
Unplanned Reoperation and Interventional Radiology Post Appendicectomy: A Meta-Analysis
*Corresponding Author(s):
Michael SugrueDonegal Clinical Research Academy And Department Of Surgery Letterkenny University Hospital, Donegal, Ireland
Tel:+353 74 91 88823,
Fax:+353 74 91 88816
Email:michael.sugrue@hse.ie
Abstract
Introduction: Optimizing delivery of care to patients with appendicitis as part of an emergency general surgery care program is important. Appendicitis is one of commonest emergency surgical presentations and has significant potential morbidity and occasional mortality. Meta-analysis of reinterventions following appendicectomy has not been published. This meta-analysis evaluated the prevalence and potential predictors of reoperation and interventional radiological (IR) procedures post appendicectomy.
Methods: A PROSPERO-registered (ID CRD42017069040) meta-analysis following PRISMA guidelines using databases PubMed and Scopus for studies between June 2012 to May 2017 was undertaken. Headings included “reoperation”, “return to operation theatre”, “complication”, “appendicectomy”, “outcome”, “abscess drainage”. Articles scoring ≥16 for comparative and ≥10 for non-comparative using MINORS criteria were included.
Results: 2810 articles reviewed were reduced to 52 qualifying studies for a final analysis of 319,053 appendicectomies. Overall, 0.9% (range 0.0% to 14.2%) underwent some form of reintervention. The reoperation rate was 0.6% (range 0.0 to 14.2%) and radiologic drainage rate 1.5% (range 0.0% to 11.1%). Reoperations were significantly associated with a laparoscopic approach, earlier grade of appendicitis and not using drains. Laparoscopy conversion to open and the grade of surgeon performing the appendicectomy did not affect reintervention.
Conclusion: This meta-analysis identified a small but notable reoperation and IR rate, significantly increased by complexity of appendicitis and open surgery. Strategies promoting for earlier presentation and diagnosis with laparoscopic approaches may improve overall outcomes.
Keywords
Appendicectomy; Emergency surgery; Interventional radiology; Reoperation; Quality improvement
INTRODUCTION
Optimizing delivery of emergency general surgery care is important as not only does it account for over 10% of all surgical admissions but also accounts for 50% of surgical mortality in the United States [1]. Within the cohort of emergency surgery patients, acute appendicitis is one of the most common reasons for admission [2]. Other common emergency surgery operations include partial colectomy, small bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions and laparotomy [3]. Appendicitis and its care are often perceived as a simple, easily treated condition and this may contribute to lack of incisive analysis of outcomes. During the 21st century the pooled incidence of appendicitis or appendicectomy was 100 per 100,000 person-years in North America and 151 per 100,000 person-years in Western Europe [4].
While non-operative treatment of appendicitis has been advocated [5], others have questioned its medium-term results [6], surgery remains the cornerstone of care. Both the disease itself and surgery may be associated with complications such as wound infection, intra-abdominal abscess and ileus [7]. Developing an understanding of adverse events post-appendicectomy is important in improving outcomes. Reintervention post appendectomy includes potentially both reoperation and interventional radiology (IR) drainage of collections.
Whilst percutaneous drainage is less invasive than surgical drainage, its use is generally reserved for a radiologically accessible unilocular abscess [8]. Open surgical drainage is used in patients requiring urgent management of overwhelming sepsis, or who fail less invasive treatment modalities [9]. Open surgical drainage is associated with high morbidity and mortality, and a length of stay greater than 2 weeks [10-12].
It is a very significant unexpected outcome for patients and their families. Understanding the frequency and cause of reintervention may alter and help future care. In general readmission following appendicectomy occurs in 4.3% of patients undergoing appendicectomy (range 0.0-14.5%) [13]. Recent published comprehensive guidelines from the World Society of Emergency Surgery in the management of acute appendicitis do not include guidelines relating to reoperation or reintervention [14]. While many studies report both morbidity and reoperation, no meta-analysis of reintervention has been published [15].
This study undertook a meta-analysis of the prevalence and potential predictors of reoperation and IR drainage post appendicectomy [16].
METHODS
Search strategy and study eligibility
A systematic review and meta-analysis of all published English articles was conducted in July 2017, using PubMed and Scopus electronic databases and manual troll for literature in a 5-year period from June 2012 to May 2017. Medical search headings included ‘reoperation’, ‘return to operation theatre’, ‘complications’, ‘appendicectomy, ‘outcomes’, ‘abscess drainage’ with Boolean operators AND or OR.
The method of analysis and inclusion criteria were specified in advance to avoid selection bias and documented in a protocol which was registered and published with the International Prospective Register of Systematic Reviews (PROSPERO) on 09/06/17 (ID CRD42017069040). This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Studies were included in the systematic review if the following criteria were met; studies that involved open or laparoscopic appendicectomy which reported reoperation rates and IR drainage rates, and full articles that were available in the English language. Studies were not included for any of the following reasons; studies that were reviews, meta-analyses, case reports, letters or protocols, studies that did not report key outcomes, interval appendicectomy, antibiotics as a primary intervention, series with less than 50 appendicectomy patients and those which data was inadequate for interpretation via meta-analysis.
Eligibility assessment was performed independently in a blinded standardised manner by two reviewers (ASB, UM). Disagreements between reviewers were resolved by discussion between the two review authors. If no agreement could be reached, a third reviewer decided (AJ).
Definitions
Appendicectomy was defined as the surgical removal of the appendix by either laparoscopic or open methods. Reintervention was defined as unplanned or unexpected reoperation or IR within 30 days of index appendicectomy. Reoperation was expressed as return to operating room (OR), and IR defined as imaging guided draining of a collection. The American Association for Surgery Trauma grading system was used to measure the anatomical severity of appendicitis (Table 1) [17].
|
Grades |
Operative AAST description of appendicitis |
|
Normal |
Normal appendix |
|
Grade 1 |
Acutely inflamed appendix intact |
|
Grade 2 |
Gangrenous appendix intact |
|
Grade 3 |
Perforated appendix with local contamination |
|
Grade 4 |
Perforated appendix with peri appendiceal phlegmon or abscess |
|
Grade 5 |
Perforated appendix with generalized peritonitis |
Table 1: AAST grading system for appendicitis [17]
Quality assessment and data extraction
The descriptive and quantitative data from the screened studies was extracted by the same reviewer (ASB) for the following variables: country of study, study type, study timeline, study size, number of hospital sites, type of procedure, inclusion and exclusion criteria of each study.
