
Effects of Diagnostic Mydriasis with Tropicamide and Phenylephrine on Intraocular Pressure
*Corresponding Author(s):
Fiebai BDepartment Of Ophthalmology, University Of Port Harcourt Teaching Hospital, Port Harcourt, Rivers State, Nigeria
Tel:+234 8039509184,
Email:bassief@yahoo.com
Abstract
To determine the effects of diagnostic mydriasis using 1% tropicamide and 2.5% phenylephrine on the intraocular pressure of patients attending the Eye Clinic of University of Port Harcourt Teaching Hospital.
Methods
This was an interventional ‘within-patient’ comparative hospital-based study conducted over 3 months, in which the right eyes of 137 subjects requiring diagnostic mydriasis received 1% tropicamide and 2.5% phenylephrine. The left eyes served as control.
Results
There were 137 study participants: 86 males (62.8%) and 51 females (37.2%). The mean age of participants was 44.87±15.94 years. The baseline IOPs were 12.34±3mmHg for the Right Eye (RE) and 12.09±2.64mmHg for the Left Eye (LE). The mean post dilatation IOP at 30, 45, 60, 90 and 120 minutes in the RE were higher than baseline. The maximum mean post dilatation IOP in the RE was 13.75±2.99mmHg and this occurred at 45 minutes. In the control undilated LE, the mean post dilatation IOPs were lower than baseline at all the follow up periods except at 45 minutes where it was slightly higher (12.11±2.87mmHg). These differences in mean IOP change were statistically significant (p<0.05). At all the follow-up periods, 8.8%-14.6% of participant’s right eyes had large IOP elevations (>5mmHg but <10mmHg). Multiple linear regression analysis showed that pre dilatation IOPs were positively correlated to post dilatation IOPs.
Conclusion
There is need to recheck IOP post dilatation preferably at 45 minutes in all patients who have had diagnostic mydriasis to prevent damage to the optic nerve. Diagnostic mydriasis could safely be done using small concentrations of tropicamide and phenylephrine.
Keywords
INTRODUCTION
Pupillary dilatation (mydriasis) is routinely done for ophthalmological examinations to aid diagnosis (diagnostic mydriasis), treatment and follow up of a wide range of ocular disorders. It facilitates the examination of the peripheral lens, ciliary body, and retina producing better diagnostic and therapeutic outcomes compared to the natural undilated pupil [7-9]. It is also used in the treatment of iritis by preventing the formation of posterior synechia and relieving pain caused by ciliary spasm [10].
Diagnostic mydriasis is usually achieved by the use of mydriatics which are either parasympatholytics or sympathomimetic agents. The parasympatholytics cause pupillary dilatation and accommodation paralysis. The sympathomimetics potentiate or mimic the action of adrenaline by stimulating the dilator pupillae muscle. Examples of parasympatholytics include atropine, homatropine, cyclopentolate and tropicamide. Examples of sympathomimetics include phenylephrine, ephedrine and hydroxyamphetamine [11].
The onset of action of tropicamide is 15-30 minutes with duration of action of 3-8 hours [12]. Phenylephrine achieves maximum mydriasis within 60-90 minutes with recovery after 5-7 hours [13].
Diagnostic mydriasis using these pharmacological agents is not without consequences. Many studies have shown that pupillary dilatation can cause a change in IOP, most supporting an increase in IOP in normal eyes and also abnormal eyes notably those that are glaucomatous [14-22] and others showing no significant change [23,24].
A significant change in IOP that persists and remains untreated serves as a risk factor for glaucoma development and progression. Diagnostic mydriasis which is routinely done in most eye clinics has the potential to increase IOP. It is therefore important to know if this occurs in Nigerian subjects and by how much. Other effects of this intraocular pressure rise include retinal vascular occlusion, anterior ischemic optic neuropathy which could be sight threatening and ocular pain [25,26]. Recognition of susceptible individuals, adequate monitoring and prompt treatment of this elevation of IOP when it occurs are very important.
MATERIALS AND METHODS
Inclusion criteria was adult patients (aged 18 years and above) visiting the eye clinic of UPTH whose eyes required diagnostic mydriasis with normal open angles as seen on gonioscopy. An angle was considered to be normal and open when on gonioscopy, Shaffer’s grade 3 or 4 angles without abnormalities such as new vessels, pigments, pseudoexfoliative materials was found. Exclusion criteria were-high IOP >21mmHg on the visit before dilatation or the day of dilatation, pre-existing ocular pathology such as uveitis, high myopia or glaucoma, patients with one eye and prior use of ocular medications that could influence IOP level.
