
Implementation of a Simplified Pediatric Peri-Appendectomy Antibiotic Regimen
*Corresponding Author(s):
Christina M ShantiDepartment Of Surgery, Division Of Pediatric Surgery, Children's Hospital Of Michigan/Wayne State University, Detroit, MI, United States
Tel:+1 3137455838,
Email:CShanti@dmc.org
Abstract
Background: Appendicitis is a common reason for emergency surgery in children. Treatment includes appendectomy and antibiotics. Our 3-antibiotic regimen was complex and consumed significant resources. To improve efficiency and costs, we transitioned to once-daily 2-antibiotic regimen and compared safety, efficacy, and costs in complicated and uncomplicated pediatric appendicitis.
Methods: A retrospective chart review for pediatric patients undergoing appendectomy in 2016. Variables included demographics, post-operative diagnosis, infections, antibiotics, nursing resources, and antibiotic costs. Patients treated in the first 6 months received the traditional antibiotic regimen. Those treated in the last 6 months received the new antibiotic regimen.
Results: 112 patients underwent appendectomy in the first 6 months and 78 in the second 6 months. We found no difference in post-operative infections. Nursing time and costs were significantly lower with the new regimen in complicated (p<0.001) and uncomplicated appendicitis (p<0.003).
Conclusions: A simplified peri-appendectomy antibiotic regimen was as effective with fewer nursing resources and treatment costs.
Introduction
Acute appendicitis is the most common cause of emergency surgical intervention in the pediatric population [1]. With a lifetime risk of 8.6% in men and 6.7% in women [2], the incidence peaks during childhood, particularly between the ages of ten and eleven years [3]. Antibiotic therapy and appendectomy are considered the standard of care for patients with appendicitis. Patients with uncomplicated appendicitis typically receive a single dose of antibiotics at the time of diagnosis, while those with complicated appendicitis require a longer course [4]. There is great debate surrounding the optimal antibiotic regimen for appendicitis and therefore significant variability among surgeons [5, 6]. Historically, a 3-drug regimen of ampicillin, gentamicin, and clindamycin has been preferred for its broad-spectrum coverage [7]. While these antibiotics are relatively inexpensive, their combination requires multiple daily doses and laboratory monitoring. In contrast, some surgeons now opt for a 2-drug regimen consisting of once daily dosing of ceftriaxone and metronidazole, proposing that it is as effective while also being more cost effective and less labor intensive for the patients, hospital, and caregivers [3, 8]. However, these claims have not been formally studied in uncomplicated appendicitis and often the extent of infection is not known until post-operatively, after antibiotics have been started. Additionally, the associated risk of certain complications, such as Clostridium difficile (C-Diff)-associated colitis has not been studied. [9]. Our study investigates the rate of post-operative infectious complications, resource utilization, and cost of both antibiotic regimens in children with uncomplicated and complicated appendicitis at our institution.
Materials and Methods
A retrospective chart review was conducted for all patients under the age of 18 years undergoing appendectomy at Children’s Hospital of Michigan from January 1, 2016 to December 31, 2016. Variables collected include demographics, prior evaluation at an outside hospital, length of stay, need for readmission, post-operative diagnosis, antibiotic regimen, postsurgical infections, Clostridium difficile colitis, estimated nursing time needed for antibiotic administration, and cost of antibiotics. The cost of antibiotics was obtained from the patient’s hospital bills and reflects charges to the patient. Prior to July 1st patients with appendicitis were treated with the triple intravenous antibiotic regimen of ampicillin, gentamicin, and metronidazole. Patients treated on or after July 1st were treated with a once daily regimen of ceftriaxone and metronidazole. Statistical analyses were performed with GraphPad Prism v8.0.2 to assess correlations between antibiotic regimen, clinical outcomes, and resource utilization in both groups.