Methodological Index for Non-Randomised Studies (MINORS) criteria [18], was used to assess quality as it is designed for the quality assessment of comparative and non-comparative surgical studies using a 3-point scale (0 not reported, 1 reported but inadequate, 2 reported and adequate) on eight items for non-comparative studies and 12 items for comparative studies. The ideal global score for non-comparative and comparative studies was chosen at 16 and 24, respectively. All collated studies including randomised controlled trials were marked against the MINORS criteria to assess the studies with the best methodologies to include in the final analysis. The studies with a MINORS score of ≥16 out of 24 for comparative and ≥ 10 out of 16 for non-comparative were included in the final analysis [19-22].
Data extracted included reintervention rate and potential risk factors. These included the methods of surgical procedure, the grade of surgeon performing the operation, and the pathology of the appendicitis [23].
Statistical Analysis
Overall rates calculation and funnel plots were created using Microsoft Excel 2017. The forest plots and statistical analysis were performed on Revman 5. A dichotomous fixed-effect meta-analysis using the Mantel-Haenszel method was used to determine any statistical significance between the reintervention rates between two groups that were homogenous studies, and random-effect models were used for heterogeneous studies. A sensitivity analysis was performed to investigate the impact of different decisions on the result by comparing fixed-effect and random-effect models. The results were presented in a pooled odds ratio and a 95% confidence interval in a forest plot. Statistical significance was defined as p < 0.05. I2 of > 50% is considered to be substantially heterogeneous [24-30].
RESULTS
Rate of reintervention
The study reviewed 2810 articles of which 165 were found to be potentially suitable. After applying the MINORS cut off score, 52 were used for reintervention rates. Of the 52, 35 had comparative groups to facilitate forest plot meta-analysis. Figure 1 provides a PRISMA flow chart for identification and inclusion of relevant papers.
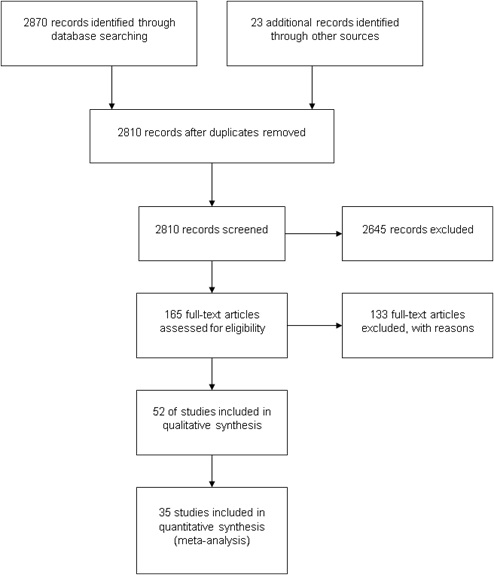 Figure 1: PRISMA Flow Chart.
Figure 1: PRISMA Flow Chart.
This meta-analysis included reported outcomes on a total of 319,053 appendicectomies. The study characteristics are shown in Table 2. Overall, 0.9% (2728/319053) (range 0.0 to 14.2%) underwent some form of reintervention. Subdividing reintervention into reoperation and IR drainage, the reoperation rate was 0.6% (2013/313778) which ranged from 0.0 to 14.2% and IR drainage was 1.5% (583/39799) which ranged from 0.0% to 11.1% [31-33].
|
Study |
Country |
No. of participating hospitals |
Prospective/ Retrospective |
Ages |
Sample size |
Reoperation |
IR drainage |
Overall reintervention |
|
Akkoyn 2012 |
Turkey |
1 |
Retrospective |
1 - 15 y |
234 |
0.9% |
|
0.9% |
|
Almstrom 2014 |
Sweden |
1 |
Retrospective |
1 - 15 y |
2756 |
0.8% |
|
0.8% |
|
Andersson 2014 |
Sweden |
All national hospitals |
Retrospective |
All |
169896 |
0.2% |
|
0.2% |
|
Bansal 2012 |
Switzerland |
1 |
Prospective |
< 15 y |
187 |
1.1% |
1.6% |
2.7% |
|
Chang 2013 |
South Korea |
1 |
Retrospective |
Children |
186 |
0.5% |
1.6% |
2.2% |
|
Collaborative 2013 |
UK |
95 |
Prospective |
All |
3326 |
|
|
2.9% |
|
Columbo 2012 |
UK |
1 |
Retrospective |
> 16 y |
205 |
3.4% |
|
3.4% |
|
Da silva 2014 |
Brazil |
1 |
Retrospective |
< 16 y |
94 |
5.3% |
|
5.3% |
|
Di Saverio 2014 |
Italy |
1 |
Prospective |
>14 y |
210 |
0.0% |
1.4% |
1.4% |
|
Emil 2014 |
Canada |
1 |
Retrospective |
10 - 20 y |
1145 |
0.2% |
1.7% |
1.8% |
|
Frutos 2013 |
Spain |
1 |
