Upper Full Rehabilitation with One to One Immediate Loading Implants: A Case Report
*Corresponding Author(s):
Maurizio SerafiniPrivate Practitioner, Via Caduti Sul Lavoro, 37 - 66100 Chieti, Italy
Email:serafinidrmaurizio@gmail.com
Abstract
The purpose of this clinical case report is to describe a full-arch rehabilitation with one to one endosseous implant restoration.
Although the proposed treatment may not be within the financial means of most patients, the aesthetical result is higher because of the close similarity between the final restorations and the natural dentition.
The following case demonstrates how dentistry can change patients lives by rehabilitating them with immediate load implants and restore their smiles.
Keywords
Bone Regeneration; C.S.L. 2s implant; Dental implants; Growth factors; One to one immediate loading implants; Oral rehabilitation
Introduction
One to one immediate load implants allows the maintenance of a perfect balanced ratio between the edentulous space and the number of implants inserted, so that load forces can be better dissipate on a wider cancellous and cortical bone area.
Immediate loading implantology allows to place titanium dental implants and prosthesis on the same day or within 24/48 hours from surgery [1].
Bone evaluation needs to be done prior to surgery and if the bone is not adequate, bone grafting is required. Immediate load offers many advantages, first of all significantly decreasing treatment time and trauma for the patient, increasing aesthetic and functional benefits.
This treatment option is becoming increasingly favored, thanks to researchers and manufacturers collaboration and their work on mechanical properties, implants chemical- physical structure and on histological bone/implant interactions [2].
When rehabilitating a patient, one of the most important things to evaluate is the occlusion, which has to be accurately examined to avoid implant fractures or failures due to overload. Neuromuscular occlusion is shaped by muscular and proprioceptive informations and when occlusal loads are transferred trough the prosthesis on each abutment, forces can be dissipated evenly.
One to one dental implants allows an easier cleaning maintenance by patients and has an esthetical outcome similar to natural teeth.
This can be achieved with proper healing of soft tissues trough mucogingival conditionment [3]
The pioneers who started immediate loading implants technique in Italy were: S. Tramonte, D. Garbaccio, Pierazzini, U. Pasqualini, G. Muratori, S. Lobello, A. Morra Greco, N. Marini, M. S. Formiggini; in The U.S.A. Were: L. Linkow, A. J. Viscido, L. C. Ward, Lew, Weiss and many others in Europe.
For the past 50 years, dental science has made huge progress not only on the material used (tantalium or steel) but also on the implant surface which was only machined back then and it was necessary to interconnect all implants with an electro-welded bar to gain stability.
The implants used in the current case are root-form, self-tapered and have incremental deep and thick spires in an apical-coronal direction, which allow forces dissipation and optimal primary stability. If forces are divided in many vectors, they can be better absorbed by cancellous bone and broken down in turn until they fade away in the cortical bone. This process is different for the cylindrical implant in which forces are dissipated on its last spire.
The implants used in the current paper can be inserted in every bone density (D1 to D4) since they determine both vertically and horizontally bone condensation while penetrating, obtaining great primary stability.
Also, it has tapered conic neck, which allows a greater volume between two adjacent implants: a bigger biological surface implies a better vascularization of the papilla.
Implant surface undergoes sandblasting and double etching treatment so to form pores from 0,5 to 20-40 micron, with high Bone Implants Contact (BIC) (Figures 1 & 2).
Wettability after all these procedures is high, the blood coat can easily stick on the surface and create fibrin net adhesion and promote osteogenesis by contact.
Last researches have also recurred to nano technology trough Discrete Crystalline Deposition (DCD) of Calcium Phosphate (CAP) nanoparticles that superimpose a nanotopographic complexity on each implant surface [4].
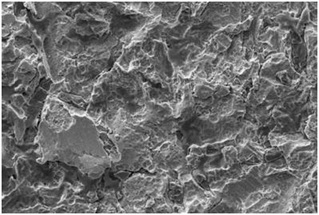 Figure 1: Implant Surface SEM Figure at 20 nano micron.
Figure 1: Implant Surface SEM Figure at 20 nano micron.
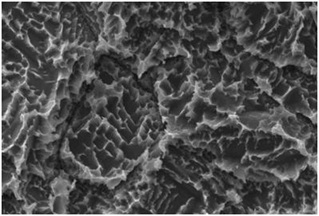 Figure 2: Implant Surface SEM figrure at 1 nano micron.
Figure 2: Implant Surface SEM figrure at 1 nano micron.
