, Ibn Rochd Hospital, Casablanca, Morocco
Tel:+212 661092820,
Email:drachadli@gmail.com
Abstract
Fahr Syndrome (FS) is a rare clinicopathological syndrome defined by the presence of bilateral and symmetrical intracerebral calcifications, usually associated with hypoparathyroidism. We report seven cases of FS with hypoparathyroidism. Mean age was 36 years. There were five women and two men. Famial history of FS was found in one case. Clinical manifestations included: seizures (n=5), cognitive impairment (n=4), tetany (n=4), epileptic disorder (n=1), extrapyramidal symptoms (n=1), psychiatric disorders as schizophrenia (n=1). We found a cataract in 6 patients. One patient had postpartum hemorrhage due to uterine atony. Etiologies were dominated by primary idiopatic hypoparathyroidism (n=5), secondary hypoparathyroidism after a total thyroidectomy (n=1), and familial pseudo-hypoparathyroidism (n=1). Treatment was based on calcium and vitamin D therapy (alfacalcidiol) associated to a symptomatic treatment leading to seizures regression, but persistence of calcifications and cognitive impairment disorders.
INTRODUCTION
Fahr Syndrome (FS), as defined by Theodor Fahr in 1930, is a rare clinicopathological syndrome, defined by the presence of bilateral and symmetrical intracerebral calcifications [1]. It is usually associated to a phosphorcalcic metabolism disorder. Hypoparathyroidism is the most common etiology. A combination of FS with hyperparathyroidism or a pseudohypoparathyroidism was more rarely reported [2].
The physiopathology of intracerebral calcifications is poorly understood and probably multifactorial. Most authors incriminate anoligoglial cells metabolic disorder with deposits of mucopolysaccharides and occurrence of secondary vascular lesions [3].
We report seven cases of F-Sand describe clinical, etiological and therapeutic features.
MATERIAL AND METHODS
We describe retrospectively seven cases of FS observed over a period of seven years (2008 to 2015). Were included patients who had basal ganglia calcifications on CT scan and primary or secondary hypoparathyroidism. Cognitive impairment evaluation was based on Mini Mental State Examination (MMSE) in 3 patients; it was subjectively evaluated in the other cases.
RESULTS
Mean age was 36 years. There were five women and two men. We found a familial history of FS in one case (Table 1). Clinical manifestations included: seizures (n=5), cognitive impairment (n=4), tetany (n=4), epileptic disorders (n=1), extrapyramidal symptoms (n=1), psychiatric disorders as schizophrenia (n=1). We found a cataract in 6 patients. One patient had postpartum hemorrhage due to uterine atony.
Calcifications of basal ganglia were found in all patients CT scans. Few patients had also subcortical and cerebellar calcifications (Table 1; Figures 1 and 2).
 Figure 1:Calcifications of the basal ganglia.
Figure 1:Calcifications of the basal ganglia.
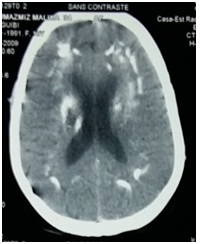 Figure 2: Calcifications of the parenchyma.
Figure 2: Calcifications of the parenchyma.
| Sex | Age (Year) | Time of Evolution Years | Clinical-Features | Ca Rate (mg/l) | Ph Rate (mg/l) | PTH (pg/ml) | CT Scan | Etiology | Therapy | |
| Case 1 | F | 36 | 31 | Seizures and tetany Mild cognitive impairment | 60 | 50,4 | 1,2 | Basal ganglia, periventricular and subcortical calcifications | HPT | Calcitherapy and vitamin D atypical neuroleptic Antiepileptic (SV) |
| Case 2 | M | 47 | 1 | Generalized seizures Muscle cramps Appendages disorders | 44 | 72 | 63 | Basal ganglia calcifications | HPT | Calcitherapy and vitamin D Antiepileptic (VS) |
| Case 3 | M | 30 | 10 | Partial seizures Bone pain Paresthesia | 46 | 45 | 174 | Basal ganglia and subcortical calcifications | PHPT | Calcitherapy and vitamin D Antiepileptic (CBZ) |
| Case 4 | F | 26 | 1 | Behavioral disorders Extra pyramidal syndrome Cognitive impairment Seizures and tetany Candidiasis and skin pustulosis | 39 | 80 | 10 | Basal ganglia calcifications | HPT | Calcitherapy and vitamin D Antiepileptic (SV) Neuroleptic |
| Case 5 | F | 31 | NM | Tetany Deafness Severe cognitive impairment Growth and puberty delay | 59 | NM | NM | Basal ganglia calcifications Cerebellar subcortical occipital calcifications | HPT | Calcitherapy and vitamin D Antiepileptic (SV) |
| Case 6 | F | 50 | 1 month | Generalized seizures Tetany | 54 | NM | NM | Basal ganglia and subcortical calcifications | HPT post thyroidectomy (3 years) | Calcitherapy and vitamin D Antiepileptic (SV) |
| Case 7 | F | 33 | 1 week | Postpartum Hemorrhage due to uterine atony Delirium, delusions Mild cognitive impairment | 43 | 60 | 3,82 | Basal ganglia calcifications | HPT | Calcitherapy and vitamin D |
Table 1: Clinical, biological, therapeutic and outcomes of different cases.
Ca: Calcium, CBZ: Carbamazepine, HPT: Hypoparathyroidism, NM: Not Mentioned, Ph: Phosphore, PHPT: Pseudo Hypoparathyroidism, PTH: Parathyroid Hormone, SV: Sodium Valproates
Mean calcium level in blood was 49 mg/l, the parathyroid hormone rate was low in 6 patients ((
Etiologies were dominated by primitiveidiopatic hypoparathyroidism in 5 patients, secondary hypoparathyroidism after a total thyroidectomy in one patient, and familial pseudo-hypoparathyroidism in one patient.