Prospective |
> 11 y |
184 |
0.5% |
|
0.5% |
|
Galli 2013 |
USA |
1 |
Retrospective |
> 15 y |
169 |
14.2% |
|
14.2% |
|
Gonenc 2012 |
Turkey |
1 |
Prospective |
> 15 y |
107 |
0.9% |
|
0.9% |
|
Graat 2012 |
Netherlands |
1 |
Retrospective |
All |
894 |
6.3% |
|
6.3% |
|
Kocatas 2013 |
Turkey |
1 |
Prospective |
> 15 y |
96 |
1.0% |
|
1.0% |
|
Kang 2016 |
South Korea |
1 |
Retrospective |
All |
133 |
1.5% |
|
1.5% |
|
Kapishke 2013 |
Germany |
1 |
Retrospective |
< 16 y |
163 |
2.5% |
|
2.5% |
|
Kelly 2014 |
USA |
57 |
Prospective |
2 - 18 y |
5097 |
1.2% |
|
1.2% |
|
Kim 2015 |
South Korea |
1 |
Retrospective |
All |
2587 |
0.2% |
|
0.2% |
|
Kim 2016 |
South Korea |
1 |
Retrospective |
< 18 y |
400 |
1.0% |
|
1.0% |
|
Kronman 2016 |
USA |
23 |
Retrospective |
3 - 18 y |
24984 |
0.2% |
|
0.2% |
|
LaRieveire 2013 |
USA |
All hospitals in Washington state |
Retrospective |
< 18 y |
36525 |
1.7% |
|
1.7% |
|
Lebere 2017 |
USA |
1 |
Retrospective |
> 18 y |
681 |
0.0% |
|
0.0% |
|
Lee 2013 |
South Korea |
1 |
Prospective |
> 16 y |
229 |
0.4% |
|
0.4% |
|
Mason 2012 |
USA |
Multiple |
Prospective |
> 16 y |
13330 |
1.5% |
|
1.5% |
|
Michailidou 2015 |
USA |
1 |
Retrospective |
< 21 y |
264 |
1.1% |
|
1.1% |
|
Michailidou 2015 |
USA |
50 |
Retrospective |
2 - 18 y |
2812 |
1.3% |
|
1.3% |
|
Moazzez 2012 |
USA |
Multiple |
Retrospective |
> 65 y |
3674 |
2.7% |
|
2.7% |
|
Mohamed 2013 |
Egypt |
1 |
Retrospective |
All |
214 |
|
7.5% |
7.5% |
|
Nadeem 2016 |
Pakistan |
3 |
Retrospective |
All |
68 |
1.5% |
|
1.5% |
|
Ndofor 2016 |
South Africa |
1 |
Retrospective |
All |
120 |
1.7% |
4.2% |
5.8% |
|
Putnam 2017 |
USA |
1 |
Prospective |
< 18 y |
410 |
1.2% |
|
1.2% |
|
Reinisch 2017 |
Germany |
1 |
Retrospective |
> 12 y |
680 |
1.9% |
|
1.9% |
|
Rickert 2015 |
Germany |
9 |
Prospective |
> 16 y |
104 |
2.9% |
|
2.9% |
|
Sadot 2013 |
Israel |
1 |
Retrospective |
All |
1899 |
0.2% |
|
0.2% |
|
Sauvain 2016 |
Switzerland |
6 |
Retrospective |
> 16 y |
2559 |
0.5% |
|
0.5% |
|
Schlottman 2016 |
Argentina |
1 |
Retrospective |
All |
225 |
4.9% |
3.1% |
8.0% |
|
Shelton 2014 |
UK |
1 |
Retrospective |
All |
517 |
0.8% |
|
1.4% |
|
Siam 2017 |
Israel |
1 |
Retrospective |
> 16 y |
1649 |
0.5% |
|
0.5% |
|
Sivrikoz 2015 |
USA |
Multiple |
Retrospective |
> 18 y |
1211 |
1.7% |
|
1.7% |
|
Skarda 2015 |
USA |
1 |
Retrospective |
All |
708 |
0.6% |
1.3% |
1.8% |
|
Soll 2016 |
Switzerland |
1 |
Retrospective |
All |
813 |
1.2% |
|
1.2% |
|
Suh 2016 |
South Korea |
1 |
Retrospective |
All |
145 |
0.0% |
0.7% |
0.0% |
|
Sulkowski 2014 |
USA |
44 |
Retrospective |
< 18 y |
33482 |
0.9% |
1.4% |
2.3% |
|
Swank 2014 |
Netherlands |
5 |
Retrospective |
>18 y |
1036 |
|
1.4% |
1.4% |
|
Taguchi 2016 |
Japan |
1 |
Retrospective |
>19 y |
81 |
1.2% |
11.1% |
12.3% |
|
Teoh 2012 |
Hong Kong |
Multiple |
Retrospective |
18 - 75 y |
200 |
|
|
3.0% |
|
Thomson 2015 |
USA |
1 |
Retrospective |
> 12 y |
81 |
12.3% |
1.2% |
13.6% |
|
Van Rossem 2016 |
Netherlands |
8 |
Prospective |
All |
415 |
|
|
7.0% |
|
Van Rossem 2016 |
Netherlands |
8 |
Prospective |
> 18 y |
1378 |
2.0% |
0.9% |
2.8% |
|
Yang 2015 |
South Africa |
5 |
Prospective |
All |
134 |
3.0% |
|
3.0% |
|
Yeom 2014 |
South Korea |
1 |
Retrospective |
All |
84 |
|
2.4% |
2.4% |
Table 2: Study Characteristics.
There was no correlation (r=−0.2) or statistical significance (p=0.3) between the sample sizes of single institutions and reoperation rate (Figure 2). Similarly, there was also no correlation (r=−0.3) or statistical significance (p=0.4) between the sample size institutions and drainage rate (Figure 3).
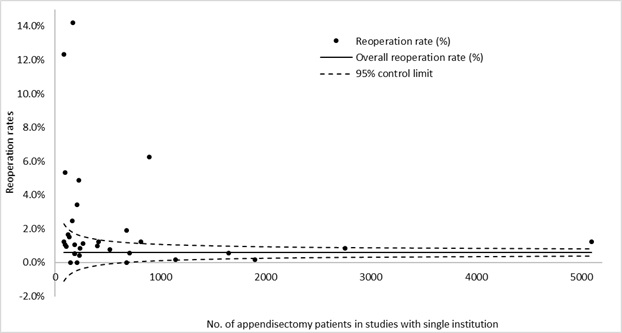 Figure 2: Reoperation rate (%) in relation to no. of appendicectomy patients per study.
