
Apocrine Adenocarcinoma of Lacrimal Sac Presenting as Chronic Dacryocystitis
*Corresponding Author(s):
Amber HoangDepartment Of Internal Medicine, New Hanover Regional Medical Center, 2131 South 17th Street, Wilmington, North Carolina, United States
Tel:+1 9106677000,
Email:a.hoang@knights.ucf.edu
Abstract
The objective of this paper is to report a case of lacrimal apocrine adenocarcinoma which presented as chronic dacryocystitis. A 62-year-old male was referred by his primary ophthalmologist for evaluation of chronic dacryocystitis of the right eye for 3 months. Biopsy showed a rare and aggressive type of cancer: apocrine adenocarcinoma of the nasolacrimal sac and paranasal sinuses. The patient was treated with orbital exenteration followed by chemoradiation therapy. Apocrine adenocarcinoma, a rare tumor of the eyelid glands, can masquerade as chronic dacryocystitis.
Keywords
INTRODUCTION
The mean age of patients with primary cutaneous apocrine adenocarcinoma is 67 years [2]. The most common surgical approach was local excision (50%), followed by wide excision (30%), mastectomy (4%), and amputation (0.6%) [2]. The prognosis of cutaneous apocrine adenocarcinoma is intermediate with a median survival of 51.5 months [2]. The presence of lymph node metastases significantly decreased survival to 33 months [2].
CASE
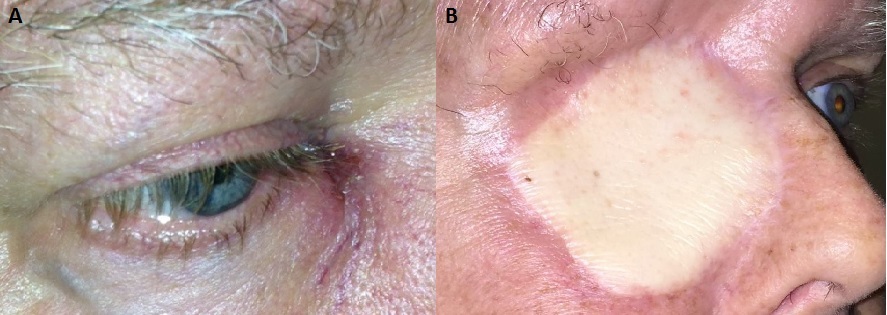
Figure 1: A) Ophthalmic examination at our institution revealed a firm mild nodule at the right lacrimal sac above the medial tendon with erythema and pus drainage. B) The patient was treated with a right orbital exenteration and neck dissection followed by right latissimus dorsi free flap reconstruction.
Given the severe skin erosion and concern for malignancy, radiologic imaging was obtained to assess the orbit and nasolacrimal system. Computed Tomography (CT) of the orbit revealed 2.8 × 1.5 × 1.6cm soft tissue mass seen in the right nasolacrimal duct region abutting the right globe with mild adjacent bone erosion (Figure 2).
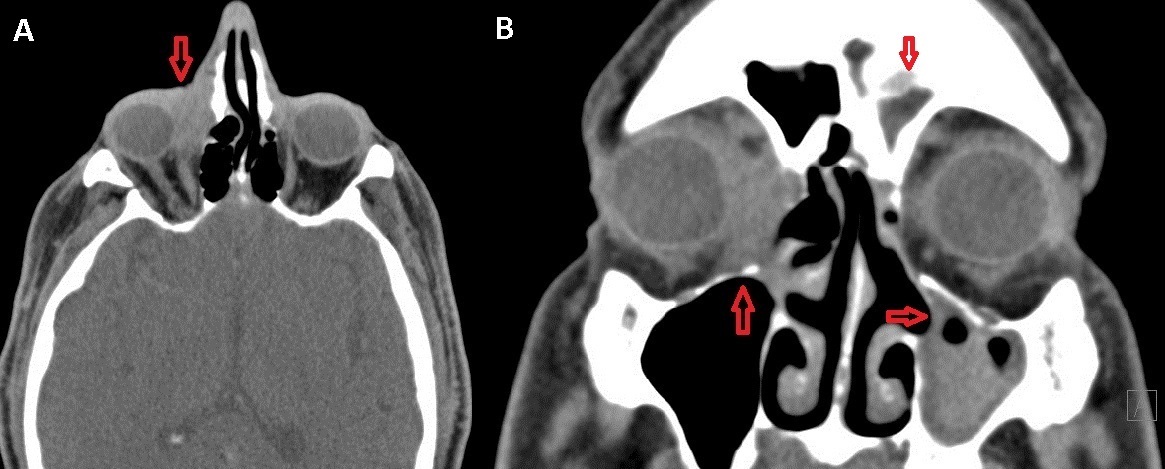
Figure 2: Axial View. A) Non-contrasted CT of orbit reveals 2.8 x 1.5 x 1.6cm soft tissue mass seen in the right nasolacrimal duct region abutting the right globe with mild adjacent bone erosion concerning for malignancy (left). (coronal) B) Polypoid mucosal thickening is seen in the right maxillary sinus. There is mucosal sinus disease with near complete opacification of the left maxillary sinus and complete opacification of the left frontal sinus (right).