The details of research were made known to the subjects. Subsequently, their approval and signed informed consent was obtained before inclusion into the study. The approval of the Ethical Committee of the University of Port Harcourt Teaching Hospital to carry out this research was sought and obtained.
RESULTS
|
|
Sex |
|
|
|
Age |
Male |
Female |
Total |
|
18-40 |
30 (60.0) |
20 (40.0) |
50(100.0) |
|
41-83 |
48 (55.2) |
39 (44.8) |
87 (100.0) |
|
Total |
78 (56.9) |
59 (43.1) |
137 (100.0) |
Figure 1 shows the frequency of ocular diagnosis in the right and left eyes of study participants. The highest proportion of participants had refractive errors (53.3% and 54.0% in the right and left eyes respectively). This was followed by cataract which was present in 32.0% and 28.9% of participant’s right and left eyes respectively. Normal ocular findings were present in 11.7% and 14.6% of participant’s right and left eyes respectively. Diabetic macular oedema occurred in 2.9% of participants right and left eyes.
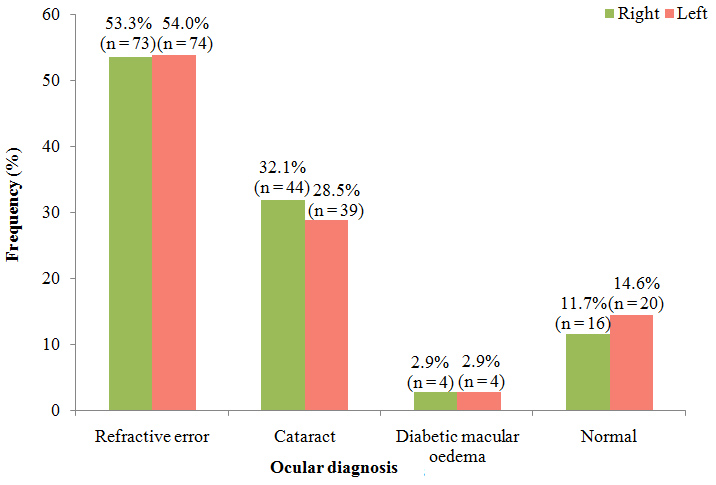
Figure 2 shows the mean changes in IOP from baseline in the dilated right eye and undilated left eye over the various follow up times. At all the follow up times, there was an increase in the mean change in IOP from baseline in the RE with the highest recorded at 45 minutes (1.41mmHg) and the least value recorded at 60 minutes (0.85mmHg).
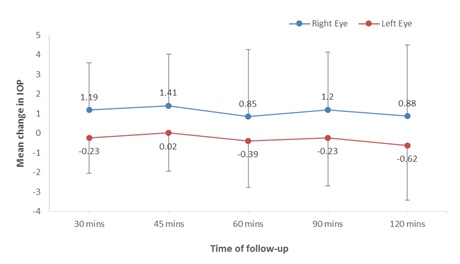
The control LE on the other hand, experienced a reduction from baseline at all the follow up times except at 45 minutes where there was a slight increase of 0.02mmHg. The greatest reduction was noticed at 120 minutes (-0.62mmHg).
Table 2 compares the changes in mean IOP between the dilated RE and undilated LE across the different times of follow up. At all the times of follow up, the mean changes in IOP were higher in the dilated RE with the least change in IOP being +0.85±3.44mmHg recorded at 60 minutes and the greatest change being 1.42±2.63mmHg recorded at 45 minutes. The control LE on the other hand had slight changes with the least being a slight increase 0.02±1.95mmHg recorded at 45 minutes and the greatest being a reduction of -0.62±2.79mmHg recorded at 120 minutes.
|
Time of follow up |
Right Eye |
Left Eye |
Paired t-test |
p-value |
|
30 mins |
1.19±2.40 |
-0.23±1.81 |
6.812 |
0.0001* |
|
45 mins |
1.42±2.63 |
0.02±1.95 |
6.651 |
0.0001* |
|
60 mins |
0.85±3.44 |
-0.39±2.38 |
5.124 |
0.0001* |
|
90 mins |
1.20±2.94 |
-0.21±2.46 |
6.732 |
0.0001* |
|
120 mins |
0.88±3.63 |
-0.62±2.79 |
7.184 |
0.0001* |
These differences in the changes in mean IOP from baseline at all the follow-up times between the RE and LE were statistically significant (p=0.0001).