Figure 2: Reoperation rate (%) in relation to no. of appendicectomy patients per study.
 Figure 3: IR drainage rate (%) in relation to no. of appendicectomy patients per study.
Figure 3: IR drainage rate (%) in relation to no. of appendicectomy patients per study.
Reasons for reintervention
There were 121 documented reasons for reoperation. 59(48.8%) had organ/space surgical site infection, 7(5.8%) sepsis, 4(3.3%) haematomas, 3(2.5%) superficial incisional surgical site infections, 3(2.5%) small bowel obstructions, 3(2.5%) appendiceal stump complication, 2(1.7%) iatrogenic ileal injuries, 2(1.7%) incisional hernias and 38 had other reasons [34].
For radiological reintervention, there were 558 documented reasons. 551(98.7%) had intra-abdominal abscess, 6(1.1%) had intra-abdominal sepsis and 1(0.2%) had intra-abdominal fluid collection [35].
Risk factors
Significantly fewer reinterventions occurred in the laparoscopic group compared to open (OR=0.65, CI=0.55-0.76, P=< 0.0001, I2=40%). This reintervention related to less reoperations in the laparoscopic group (OR=0.62, CI=0.52-0.73, P=<0.0001, I2=50%) rather than IR drainage (OR=1.18, CI=0.65-2.15, P=0.58, I2=0%) (Figure 4).
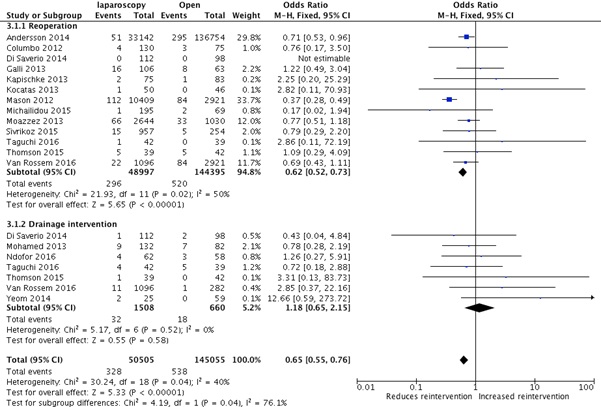 Figure 4: Laparoscopy versus open appendicectomy.
Figure 4: Laparoscopy versus open appendicectomy.
Single port laparoscopy (SILS) versus triple port laparoscopy did not appear to affect reintervention rates (OR=0.23, CI=0.05-1.05, P=0.06, I2=0) (Figure 5). There was also no statistical difference between those completed laparoscopically compared to those undergoing conversion from laparoscopy to open (OR=0.59, CI=0.01-23.86, P=0.94, I2=72%).
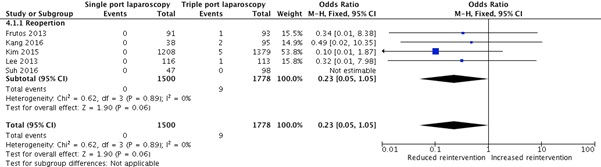 Figure 5: Single port laparoscopy versus triple port laparoscopy.
Figure 5: Single port laparoscopy versus triple port laparoscopy.
Paediatric and general surgeons had similar outcomes (OR=2.50, CI=0.66-9.47, P=0.18, I2=0%), as did resident and senior surgeons (OR=1.42, CI=0.86-2.35, P=0.17, I2=0%). Results show an increased rate of reoperations in AAST grades 3 to 5 by 4.62 times (OR=4.62, CI=2.95-7.22, P=<0.00001, I2=25%) (Figure 6).
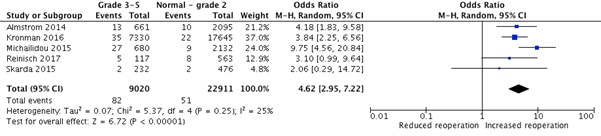 Figure 6: Reoperation rates according to AAST grades.
Figure 6: Reoperation rates according to AAST grades.
There were statistically more reoperations after readmission compared to before patient discharge (OR = 0.09, CI = 0.03 - 0.30, P = < 0.0001, I2 = 0%), and there was a higher rate of reoperation in those who had an intra-abdominal drainage for complicated appendicitis during surgery than those without (OR = 11.01, CI = 1.82 - 66.60, P = 0.009, I2 = 24%).
DISCUSSION
This meta-analysis identified 52 studies contributing to a cohort of over 300,000 patients undergoing appendicectomy, with an overall incidence of reintervention of <1%. Not all 52 studies documented both rates of reoperation and IR data was only extracted if the study clearly stated whether or not reintervention was performed. As a result, the total cohort of patients undergoing reoperation and IR was varied [36-41].
There was a variation with the rate of reintervention from 0.0% to 14.2%. The reasons for this variation are complex and are related to the heterogeneous variables of the studies including sample size, region, age range of participants and inclusion and exclusion criteria [42-45].
Scott, et al. in a US based study of national inpatients from emergency surgery, between 2008-2011, ranked appendicectomy as the 8th most common procedure to result in mortality. Appendicectomy mortality ranked after the following procedures; excision of large intestine, excision of small intestine, laparotomy, operative control of peptic ulcer disease, lysis of peritoneal adhesion, cholecystectomy and total colectomy accordingly [1, 46-50].
Small series which only included complicated appendicitis such as Galli et al. and Thomson et al. reported high reintervention rate. Galli et al in a retrospective based US based adult study, that only included complicated appendicitis, had the largest reintervention rate of 14.2% [29, 51-56]. Thomson et al. had the second highest reintervention rate of 13.6%, a retrospective study of complicated appendicitis [57-64]. Lower rates of reintervention are more likely to be seen in series using large databases, where data has great chance of not being recorded [65-69].
The categorization and reported grading of appendicitis was somewhat problematic. A binary categorical division into complicated and uncomplicated appendicitis is over simplified and limits robust analysis of complications. The American Association for the Surgery of Trauma (AAST) offers a more comprehensive view of the spectrum of the initial disease, thus affording a more robust analysis of outcomes linked to original disease severity [17]. This applies particularly to grade 3 to 5 which are more likely to have complications and reinterventions.