In order to use immediate loading implants, the primary stability has to be optimal because it is at first a mechanical phenomenon, but whit the progressive bone remodeling bone cells colonize the rough surface of the implants creating osteointegration.
This is the reason why immediate loading implantology it's not always possible but it requires bone quality and quantity standards.
If those standards are not satisfied, like in the case reported in figures 3 and 4, two stages surgery implantology is the valid alternative.
 Figure 3: Dental scan showing severe bone resorption.
Figure 3: Dental scan showing severe bone resorption.
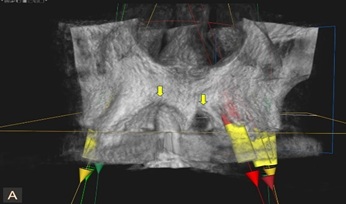 Figure 4: Dental scan showing severe bone resorption.
Figure 4: Dental scan showing severe bone resorption.
Clinical Case
A 49-year-old female patient with unremarkable medical history, presented with the chief complaint of upper loose fixed prosthesis which she has been wearing for many years and gum recessions on lateral incisors which caused the patient social issues. Patient also reported that this situation was causing her working issues because she felt self-consciousness talking or smiling in front of other people.
An Orthopantomogram (OPG) and a Dental Scan were taken (Figures 5-8).
 Figure 5: Orthopantomogram.
Figure 5: Orthopantomogram.
 Figure 6: Dental scan.
Figure 6: Dental scan.
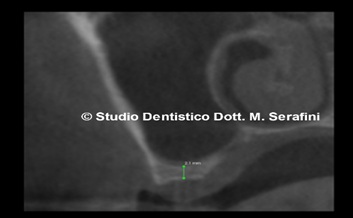 Figure 7: Right side.
Figure 7: Right side.
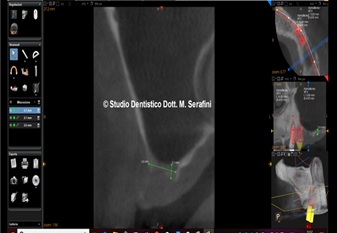 Figure 8: Left side.
Figure 8: Left side.
Radiographic images show severe bone loss with 2 mm bone height on both sides.
Accordingly with the patient the treatment plan is extractions of all upper teeth which are no longer restorable and replace the old prosthesis with an immediate loading implant supported one to one.
Prior to surgery patient was prescribed antibiotic therapy (Amoxicillin and Clavulanic acid 1 g, two times a day for one week).
After removal of the old prosthesis the clinical situation is the one showed in figure 9.
 Figure 9: Clinical situation.
Figure 9: Clinical situation.
6 venous blood tubes samples of 3.5 ml each are taken and centrifuged with sodium citrate as anticoagulant for 20 minutes at 100 rpm obtaining PRP (Figures 10 & 11).
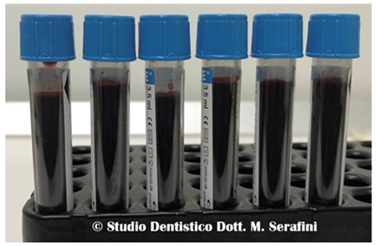 Figure 10: Venous blood.
Figure 10: Venous blood.
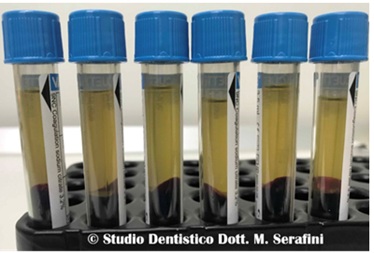 Figure 11: PRP.
Figure 11: PRP.
Under local anesthesia, all upper teeth were extracted, a full thickness flap both palatal and vestibular is reflected and on both sides crestal sinus lift was performed using Crestal Sinus Lift (CSL) implants made by 2s implants. A number of 10 implants are inserted, 3 of them submerged and 7 immediately loaded. Autologous bone graft mixed with PRP is inserted as scaffold both palatal and vestibular (Figures 12-16).
 Figure 12: Right side.
Figure 12: Right side.
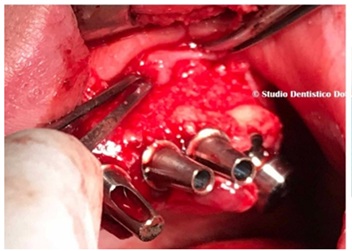 Figure 13: Left side.
Figure 13: Left side.