Treatment was based on calcium (carbonate of calcium) and vitamin D therapy (alfacalcidiol). Symptomatic treatment was indicated in all cases: antipsychotics and / or anti epileptic therapy, none of our patient had subcutaneous parathormone or lithium therapy. At follow up, all patients had clinical and biological monitoring (calcium, urinary 24h calcium). We noticed, at the follow up, a regression of seizures in all cases, but persistence of calcifications patients and cognitive impairment disorders.
DISCUSSION
Fahr Syndrome is a rare clinicopathological syndrome [1]. Its clinical symptoms may include: Neuropsychiatric disorders such as personality disorders and / or behavior, confusional or delirious syndrome, cognitive disorders, extrapyramidal syndrome as observed in one of our patients. Partial or generalized seizures can also happen in FS, rarely cerebellar or pyramidal syndrome, cranial nerves impairment and chorea [4]. Usually psychiatric manifestations precede neurologic symptoms [5]. And more rarely FS may remain asymptomatic [4].
A variety of conditions can cause intracerebral calcification: endocrinedisorders, infectious diseases, degenerative or systemic diseases and tumors. In these cases, the calcifications are not bilateral, symmetric or localized to the basal ganglia as observed in FS [6]. Idiopathic FS is called Fahr’s disease, especially if there is a familial history consistent with autosomal dominant inheritance [7].
Hmami F [8] reported 5 cases of adolescence-onset epilepsy with unsuccessful antiepileptic therapy, who had hypoparathyroidism in three cases and pseudohypoparathyroidism in the other two. The patients were treated with oral calcium and active vitamin D (1-alphahydroxy vitamin D3). Seizure frequency progressively decreased and serum calcium levels returned to normal. Seizures were the most commonly symptoms found in our patients.
Yurekli et al. [9] diagnosed a case presenting with dementia, and observed a reduction in the dementia symptoms after treatment.
Simone et al. [10] reported a case of a 69-year-old male with repeated episodes of transient loss of consciousness and minimal cognitive and behavioural disturbances. With a diagnosis of pseudo hypoparathyroidism, whose correction led to a significant clinical improvement. Unfortunately we hadn’t similar results.
Prescribing thiazide diuretic may be helpful by increasing serum calcium without causing hypercalcaemia. Subcutaneous administration of synthetic parathormone also can significantly reduce calcium and vitamin D intake and hypercalciuria, but it is not permitted for this indication currently.
Hypomagnesemia must be systematically investigated and corrected in all cases so that the calcium and vitamin D treatment can be effective [7].
Other pharmacological treatments, such as clonazepam and atypical antipsychotics (quetiapine), can be useful to improve anxiety, depression and obsessive compulsive disorders and can also reduce dystonia. One of our patient’s had quetiapine with an improvement of movement disorders.
Lithium should be provided carefully because it can increase seizures risk in patients with FS [11].
CONCLUSION
Fahr syndrome is a rare entity which is not overlooked. There is an agreement that FS must be considered in the diagnosis of patients displaying nonspecific neuropsychiatric symptoms accompanied by calcium metabolism disorders in order to allow an appropriate treatment and to prevent high morbidity neurological damage.
REFERENCES
- Chevalier D, Marie I, Tillon J, Lévesque H (2005) [A cause of cerebral calcifications not to be ignored: Fahr syndrome]. Rev Med Interne 26: 668-670.
- Khammassi N, Chrifi J, Mohsen D, Abdelhedi H, Tougourti MN, et al. (2010) [Fahr’s syndrome: two case report]. Rev Neurol (Paris) 166: 446-450.
- Younes-Mhenni S, Thobois S, Streichenberger N, Giraud P, Mousson-de-Camaret B, et al. (2002) [Mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes (Melas) associated with a Fahr disease and cerebellar calcifications]. Rev Med Interne 23: 1027-1029.
- Gulsun M, Baykiz AF, Kabatas S, Belli H (2006) Fahr’s Syndrome - Three cases presenting with psychiatric signs. Eur J Gen Med.
- Rafai MA, Oumari S, Lytim S, Boulaajaj FZ, Moutawakkil BE, et al. (2014) Le syndrome de Fahr: aspects cliniques, radiologiques et étiologiques. Feuillets de Radiologie 54: 2-8.
- Sobrido MJ, Geschwind DH (2003) Genetics of Familial Idiopathic Basal Ganglia Calcification. Genetics of Movement Disorders.
- Boulanger H, Ahriz Saksi S, Chhuy F, Flamant F (2013) Hypocalcémie. EM Consulte, AKOS, Traité de Médecine.
- Hmami F, Chaou-ki S, Benmiloud S, Souilmi FZ, Abourazzak S et al. (2014) Seizures revealing phosphocalcic metabolism abnormalities. Rev Neurol (Paris) 170: 440-444.
- Yürekli V, Gündogar D, Özcankaya R (2007) A rare cause for dementia: Fahr disease. Süleyman Demirel University, Department of Medicine Journal 14: 32-34.
- Simone O, Tortorella C, Antonaci G, Antonaci S (2008) [An unusual case of transient loss of consciousness: the Fahr’s syndrome]. Recenti Prog Med 99: 93-96.
- Chaudhari D, Renjen PN (2015) Fahr’s disease: A rare neurological disease. Apollo Medicine 12: 148-151.
Citation: Benassila FZ, El Aziz S, Chadli A (2016) Fahr Syndrome and Dysparathyroidism. J Diabetes Metab Disord 3: 015.
Copyright: © 2016 Benassila FZ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