Of the 52 studies included in this meta-analysis there were 7 studies which only included grade 3 to 5 appendicitis [24, 29, 46, 54, 60, 62, 64]. The average rate of reintervention for complicated appendectomies of these 7 studies was higher at 2.5% (2.2-14.2%).
Our meta-analysis identified that IR intervention occurred almost 3 times as frequently as reoperation. The leading cause for IR intervention is largely post-operation intra-abdominal abscess followed by intra-abdominal sepsis and fluid collection. Strategies to reduce intra-abdominal sepsis, as outlined by de Saverio (recent guidelines) should be adopted and analysed [14]. International databases to document IR with clearly defined outcomes would help identify clearer indications and pitfalls.
Allaway, et al. did a study of 4900 post-appendicectomy patients and the role of early laparoscopic washout for persistent sepsis. In their retrospective study 41 (0.8%) patients had a laparoscopic washout,16 (0.3%) had percutaneous drainage, and 6 (0.1%) open drainage. The mean time after appendicectomy to discharge was significantly shorter for laparoscopic washout (4.1 days vs. 10.1 and 9.0 days). The mean time for resolution of SIRS was significantly shorter (2.0 days vs. 3.3 and 5.2 days). They felt that early laparoscopic washout for persistent intra-abdominal sepsis may be an alternative to non-operative management and delayed intervention for intra-abdominal abscess and may have better outcomes than either percutaneous drainage or open drainage [70].
Our meta-analysis found the commonest indication for reoperation was for organ/space surgical site infection, followed by post-operative septic collections and haematoma. These trends seem to be universal irrespective of whether previous studies were from single institutions, registry based, and on the countries studied.
With increasing use of guidelines and opportunities to reduce surgical site infection [71], strategies to optimise surgery need to be considered to reduce reintervention and reoperation rate. These include the hazards of non-operative management and the potential for increased complications in patients who fail non-operative management [72]. The role of delay to definitive surgery in complicated grade 3 - 5 appendicitis results in potential increase of reintervention rate [73].
Reduction of surgical site infection (SSI) may lead to a reduction in reintervention. The use of a bundle may help achieve this and involve multiple elements including wound ring protectors [74], appropriate prophylactic antibiotics [75] and administering prophylactic antibiotics less than 120 minutes before incision [76]. In a new development, a recent meta-analysis by Hureibi et al. showed no reduction in SSI with delayed primary closure [77]. This may help earlier discharge of patients post appendectomy and reduce need for dressing and associated costs.
Ninh and colleagues in a review of 72,538 patients undergoing appendicectomy found that those who developed sepsis post-operatively were more likely to return to the operating room (24.8% vs. 0.8%, be re-admitted (53.4% vs. 2.7% and die within 30 days of surgery, 5.5% vs. 0.05%) [69]. Patients with multiple risk factors may benefit from non-operative management in mild cases however surgery is still indicated with increasing grades and complexity of appendicitis. Several meta-analyses have supported the efficacy of non-operative management and decreased risk of sepsis [78 - 82]. Identifying appropriate patients for non-operative management is crucial as up to 40% will get recurrent appendicitis.
Patients who present with appendicular mass or abscess are a select group whereby depending on surgical preference may either be subjected to a non-operative Ochsner-Sherren type regimen or surgery' not 'Le preference may either be subjected to a non-operative OchsnerSherren type regimen or surgery. Non-operative management involves marking of the palpable mass size on the patient’s skin and commencing antibiotic therapy. Non-surgical treatment of appendicular abscess or phlegmon succeeds in over 90% with an overall rate of recurrence of 7.2%, and 19.7% of cases require percutaneous drainage [83]. Fugazzola, et al. found that children tend to have better results in terms of readmission and complication rate in those managed non-operatively [84]. On the other hand, Mentula et al. demonstrated that laparoscopic appendicectomy had a better outcome in these patients with significant reduction in unplanned readmission. Percutaneous drainage was required in only 7% of the laparoscopic appendicectomy group compared to 30% of the controls with a greater uneventful recovery rate of 90% in the laparoscopic group compared to 50% of conservative group [85]. The issue therefore remains somewhat controversial.
Reoperation for small bowel obstruction was uncommon, counting for only 2.5% of the overall group. Sakari et. al, a recent retrospective study of 402 patients undergoing surgery for small bowel obstruction in Scandinavia, identified that post appendicectomy complications accounted for 29% of the overall population undergoing reoperation for small bowel obstruction [86]. Consideration should potentially be given to the prevention of adhesions developing with the use of icodextrin 4% solution [87,88].
In conclusion, this meta-analysis of reoperation and radiological reintervention post appendicectomy identified a low but not insignificant risk. Patients and their families need to be well informed of these risks. Strategies should be implemented to include pathway and bundle in appendicectomy management to reduce the potential risk of such events occurring.
CONFLICT OF INTEREST
None
This project is supported by the European Union’s INTERREG VA Programme, managed by the Special EU Programmes Body (SEUPB) and Donegal Clinical and Research Academy.
REFERENCES
- Scott JW, Olufajo OA, Brat GA, Rose JA, Zogg CK, et al. (2016) Use of National Burden to Define Operative Emergency General Surgery. JAMA Surg 02115: e160480.
- Addiss DG, Shaffer N, Fowler BS, Tauxe RV (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132: 910-925.
- McCarthy M (2016) Seven procedures account for 80% of emergency general surgery operations, deaths, and complications, US study finds. BMJ 353: i2498.
- Ferris M, Quan S, Kaplan BS, Molodecky N, Ball CG, et al. (2017) The Global Incidence of Appendicitis. Ann Surg 266: 237-241.
- Di Saverio S, Sibilio A, Giorgini E, Biscardi A, Villani S, et al. (2014) The NOTA Study (Non Operative Treatment for Acute Appendicitis). Ann Surg 260: 109-117.
- Wilms IMH, de Hoog DE, de Visser DC, Janzing HM (2011) Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev 9: CD008359.