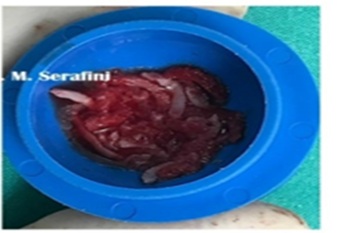 Figure 14: Autologous bone graft.
Figure 14: Autologous bone graft.
 Figure 15: Occlusal view.
Figure 15: Occlusal view.
Temporary prosthesis is fabricated and placed allowing for proper healing of the soft tissues (Figures 16-18).
 Figure 16: Temporary prosthesis.
Figure 16: Temporary prosthesis.
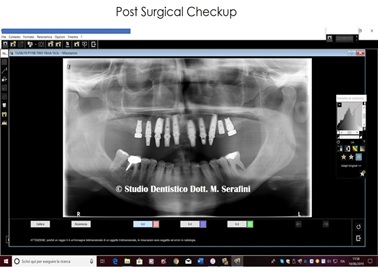 Figure 17: Post-surgical x-ray.
Figure 17: Post-surgical x-ray.
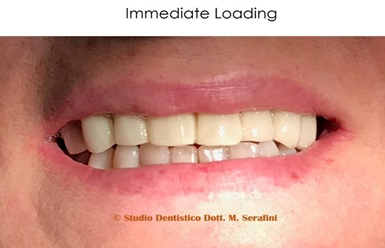 Figure 18: Immediate loading.
Figure 18: Immediate loading.
After 2 months, accordingly with the patient, it was decided to insert one more implant in position 1.6.
A dental scan was taken to plan the surgery as shown in figures19 & 20.
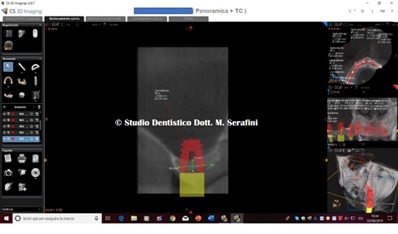 Figure 19: Dental scan.
Figure 19: Dental scan.
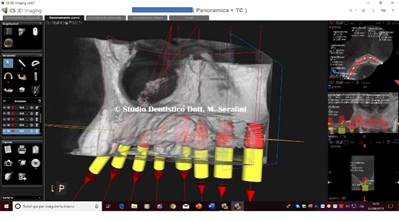 Figure 20: Planning.
Figure 20: Planning.
6 venous blood test tubes samples were taken to obtain PRP (Figure 21).
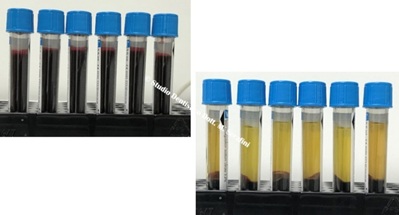 Figure 21: Venous blood and PRP
Figure 21: Venous blood and PRP
Under local anesthesia a full thickness flap is reflected palatal and vestibular (Figures 22 & 23).
 Figure 22: Occlusal view.
Figure 22: Occlusal view.
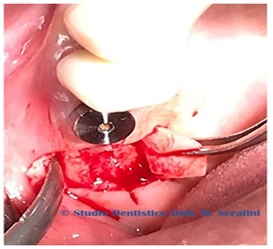
Figure 23: Flap reflected.
Crestal sinus lift trough C.S.L. 2s Implant is performed by placing P.R.P. and a mix of imbibed fibrin sponges and PRF obtained mixing PRP with calcium gluconate as shown in figures 24 & 25.
 Figure 24: Fibrine sponges mixed with PRF.
Figure 24: Fibrine sponges mixed with PRF.
 Figure 25: Fibrine sponges mixed with PRF.
Figure 25: Fibrine sponges mixed with PRF.
Implant positioned showed in figures 26 & 27.
 Figure 26: Implant positioned in position 1.6.
Figure 26: Implant positioned in position 1.6.
 Figure 27: Implant positioned in position 1.6.
Figure 27: Implant positioned in position 1.6.
Post-surgical checkup is shown in figure 28.
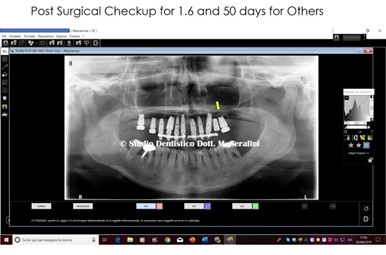 Figure 28: X-ray checkup.