Biopsy of the lesion was immediately performed following CT imaging and pathological examination revealed apocrine adenocarcinoma of the right lacrimal sac and sinus mucosa (Figure 3).
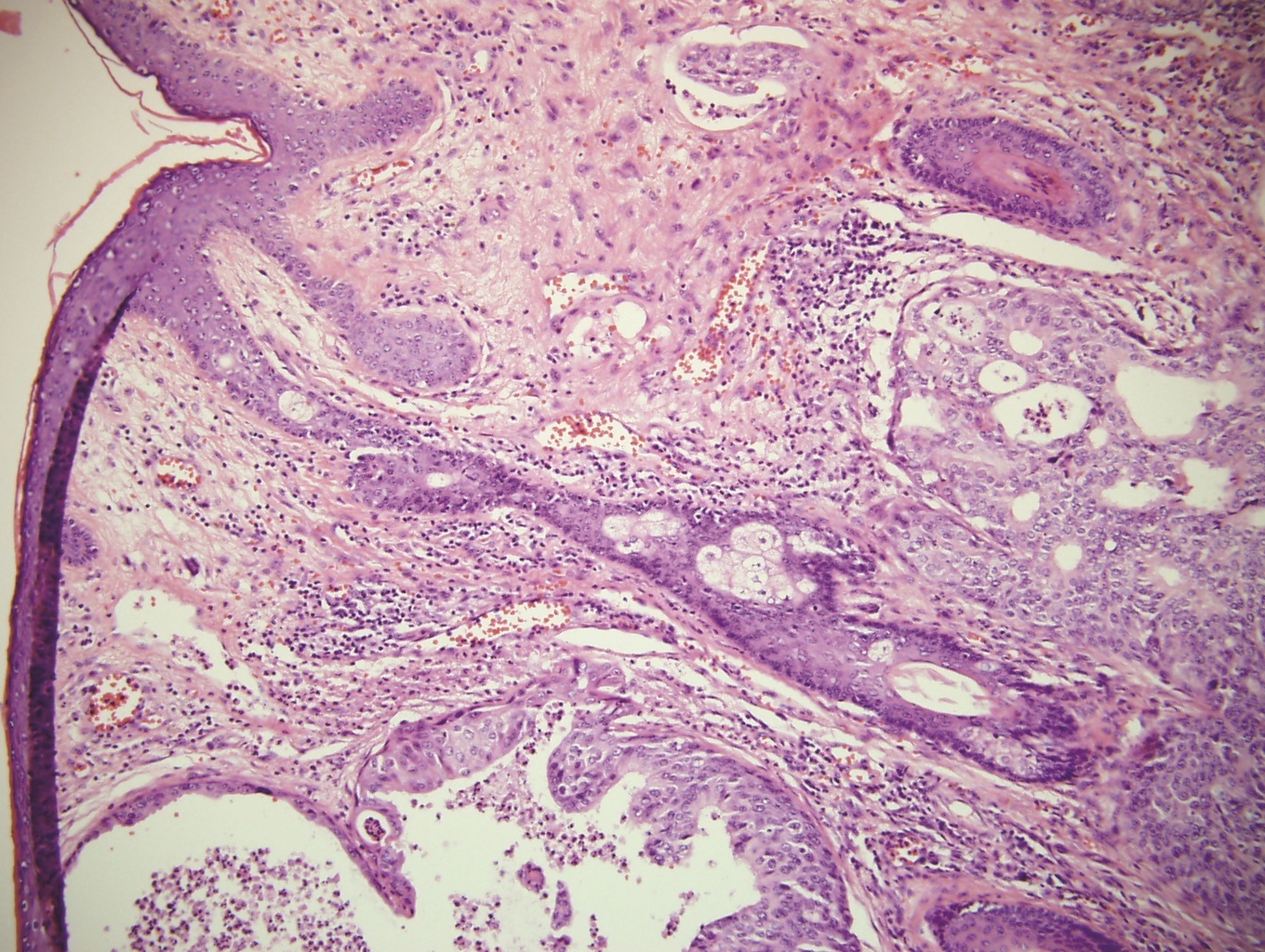
Figure 3: Histopathological examination revealed poorly differentiated apocrine glandular cells consistent with apocrine adenocarcinoma of lacrimal sac extending to the peripheral edge and base.