- Esposito C, Calco AI, Castagnetti M, Alicchio F, Saurez C, et al. (2012) Open versus laparoscopic appendectomy in pediatric population: a literature review and analysis of complications. J Laparoendosc Adv Surg Tech A 22: 834-839.
- Johnson WC, Gerzof SG, Robbins AH, Nabseth DC (1981) Treatment of abdominal abscesses: comparative evaluation of operative drainage versus percutaneous catheter drainage guided by computed tomography or ultrasound. Ann Surg 194: 510-520.
- Brolin RE, Nosher JL, Leiman S, Lee WS, Greco RS (1984) Percutaneous catheter versus open surgical drainage in the treatment of abdominal abscesses. Am Surg 50: 102-108.
- Dobremez E, Lavrand F, Lefevre Y, Boer M, Bondonny JM, et al. (2003) Treatment of post-appendectomy intra-abdominal deep abscesses. Eur J Pediatr Surg 13: 393-397.
- Gorter RR, Meiring S, van der Lee JH, Heij HA (2016) Intervention not always necessary in post-appendectomy abscesses in children; clinical experience in a tertiary surgical centre and an overview of the literature. Eur J Pediatr 175: 1185-1191.
- Brolin RE, Nosher JL, Leiman S, Lee WS, Greco RS (1984) Percutaneous catheter versus open surgical drainage in treatment of abdominal abscess. Am Surg 50: 102-108.
- Bailey K, Choynowski M, Kabir SMU, Lawler J, Badrin A, et al. (2019) Meta-analysis of unplanned readmission to hospital post-appendectomy: an opportunity for a new benchmark. ANZ J Surg 89: 1386-1391.
- Di Saverio S, Podda M, De Simone B, Ceresoli M, Augstin G, et al. (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jarusalem guidelines. World J Emerg Surg 15: 27.
- http://www.icd9data.com/2012/Volume1/800-999/996-999/998/998.9.htm
- Protocol for the surveillance of surgical site infection, version 6 (2013) Public Health England.
- Hernandez MC, Aho JM, Habermann EB, Choudhry AJ, Morris DS et al. (2017) Increased anatomic severity predicts outcomes: Validation of the American Association for the Surgery of Trauma’s Emergency General Surgery score in appendicitis. J Trauma Acute Care Surg 82: 73-78.
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, et al. (2003) Methodological index for non?randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73: 712-716.
- Akkoyun I, Tas Tuna A (2012) Advantages of abandoning abdominal cavity irrigation and drainage in operations performed on children with perforated appendicitis. J Pediatr Surg 47: 1886-1890.
- Almström M, Svensson J, Patkova B, Svenningsson A, Wester T (2016) In-hospital Surgical Delay Does Not Increase the Risk for Perforated Appendicitis in Children: A Single-center Retrospective Cohort Study. Ann Surg. 265: 616-621.
- Andersson R (2014) Short-term complications and long-term morbidity of laparoscopic and open appendicectomy in a national cohort. BMJ Brit Med J 101: 1135-1142.
- Bansal S, Banever G, Karrer F, Partrick D (2012) Appendicitis in children less than 5 years old: Influence of age on presentation and outcome. Am J Surg 204: 1031-1035.
- Bhangu A, Richardson C, Torrance A, Pinkney T, Battersby C, et al. (2013) Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. BMJ Brit Med J 100: 1240-1252.
- Chang H, Han S, Choi S, Oh J (2013) Feasibility of a laparoscopic approach for generalized peritonitis from perforated appendicitis in children. Yonsei Med J 54: 1478-1483.
- Colombo F, Andreani S, Gravante G, Davies A (2012) Laparoscopic open appendicectomies: Results obtained by junior surgeons at a british University Hospital. Eur Rev Med Pharmaco 16: 687-690.
- Da Silva PS, de Aguiar VE, Waisberg J (2014) Pediatric surgeon vs general surgeon: Does subspecialty training affect the outcome of appendicitis? Pediatr Int 56: 248-253.
- Emil S, Elkady S, Shbat L, Youssef F, Baird R, et al. (2014) Determinants of postoperative abscess occurrence and percutaneous drainage in children with perforated appendicitis. Pediatr Surg Int 30: 1265-1271.
- Frutos MD, Abrisqueta J, Lujan J, Abellan I, Parrilla P (2013) Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy. Ann Surg 257: 413-418.
- Galli R, Banz V, Fenner H, Metzger J (2013) Laparoscopic approach in perforated appendicitis: Increased incidence of surgical site infection? Surg Endosc 27: 2928-2933.
- Gonenc M, Gemici E, Kalayci M, Karabulut M, Turhan A, et al. (2012) Intracorporeal Knotting Versus Metal Endoclip Application for the Closure of the Appendiceal Stump During Laparoscopic Appendectomy in Uncomplicated Appendicitis. J Laparoendosc Adv Surg Tech A 22: 231-235.
- Graat L, Bosma E, Roukema J, Heisterkamp J (2012) Appendectomy by Residents Is Safe and Not Associated with a Higher Incidence of Complications. Ann Surg 255: 715-719.
- Kang B, Yoon K, Jung S, Lee G, Lee H (2016) Feasibility of single-incision laparoscopic appendectomy in a small hospital. Ann Surg Treat Res 91: 74-79.
- Kapischke M, Pries A, Caliebe A (2013) Short term and long-term results after open vs. laparoscopic appendectomy in childhood and adolescence: a subgroup analysis. BMC Pediatr 13: 154.
- Kelly K, Fleming F, Aquina C, Probst C, Noyes K, et al. (2014) Disease severity, not operative approach, drives organ space infection after pediatric appendectomy. Ann Surg 260: 466-773.
- Kim J, Kim H, Park S, Lee J, Heo D, et al. (2015) Single-incision Laparoscopic Appendectomy Versus Conventional Laparoscopic Appendectomy. Ann Surg 262: 1054-1058.