Figure 28: X-ray checkup.
50 days checkup in figure 26 shows a great amount of autologous bone regenerated on the left side pointed out by the yellow arrow in figure 29.
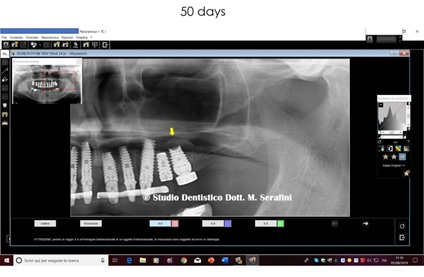 Figure 29: Particular on bone formed after 50 days.
Figure 29: Particular on bone formed after 50 days.
X-ray control after 6 months for the left side and 5 months for the right side in figure 30 shows the sinus floor prior surgery pointed out with red arrow and the bone generated after surgery pointed out with yellow arrows
 Figure 30: X-ray checkup.
Figure 30: X-ray checkup.
After 1 year for 1.6 and 14 months for 2.6 another X-ray is taken together with a clinical picture (Figures 31 & 32).
 Figure 31: X-ray control.
Figure 31: X-ray control.
 Figure 32: Clinical checkup.
Figure 32: Clinical checkup.
Final prosthesis is made and shown in figures 33-35.
 Figure 33: Final outcome.
Figure 33: Final outcome.
 Figure 34: Occlusal view.
Figure 34: Occlusal view.
 Figure 35: Final outcome.
Figure 35: Final outcome.
Discussion
Successful immediate loading dental implant has been reported as early as 1979. Many are the variables to take into consideration when choosing immediate loading implants rehabilitation, such as primary stability as the key requirement for its success. The torque range of implant insertion is from 30 to 45 Ncm, otherwise implants shouldn’t be loaded. Another important variable is the prosthetic design which has to ensure a uniform load distribution [5-7], this is why one to one is the prosthetic choice to ensure even forces on each implant inserted and avoid overload issues. Bone type is another criteria to evaluate for a successful outcome. Compact bone gives good primary stability while cancellous bone doesn't. To facilitate stability in softer bone type, implants features such as the ones of C.L.S. 2s implant used in the current paper, come in clinician's need.
Of course the success of any clinical procedures begins and ends with the selection of the right patient who has to be skilled to understand not only the treatment and its outcomes, but also the importance of frequent checkups and good maintenance at home.
Conclusion
The present case report demonstrates how dentistry can change lives. It also shows how we can satisfied patient's needs by providing predictable, long lasting rehabilitation in less time. When executed precisely, using adequate criteria to evaluate the patient, choosing the implant and perform the surgical and prosthetic treatment, a successful outcome can be achieved.
Further studies are necessary to evaluate long term data of immediate loading implants especially in poor bone quality and quantity and in those cases who need bone regeneration like the one described in the present study.
References
- Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV (2007) Interventions for replacing missing teeth: different times for loading dental implants. Cochrane database Syst Rev 18: CD003878.
- Romanos Ge, Testori T, Degidi M, Piattelli A (2005) Histologic and histomorphometric findings from retrieved, immediately occlusally loaded implants in humans. J Periodontol 76: 1823-1832.
- Gallucci GO, Morton D, Weber HP (2009) Loading protocols for dental implants in edentulous patients. Int J Oral Maxillofac Implants 24: 132-146.
- Serafini M (2021) New Concept of Maxillary Sinus Lift through a New Implant Dedicated: “2s Implant”. J Stem Cell Res Dev Ther 7: 061.
- Grunder U (2001) Immediate functional loading of immediate implants in edentulous arches;two years result. Int J Periodontics Restorative Dent 21: 545-551.
- Tealdo T, Bevilacqua M, Menini M, Pera F, Ravera G, et al. (2001) Immediate versus delayed loading of dental implants in edentulous maxillae: a 36-month prospective study. Int J Prosthodont 24: 294-302.
- Pieri F, Aldini NN, Fini M, Corinaldesi G (2009) Immediate occlusal loading of immediately placed implants supporting fixed restorations in completely edentulous arches: a 1-year prospective pilot study. J Periodontol 80: 411-421.
Citation: Serafini M, Teodoro SD, Romondio L, Zagaria L (2021) Upper Full Rehabilitation with One to One Immediate Loading Implants: A Case Report. J Stem Cell Res Dev Ther 7: 084.
Copyright: © 2021 Maurizio Serafini, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.