Table 3 compares Post-dilatation IOP (mmHg) between males and females. Males had a slightly higher mean post dilatation IOP (13.93±2.68mmHg) compared to females (13.45±3.44mmHg). This difference was however not statistically significant (p=0.366).
|
|
Sex |
|
|
|
|
Male mean ± SD |
Female mean ± SD |
t |
p-value |
|
|
Post dilation IOP (mmHg) |
13.93±2.68 |
13.45±3.44 |
0.908 |
0.366 |
Table 4 shows IOP changes above 5mmHg in the dilated RE and control LE across the follow-up period. At all the follow-up times, between 8.8% to 14.6% of participants right eyes had IOP elevations above 5mmHg while only 2.9% of left eyes had same. No participant had elevations above 10mmHg.
|
Follow-up period |
Right Eye |
Left Eye |
|
30 mins |
16 (11.7) |
4 (2.9) |
|
45 mins |
12 (8.8) |
0 (0.0) |
|
60 mins |
16 (11.7) |
4 (2.9) |
|
90 mins |
20 (14.6) |
0 (0.0) |
|
120 mins |
15 (10.9) |
0 (0.0) |
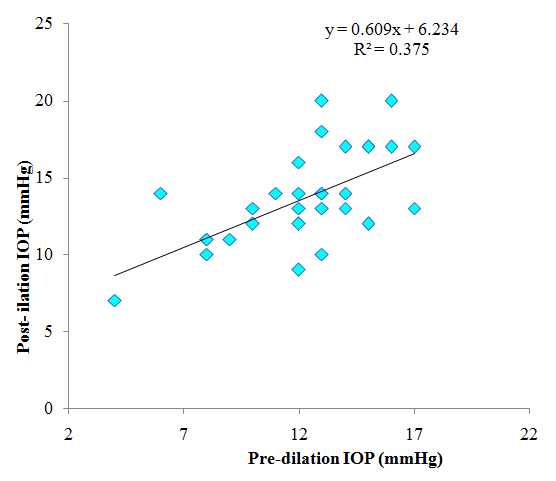
Figure 3 shows the correlation between Pre dilation IOP and post dilatation IOP of the RE. There was a positive correlation between Pre dilation IOP and Post dilation IOP of the RE; as pre-dilation IOP increases, post dilatation IOP increases. This was statistically significant (p=0.0001).
DISCUSSION
In our study, all participants were adults with a mean age of 44.87±15.94 years. This mean age is similar to that reported in other studies [14,15,24]. Hung et al., and Tsai et al., did a similar study but in children [17,23]. This mean age of patients needing diagnostic mydriasis may be a reflection of disorders that cause visual impairment in our environment such as cataracts, age-related macular degeneration and diabetic retinopathy; which are all age-related.
In our series, eyes with normal open angles as seen on gonioscopy were used. The most common ocular diagnosis was refractive error which accounted for the highest proportion. Others were cataract and diabetic macular oedema. Some studies also used patients without glaucoma [14,31]. On the other hand, other studies used eyes with glaucoma [16,32,33] or a mixture of both glaucomatous and non-glaucomatous [15].
In the present study, the mean baseline pre-dilatation IOP was similar in both eyes. However, the mean post dilatation IOP was significantly higher in the dilated right eye than the undilated left eye. Kim et al., and Velasco et al., whose study population was similar to this, reported similar findings [14,31]. Shaw & Lewis and Siam et al., also reported higher post dilatation IOPs but their studies included patients with glaucoma [16,33]. Other studies with similar results were those of Hung et al., and Shihadeh et al., but these studies were on children and patients with pseudoexfoliation respectively [17,19]. On the other hand, Pukrushpan et al., reported no significant difference in mean IOP pre and post dilatation even though their study population was similar to that of this study [24]. This difference in findings may be because of the use of a single agent and the fact that IOP was rechecked only once at 30 minutes after dilatation therefore, elevations which may have occurred thereafter might have been missed. In this study, post dilatation IOP was checked 5 times as such, the tendency of changes being missed was reduced to the barest minimum. In the same vein, Tsai et al., whose study was in children noted no significant, difference between mean pre and post dilatation IOPs [23]. Their study population being children and the fact that IOP was rechecked just once, at 45 minutes may have been responsible for this difference.