- Kim Y, Jung K, Ryu Y, Moon S (2016) Pediatric appendectomy: the outcome differences between pediatric surgeons and general surgeons. Surg Today 46: 1181-1186.
- Kocata? A, Gönenç M, Bozkurt M, Karabulut M, Gemici E, et al. (2013) Comparison of open and laparoscopic appendectomy in uncomplicated appendicitis: A prospective randomized clinical trial. Ulus Travma Acil Cerrahi Derg 19: 200-204.
- Kronman M, Oron A, Ross R, Hersh A, Newland J, et al. (2016) Extended-Versus Narrower-Spectrum Antibiotics for Appendicitis. Pediatrics 138: e20154547
- Lariviere C, McAteer J, Huaco J, Garrison M, Avansino J, et al. (2013) Outcomes in pediatric surgery by hospital volume: A population-based comparison. Pediatr Sug Int 29: 561-570.
- Leberer D, Elliott J, Dominguez E (2016) Patient characteristics, outcomes and costs following interhospital transfer to a tertiary facility for appendectomy versus patients who present directly. Am J Surg pii: S0002-9610: 30725-30750.
- Lee W, Choi S, Lee J, Kim K, Park Y, et al. (2013) Single-Port Laparoscopic Appendectomy Versus Conventional Laparoscopic Appendectomy. Ann Surg 257: 214-218.
- Mason RJ, Moazzez A, Moroney JR, Katkhouda N (2012) Laparoscopic vs. open appendectomy in obese patients: Outcomes using the American College of Surgeons National Surgical Quality Improvement Program database. J Am Col Surg 215: 88-99.
- Michailidou M, Goldstein S, Sacco Casamassima M, Salazar J, Elliott R, et al. (2015) Laparoscopic versus open appendectomy in children: The effect of surgical technique on healthcare costs. Am J Surg 210: 270-275.
- Michailidou M, Sacco Casamassima M, Goldstein S, Gause C, Karim O, et al. (2015) The impact of obesity on laparoscopic appendectomy: Results from the ACS National Surgical Quality Improvement Program pediatric database. J Pediatr Surg 50: 1880-1884.
- Moazzez A, Mason R, Katkhouda N (2013) Thirty-day outcomes of laparoscopic versus open appendectomy in elderly using ACS/NSQIP database. Surg Endosc. 27: 1061-1071.
- Mohamed A, Mahran K (2013) Laparoscopic appendectomy in complicated appendicitis: Is it safe? J Minim Access Surg 9: 55-58.
- Nadeem M, Khan S, Ali S, Shafiq M, Elahi M, et al. (2016) Comparison of extra-corporeal knot-tying suture and metallic endo-clips in laparoscopic appendiceal stump closure in uncomplicated acute appendicitis. Int J Surg Open 2: 11-14.
- Ndofor B, Mokotedi S, Koto M (2016). Comparing laparoscopic appendectomy to open appendectomy in managing generalised purulent peritonitis from complicated appendicitis: The uncharted path. S Afr J Surg 54: 30-34.
- Putnam L, Ostovar-Kermani T, Le Blanc A, Anderson K, Holzmann-Pazgal G, et al. (2017). Surgical site infection reporting: more than meets the agar. J Pediatr Surg 52: 156-160
- Reinisch A, Heil J, Woeste G, Bechstein W, Liese J (2017) The meteorological influence on seasonal alterations in the course of acute appendicitis. J Surg Res 7: 1-7
- Rickert A, Kruger C, Runkel N, Kuthe A, Koninger J, et al. (2015) The TICAP-Study (titanium clips for appendicular stump closure): A prospective multicentre observational study on appendicular stump closure with an innovative titanium clip. BMC Surg 15: 85.
- Sadot E, Wasserberg N, Shapiro R, Keidar A, Oberman B, et al. (2013) Acute Appendicitis in the Twenty-First Century: Should We Modify the Management Protocol? J Gastroint Surg 17: 1462-1470.
- Sauvain M, Slankamenac K, Muller M, Wildi S, Metzger U, et al. (2016) Delaying surgery to perform CT scans for suspected appendicitis decreases the rate of negative appendectomies without increasing the rate of perforation nor postoperative complications. Langenbeck’s Arch Surg 401: 643-649.
- Schlottmann F, Reino R, Sadava E, Campos Arbulú A, Rotholtz N (2016) Could an abdominal drainage be avoided in complicated acute appendicitis? Lessons learned after 1300 laparoscopic appendectomies. Int J Surg 36: 40-43.
- Shelton J, Brown J, Young J (2014) Preoperative C-reactive protein predicts the severity and likelihood of complications following appendicectomy. Ann R Coll Surg Eng 96: 369-372.
- Siam B, Al-Kurd A, Simanovsky N, Awesat H, Cohn Y, et al. (2017). Comparison of Appendectomy Outcomes Between Senior General Surgeons and General Surgery Residents. JAMA Surg 152: 679-685.
- Sivrikoz E, Karamanos E, Beale E, Teixeira P, Inaba K, et al. (2015) The effect of diabetes on outcomes following emergency appendectomy in patients without comorbidities: A propensity score-matched analysis of National Surgical Quality Improvement Program database. Am J Surg 209: 206-211.
- Skarda D, Rollins M, Andrews S, McFadden M, Barnhart D, et al. (2015) One hospital, one appendectomy: The cost effectiveness of a standardized doctor’s preference card. J Pediatr Surg 50: 919-922.
- Soll C, Wyss P, Gelpke H, Raptis D, Breitenstein S (2016) Appendiceal stump closure using polymeric clips reduces intra-abdominal abscesses. Langenbeck’s Arch Surg 401: 661-666.
- Sulkowski J, Asti L, Cooper J, Kenney B, Raval M, et al. (2014) Morbidity of peripherally inserted central catheters in pediatric complicated appendicitis. J Surg Res 190: 235-241.
- Swank H, Van Rossem C, Van Geloven A, In't Hof K, Kazemier G, et al. (2014) Endostapler or endoloops for securing the appendiceal stump in laparoscopic appendectomy: A retrospective cohort study. Surg Endosc 28: 576-583.