Positron Emission Tomography (PET) scan revealed moderately avid bilateral level Ib/submandibular lymph nodes consistent with TNM stage of T3N2bM0. The patient underwent radical surgery including open craniofacial resection with frontal craniectomy, subtotal maxillectomy, partial rhinectomy, right orbital exenteration and neck dissection followed by right latissimus dorsi free flap reconstruction. Irrigation was not performed since there was an active infection. He also completed 6 cycles of cisplatin (30mg/m2) and paclitaxel (60mg/m2) with concurrent 200cGy in 30 fractions of radiation therapy. In December 2015, the patient underwent a CT scan of the sinuses, Magnetic Resonance Imaging (MRI) cranial nerve V protocol, and PET scan which all demonstrated no recurrence of disease (Figure 1B).
DISCUSSION
The histopathological diagnostic criteria of apocrine adenocarcinoma described by Kipkie and Haust requires: 1) Pathognomonic “decapitation secretion,” 2) Periodic Acid-Schiff (PAS) positivity, 3) Iron-positive intracellular pigment, 4) Eosinophilic cytoplasm, 5) Tissue from an area normally containing apocrine glands [6]. Immunochemistry is a useful diagnostic tool for differentiating apocrine adenocarcinoma from other subtypes such as apocrine hidrocystomas and apocrine cystadenoma. While benign tumors can also possess PAS-positivity and decapitation secretion, they distinctly stain positive for cytokeratins and human milk fat globulin 1 [7]. Furthermore, GCDFP-15 is helpful in cases where the characteristic “decapitation secretion” of apocrine epithelium is not easily observed, and it has been shown to stain positive in 84% of apocrine-related neoplasms [8]. Although GCDFP-15 was negative in our case, histopathological examination revealed poorly differentiated apocrine glandular cells consistent with apocrine adenocarcinoma.
The recommended management is combined exenteration surgery and radiotherapy in eyelid apocrine carcinomas with advanced metastases [3,5]. Nonmetastatic cases can be successfully treated with wide local resections and radiotherapy as an adjuvant treatment for local orbital or nodal disease [5]. Local lymph node dissections have been reported to have variable success [4,9,10]. Chemotherapy was described in one of the cases with no follow-up report on survival [5]. This case report incorporated TMN staging, which is the current recommendation of the American Joint Committee’s 7th Edition Eyelid Carcinoma Classification System on Cancer [11]. The most important survival determinants are the presence of lymph node involvement, local invasion, and systemic metastasis [3]. TMN staging can help physicians define prognosis and, subsequently, develop an appropriate treatment plan based on the extent of disease.
CONCLUSION
DECLARATION OF INTERESTS
REFERENCES
- Warkel RL (1984) Selected apocrine neoplasms. J Cutan Pathol 11: 437-449.
- Hollowell KL, Agle SC, Zervos EE, Fitzgerald TL (2012) Cutaneous apocrine adenocarcinoma: defining epidemiology, outcomes, and optimal therapy for a rare neoplasm. J Surg Oncol 105: 415-419.
- Figueira EC, Danks J, Watanabe A, Khong JJ, Ong L, et al. (2013) Apocrine adenocarcinoma of the eyelid: case series and review. Ophthal Plast Reconstrc Surg 9: 417-423.
- Ni C, Wagoner M, Kieval S, Albert DM (1984) Tumours of the Moll’s glands. Br J Ophthalmol 68: 502-506.
- Stout AP, Cooley SG (1951) Carcinoma of sweat glands. Cancer 4: 521-536.
- Kipkie GF, Haust MD (1958) Carcinoma of apocrine glands; report of case. AMA Arch Derm 78: 440-445.
- de Viragh PA, Szeimies RM, Eckert F (1997) Apocrine cystadenoma, apocrine hidrocystoma, and eccrine hidrocystoma: three distinct tumors defined by expression of keratins and human milk fat globulin 1. J Cutan Pathol 24: 249-255.
- Ansai S, Koseki S, Hozumi Y, Kondo S (1995) An immunohistochemical study of lysozyme, CD-15 (Leu M1), and gross cystic disease fluid protein-15 in various skin tumors. Assessment of the specificity and sensitivity of markers of apocrine differentiation. Am J Dermatopathol 17: 249-255.
- Shintaku M, Tsuta K, Yoshida H, Tsubura A, Nakashima Y, et al. (2002) Apocrine adenocarcinoma of the eyelid with aggressive biological behavior: report of a case. Pathol Int 52: 169-173.
- Thomson SJ, Tanner NS (1989) Carcinoma of the apocrine glands at the base of eyelashes; a case report and discussion of histological diagnostic criteria. Br J Plast Surg 42: 598-602.
- Ainbinder DJ, Esmaeli B, Groo SC, Finger PT, Brooks JP (2009) Introduction of the 7th edition eyelid carcinoma classification systemc from the American Joint-Committee on Cancer-International Union Against Cancer staging manual. Arch Pathol Lab Med 133: 1256-1261.
Citation: Hoang A, Khine KT, Zaldivar R (2017) Apocrine Adenocarcinoma of Lacrimal Sac Presenting as Chronic Dacryocystitis. J Ophthalmic Clin Res 4: 027.
Copyright: © 2017 Amber Hoang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