Results
There were 190 patients who met inclusion criteria. Of those, 112 appendicitis patients (67 uncomplicated and 45 complicated) received the triple antibiotic regimen and 78 patients (42 uncomplicated and 36 complicated) received the double antibiotic, once daily dosing regimen. The larger number of patients in the first group may relate to previously described seasonal variation in appendicitis, being more common in the spring and summer seasons than fall and winter (Deng Y). There were no differences in the demographics of patients in either group (table 1).
|
|
Old Regimen (117 Pts) |
New Regimen (75 Pts) |
|
Age (mean) (years) |
10.4 |
10.4 |
|
% Male |
63 |
50 |
|
% Transfer from Outside Hospital |
26 |
26 |
|
Length of Stay (mean) (days) |
2.9 |
3.5 |
|
Length of Stay – Complicated (mean) (days) |
4 |
5 |
|
Length of Stay – Uncomplicated (mean) (days) |
2.16 |
1.95 |
|
% Complicated Appendicitis |
40 |
44 |
Table 1: Demographics. Old regimen = ampicillin, gentamycin, metronidazole; New regimen = once daily ceftriaxone, metronidazole
As expected, the hospital length of stay was longer for the patients with complicated appendicitis compared to those with uncomplicated appendicitis (Table 1). There was no significant difference in the length of stay between the two antibiotic groups whether they were diagnosed with complicated or uncomplicated appendicitis (Table 1). Patients with complicated appendicitis received more doses of antibiotics (mean: 21 doses) compared to those with uncomplicated appendicitis (mean: 7 doses). Nursing time requirements for those with complicated appendicitis averaged 614 minutes compared to an average of 215 minutes for uncomplicated appendicitis. The cost of antibiotic administration was also much higher for patients with complicated compared to uncomplicated appendicitis ($2336.95 vs. $986.99 respectively).
Nursing time required for antibiotic administration was significantly lower in the new regimen group for both complicated (-798 minutes, p<0.001) and uncomplicated appendicitis (-214 minutes, p=0.003) (Figure 1).
In addition, the cost of antibiotics was significantly lower with the new regimen for both complicated (-$2,223, p<0.001) and uncomplicated appendicitis groups (-$1,008 p<0.001) (Figure 2).
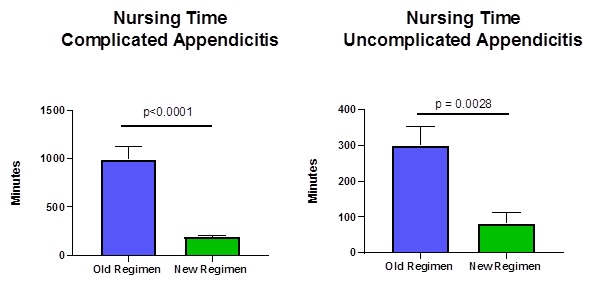 Figure 1: Nursing time (minutes) spent with patients with uncomplicated and complicated appendicitis in old versus new antibiotic regimens (p ≤ 0.05). Old regimen = ampicillin, gentamicin, metronidazole; New regimen = once daily ceftriaxone, metronidazole
Figure 1: Nursing time (minutes) spent with patients with uncomplicated and complicated appendicitis in old versus new antibiotic regimens (p ≤ 0.05). Old regimen = ampicillin, gentamicin, metronidazole; New regimen = once daily ceftriaxone, metronidazole
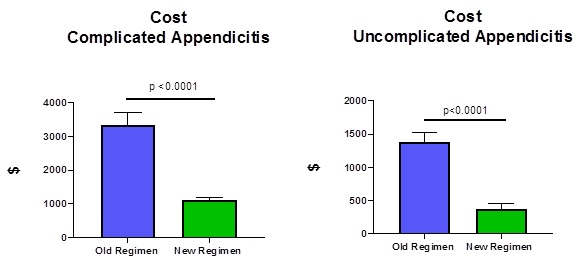 Figure 2: Cost of antibiotic therapy in patients with uncomplicated and complicated appendicitis in old versus new antibiotic regimens (p ≤ 0.05). Old regimen = ampicillin, gentamicin, metronidazole; New regimen = once daily ceftriaxone, metronidazole
Figure 2: Cost of antibiotic therapy in patients with uncomplicated and complicated appendicitis in old versus new antibiotic regimens (p ≤ 0.05). Old regimen = ampicillin, gentamicin, metronidazole; New regimen = once daily ceftriaxone, metronidazole
Infectious complications were rare in both groups. A surgical wound infection occurred in only 1 patient while 13 patients developed a deep space infection post-operatively (Table 1). There were no statistically significant differences in the rates of surgical site infections, Clostridium difficile colitis, deep space infections, or readmission rates between the two groups (Table 2).