Throughout the study period in our study, the IOPs never returned to the baseline. Kim et al., however noted a return to baseline IOP after about 4 hours and Velasco et al., near baseline at 5 hours; in their study, Velasco et al., noted complete return to baseline after 24 hours [14,31]. This study lasted for just 2 hours, and that may be the reason why the IOPs did not return to pre-dilatation levels in the right eye. It is therefore unknown whether the post dilatation IOPs would have returned to baseline levels, had the study lasted longer.
In the dilated right eye, the peak IOP change was noted at 45 minutes. This is similar to a study in Spain where a maximum rise in IOP was achieved at 45 minutes [31]. On the other hand, a Korean study reported maximum IOP rise at 150 minutes post dilatation [14]. This difference may not be unconnected to the fact that in their study, the first post dilatation IOP was checked at 30 minutes and the next at 150 minutes, giving a wide gap between the first and second and it is likely that the IOP may have peaked before then.
At all follow-up periods, 8.8%-14.6% of participant’s right eyes had large IOP elevations (>5mmHg but <10mmHg). This range was chosen because the mean diurnal fluctuations of IOP in normal persons do not exceed 5mmHg [1,34]. Shaw & Lewis however, reported a rise above 5mmHg in 32% of their study participants and more than 10mmHg in 12% of subjects [16]. These changes were noted one-hour post dilatation and may be because the study population included glaucoma patients. Hung et al., whose study population were children, reported much lower percentages with only 3.3% of participants having IOP fluctuations greater than 5mmHg [17].
CONCLUSION
FINANCIAL DISCLOSURE
None
REFERENCES
- Kanski JJ, Bowling B (2011) Clinical ophthalmology: A systematic approach (7thedn) In: Gabbedy R, Cook L (eds.). Elsevier Saunders, Philadelphia, USA. Pg no: 313.
- American Academy of Ophthalmology (2007-2008) Intraocular pressure and aqueous humour dynamics. In: Basic and clinical science course. Glaucoma, American Academy of ophthalmology, San Francisco, USA, Pg no: 17-25.
- Khan JC, Hughes EH, Tom BD, Diamond JP (2002) Pulsatile ocular blood flow: the effect of the valsalva manoeuver in open angle and normal tension glaucoma: A case report and prospective study. Br J Ophthalmol 86: 1089-1092.
- Bakke EF, Hisdal J, Sembo SO (2009) Intraocular pressure increases in parallel with systemic blood pressure during isometric exercise. Invest Ophthalmol Vis Sci 50: 760-764.
- Tan GS, Wong CY, Wong TY, Govindasamy CV, Wong EY, et al. (2009) Is Routine Pupil Dilation Safe among Asian Patients with Diabetes? Invest Ophthalmol Vis Sci 50: 4110-4113.
- Lavanya R, Baskaran M, Kumar RS, Wong H, Chew PT, et al. (2012) Risk of acute angle closure and changes in intraocular pressure after pupillary dilatation in Asian subjects with narrow angles. Am Acad Ophthalmol 119: 474-480.
- Siegel BS, Thompson AK, Yolton DP, Reinke AR, Yolton RL (1990) A comparison of diagnostic outcomes with and without pupillary dilatation. J Am Optom Assoc 61: 25-34.
- Parisi ML, Scheiman M, Coulter RS (1996) Comparison of the effectiveness of a nondilated versus dilated fundus examination in the paediatric population. J Am Optom Assoc 67: 266-272.
- Klein R, Klein BE, Neider MW, Hubbard LD, Meuer SM, et al. (1985) Diabetic retinopathy as detected using ophthalmoscopy, a nonmydriatic camera and a standard fundus camera. Ophthalmology 92: 485-491.
- American Academy of ophthalmology (2007-2008) Ocular pharmacology: Basic and clinical science course. Fundamentals and Principles of Ophthalmology. American Academy of ophthalmology, San Francisco, USA.
- Kanski JJ (1969) Mydriatics. Br J Ophthalmol 53: 428-429.
- FDA (2015) Tropicamide. FDA, Maryland, USA.
- eMC (2016) Minims Phenylephrine Hydrochloride 2.5% w/v, Eye drops solution. Bausch + Lomb UK Ltd, England, UK.
- Kim JM, Park KH, Han SY, Kim KS, Kim DM, et al. (2012) Changes in intraocular pressure after pharmacologic pupil dilation. BMC Ophthalmol 12: 53.