- Taguchi Y, Komatsu S, Sakamoto E, Norimizu S, Shingu Y, et al. (2016) Laparoscopic versus open surgery for complicated appendicitis in adults: a randomized controlled trial. Surg Endosc 30: 1705-1712.
- Teoh A, Chiu P, Wong T, Poon M, Wong S, et al. (2012) A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy. Ann Surg 256: 909-914.
- Thomson J, Kruger D, Jann-Kruger C, Kiss A, Omoshoro-Jones J, et al. (2015) Laparoscopic versus open surgery for complicated appendicitis: a randomized controlled trial to prove safety. Surg Endosc 29: 2027-2032.
- van Rossem C, Bolmers M, Schreinemacher M, van Geloven A, Bemelman W (2015) Prospective nationwide outcome audit of surgery for suspected acute appendicitis. Br J Surg 103: 144-151.
- Van Rossem C, Schreinemacher M, Van Geloven A, Bemelman W, Van Acker G, et al. (2016) Antibiotic duration after laparoscopic appendectomy for acute complicated appendicitis. JAMA Surg 151: 323-329.
- Yang E, Cook C, Kahn D (2015) Acute appendicitis in the public and private sectors in cape town, south africa. World J Surg 39: 1700-1707.
- Yeom S, Kim M, Park S, Son T, Jung Y, et al. (2014) Comparison of the outcomes of laparoscopic and open approaches in the treatment of periappendiceal abscess diagnosed by radiologic investigation. J Laparoendosc Adv Surg Tech A 24: 762-769.
- Ninh A, Wood K,Bui AH, Leitman IM (2019). Risk Factors and Outcomes for Sepsis after Appendectomy in Adults. Surg infect 20: 601-606.
- Allaway MGR, Clement K, Eslick GD, Cox MR (2019) Early Laparoscopic Washout may Resolve Persistent Intra-abdominal Infection Post-appendicectomy. World J Surg 43: 998-1006.
- Helmer K, Robinson E, Lally K, Vasquez J, Kwong K, et al. (2002) Standardized patient care guidelines reduce infectious morbidity in appendectomy patients. Am J Surg 183: 608-613.
- Podda M, Cillara N, Di Saverio S, Lai A, Feroci F, et al (2017) Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon 15: 303-314.
- Saar S, Talving P, Laos J, Põdramägi T, Sokirjanski M, et al. (2016) Delay between Onset of Symptoms and Surgery in Acute Appendicitis Increases Perioperative Morbidity: A Prospective Study. World J Surg 40: 1308-1314.
- Ahmed K, Connelly TM, Bashar K, Walsh SR (2016) Are wound ring protectors effective in reducing surgical site infection post appendectomy? A systematic review and meta-analysis. Ir J Med Sci 185: 35-42.
- Kasatpibal N, Nørgaard M, Sørensen HT, Schønheyder HC, Jamulitrat S, et al. (2006) Risk of surgical site infection and efficacy of antibiotic prophylaxis: A cohort study of appendectomy patients in Thailand. BMC Infect Dis 6: 111.
- de Jonge SW, Gans SL, Atema JJ, Solomkin JS, Dellinger PE, et al. (2017) Timing of preoperative antibiotic prophylaxis in 54,552 patients and the risk of surgical site infection: A systematic review and meta-analysis. Medicine 96: e6903.
- Hureibi K, Abraham P, Al-Sunidar O, Alaraimi B, Elzaidi E (2019) To close or not to close? A systemic review and meta-analysis of wound closure in appendicectomy. Int J Surg 16: 9-13.
- Kirby A, Hobson RP, Burke D, Cleveland V, Ford G, et al. (2015) Appendicectomy for suspected uncomplicated appendicitis is associated with fewer complications than conservative antibiotic management: A meta-analysis of post-intervention complications. J Infect 70: 105-110.
- Liu K, Fogg L (2011) Use of antibiotics alone for treatment of uncomplicated acute appendicitis: A systematic review and meta-analysis. Surgery 150: 673-683.
- Mason RJ, Moazzez A, Sohn H, Katkhouda N (2012) Meta- Analysis of randomized trials comparing antibiotic therapy with appendectomy for acute uncomplicated (no abscess or phlegmon) appendicitis. Surg Infect 13: 74-84.
- Varadhan KK, Neal KR, Lobo DN (2012) Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: Meta-analysis of rando- mised controlled trials. BMJ 344: e2156-e2156.
- Findlay JM, Kafsi J el, Hammer C, Gilmour J, Gillies RS, et al (2016) Nonoperative management of appendicitis in adults: A systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 223:814-824.
- Andersson R, Petzold M (2017) Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg 246: 741-748.
- Fugazzola P, Coccolini F, Tomasoni M, Stella M, Ansaloni L, et al. (2019) Early appendectomy vs. conservative management in complicated acute appendicitis in children: a meta-analysis. J Pediatric Surg 54: 2234-2241.
- Mentula P, Sammalkorpi H, Leppäniemi A (2015) Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg 262: 237-242.
- Sakari T, Christersson M, Karlbom U (2020) Mechanisms of adhesive small bowel obstruction and outcome of surgery; a population-based study. BMC Surg 20: 62.
- Catena F, Ansaloni L, Di Saverio S, Pinna A (2012) P.O.P.A. study: prevention of postoperative abdominal adhesions by icodextrin 4% solution after laparotomy for adhesive small bowel obstruction. A prospective randomized controlled trial. J Gastrointestinal Surg 16: 382-388.
- Klink C, Schickhaus P, Binnebosel M, Jockenhoevel S, Rosch R, et al. (2013) Influence of 4% icodextrin solution on peritoneal tissue response and adhesion formation. BMC Surg 13: 34.
Citation: Badrin AS, Maguire U, Johnston A, Bucholc M, Sugrue M (2020) Unplanned Reoperation and Interventional Radiology Post Appendicectomy: A Meta-Analysis. J Emerg Med Trauma Surg Care 7: 049
Copyright: © 2020 Adibah Shamsul Badrin, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