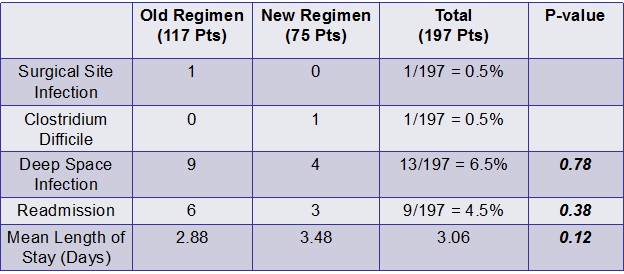 Table 2: Incidence of postsurgical complications in patients receiving the old antibiotic regimen and the new antibiotic regimen.
Table 2: Incidence of postsurgical complications in patients receiving the old antibiotic regimen and the new antibiotic regimen.
Discussion
Our study found that a simplified antibiotic regimen had similar efficacy and complication rates for pediatric patients with complicated and uncomplicated appendicitis, while lowering costs and nursing time requirements. These differences were even greater in patients diagnosed with complicated compared to non-complicated appendicitis.
Infectious complications were rare in all groups. The antibiotic regimen used had no impact on post-operative infectious complications, length of hospital stay, or readmission rate. This single daily dose regimen of ceftriaxone and metronidazole can be used for pediatric patients with complicated or uncomplicated appendicitis to decrease resource requirement and cost during hospitalization. This allowed us to standardize antibiotics for all patients with appendicitis pre-operatively and adjust the length of the antibiotic course after surgery based on the operative findings.
Conclusion
A simplified once daily, 2-antibiotic regimen for pediatric appendicitis was as effective and safe as the traditional 3-drug regimen while requiring less nursing time and lowering costs. These benefits are amplified in complicated appendicitis.
References
- Pearl RH (1995) Pediatric appendectomy. J Pediatr Surg, 30: 173-8, discussion 178-81.
- Ein SH, A Nasr, A Ein (2013) Open appendectomy for pediatric ruptured appendicitis: a historical clinical review of the prophylaxis of wound infection and postoperative intra-abdominal abscess. Can J Surg, 56: 7-12.
- Peter SDS, Tsao K, Spilde TT, Holcomb GW, Sharp SW et al (2008) Single daily dosing ceftriaxone and metronidazole vs standard triple antibiotic regimen for perforated appendicitis in children: a prospective randomized trial. J Pediatr Surg, 43: 981-5.
- Bi LW, Yan BL, Yang QY, Cui HL (2019) Comparison of conservative treatment with appendectomy for acute uncomplicated pediatric appendicitis: a meta-analysis J Comp Eff Res, 8: 767-780.
- Nadler EP, Reblock KK, Ford HR, Gaines BA (2003) Monotherapy versus multi-drug therapy for the treatment of perforated appendicitis in children. Surg Infect (Larchmt), 4: 327-33.
- Higginbotham P, A Gottlieb (1998) Improving care with a pediatric appendicitis pathway. Nurs Case Manag, 3: 26-35.
- Lund DP, Murphy EU (1994) Management of perforated appendicitis in children: a decade of aggressive treatment. J Pediatr Surg, 29: 1130-3; discussion 1133-4.
- Bonadio W, Rebillot K, Ukwuoma O, Saracino C, Iskhakov A et al (2017) Management of Pediatric Perforated Appendicitis: Comparing Outcomes Using Early Appendectomy Versus Solely Medical Management. Pediatr Infect Dis J, 36: 937-941.
- Sanders NL, Bollinger RR, Lee R, Thomas S, Parker W et al (2013) Appendectomy and Clostridium difficile colitis: relationships revealed by clinical observations and immunology. World J Gastroenterol, 19: 5607-14.
Citation: Shanti CM, Ridelman E, Veenstra MA (2021) Implementation of a Simplified Pediatric Peri-Appendectomy Antibiotic Regimen. J Emerg Med Trauma Surg Care 8: 061.
Copyright: © 2021 Michelle A Veenstra, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