- Hancox J, Murdoch I, Parmar D (2002) Changes in intraocular pressure following diagnostic mydriasis with cyclopentolate 1%. Eye (Lond) 16: 562-566.
- Shaw BR, Lewis RA (1986) Intraocular pressure elevation after pupillary dilatation in open angle glaucoma. Arch Ophthalmol 104: 1185-1188.
- Hung KC, Huang HM, Lin PW (2015) Changes of intraocular pressure and refractive status in children following cycloplegic refraction with 1% cyclopentolate and 1% tropicamide. Taiwan J Ophthalmol 5: 124-127.
- Kristensen P (1968) Pigment liberation test in open-angle glaucoma. Acta Ophthalmol 46: 586-599.
- Shihadeh WA, Ritch R, Scharf B, Liebmann M (2011) Delayed intraocular pressure elevation after pupillary dilation in exfoliation syndrome. Acta Ophthalmol 89: 560-562.
- Valle O (1976) The cyclopentolate provocative test in suspected or untreated open-angle glaucoma III. The significane of pigment for the result of the cyclopentolate provocative test in suspected or untreated open-angle glaucoma. Acta Ophthalmol 54: 654-664.
- Mocan MC, Ustunel S, Dikmetas O, Bozkurt B, Irkec M (2014) The effect of pharmacologic pupillary dilatation on anterior segment parameters in patients with exfoliation syndrome. J Optom 7: 51-56.
- Atalay E, Tamçelik N, Cicik ME (2015) The Impact of Pupillary Dilation on Intraocular Pressure and Anterior Segment Morphology in Subjects with and without Pseudoexfoliation. Curr Eye Res 40: 646-652.
- Tsai IL, Tsai CY, Kuo LL, Liou SW, Lin S, et al. (2012) Transient changes of intraocular pressure and anterior segment configuration after diagnostic mydriasis with 1% tropicamide in children. Clin Exp Optom 95: 166-172.
- Pukrushpan P, Tulvatana W, Kulvichit K (2006) Intraocular pressure change following application of 1% tropicamide for diagnostic mydriasis. Acta Ophthalmol Scand 84: 268-270.
- Hayreh SS (1980) Anterior ischemic optic neuropathy. IV. Occurrence after cataract extraction. Arch Ophthalmol 98: 1410-1416.
- Savage JA, Thomas JV, Belcher CD, Simmons RJ (1985) Extracapsular cataract extraction and posterior chamber intraocular lens implantation in glaucomatous eyes. Ophthalmology 92: 1506-1516.
- Montgomery DMI, Macewan CJ (1989) Pupil dilatation with tropicamide. The effects on acuity, accommodation and refraction. Eye (Lond) 3: 845-848.
- Van der Spek AF, Hantler CB (1986) Phenylephrine eyedrops and anesthesia. Anaesthesiology 64: 812-814.
- Fraunfelder FT, Scafidi A (1978) Possible adverse effects from topical ocular 10% phenylephrine. Am J Ophthalmol 85: 447-453.
- Kenawy NB, Jabir M (2003) Phenylephrine 2.5% and 10% in phacoemulsification under topical anaesthesia: is there an effect on systemic blood pressure? Br J Ophthalmol 87: 505-506.
- Velasco Cabrera J, Eiroa Mozos P, Garcia Sanchez J, Bermudez Rodriguez F (1998) Changes in intraocular pressure due to cycloplegia. CLAO J 24: 111-114.
- Kronfeld PC, McGarry HI, Smith HE (1942) The Effect of Mydriatics Upon the Intra-ocular Pressure in So-Called Primary Wide-Angle Glaucoma. Trans Am Ophthalmol Soc 40: 127-140.
- Siam GA, Monteiro de Barros DS, Gheith ME, Da Silva RS, Lankaranian D, et al. (2007) The amount of intraocular pressure rise during pharmacological pupillary dilatation is an indicator of the likelihood of future progression of glaucoma. Br J Ophthalmol 91: 1170-1172.
- David R, Zangwill L, Briscoe D, Dagan M, Yagev R, et al. (1992) Diurnal intraocular pressure variations: an analysis of 690 diurnal curves. Br J Ophthalmol 76: 280-283.
Citation: Adediji AK, Adio AO, Fiebai B (2019) Effects of Diagnostic Mydriasis with Tropicamide and Phenylephrine on Intraocular Pressure. J Ophthalmic Clin Res 6: 049.
Copyright: © 2019 Adediji AK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

