Burnout of Frontline Health Care Workers Working during Sporadic and Cluster Periods of the COVID-19 Pandemic: A Comparative Study
*Corresponding Author(s):
Oyunsuren DDepartment Of Mental Health, School Of Medicine, Mongolian National University Of Medical Sciences, Jamyan St 3, Ulaanbaatar, Mongolia
Tel:+9 7699078521,
Email:oyunsuren.d@mnums.edu.mn
Abstract
The new SARS-n-CoV2 (COVID-19) pandemic is a global threat to the mental, physical and social health of the population. There is an urgent need to conduct psychological, social and mental health research related to the pandemic and to plan long-term interventions. At the beginning of the outbreak, British scholars identified that the priority objectives of research on COVID-19 are to study and report collected information related to anxiety, depression, self-harm (or suicide) and other mental health problems among the general population and vulnerable groups, including frontline staff and health care workers.
Keywords
Burnout; COVID-19 pandemic; Depression
Introduction
Some studies by Chinese researchers in the early stages of the pandemic noted the need for immediate identification of symptoms, such as anxiety, depression and stress, among physicians, nurses and other health care professionals [1]. Who care for and diagnose infected patients and conduct comprehensive mental health care and stress management interventions for them [2,3].
According to a review of 13 studies on the prevalence of SARS-CoV and MERS-CoV in the MEDLINE database of German scholars, quarantine interventions have negative psychological impacts, such as depression, anxiety, anger, stress, posttraumatic stress disorder, social isolation, loneliness and discrimination, not only among the general population but also among frontline health care workers [4].
The COVID-19 pandemic has a significant negative impact on health care workers. This is caused by factors including (but not limited to) increased workload, fear of becoming ill or of family members’ becoming ill, shortages of personal protective equipment and decreases in the care of critically ill patients due to fear [5,6]. Many researchers have established that the COVID-19 outbreak has increased stressors in the health care system and has already increased burnout related to workplace stress [7,8].
Although the information regarding the COVID-19 outbreak’s impact on the mental health of health care workers is incomplete, it is possible to draw some preliminary conclusions based on the research related to previous major epidemics. For example, during and after the SARS outbreak in 2003 and the MERS outbreak in 2012, reports emerged of psychological distress, such as anxiety, fear, discrimination, fatigue and posttraumatic stress disorder, among frontline health care workers [9-11]. Indian researchers have observed that four-stage psychological responses (as in the Kubler-Ross model) in the catastrophic period were manifested for grief in countries affected by the COVID-19 pandemic and having high morbidity and mortality rates [12,13]. According to them, the first stage of this four-stage response occurs in the sporadic or imported cases period, during which the anxiety and fear caused by psychological denial predominate. The next stage of the response is during the period of local transmission (cluster cases), during which psychological distress, such as anxiety, fear and worry, is more likely to increase. The third stage of the response involves community transmission, during which negative emotions, such as anger and rage, may be expressed in depression and anxiety related to the state of uncertainty and unknown. Stage 4 accompanies an epidemic that affects the whole country or region, during which depression may escalate to despair, although people will be able to accept the reality and assess what to do [12].
The results of studies done during and after previous major outbreaks of coronavirus show that the psychological impacts of quarantine during a pandemic can lead to irritability, self-infection, fear of infecting loved ones and family members, denial, anger, frustration, insomnia, loneliness, despair, depression and, in some cases, even suicide [14-16].
In Mongolia, the period of sporadic or imported cases started in March 2020, when the first imported case of COVID-19 was reported, while the period of cluster cases started in November 2020. We aimed in this study to identify the burnout syndrome of frontline health care workers with some mental symptoms, comparing the sporadic and cluster periods of the COVID-19 pandemic.
Goal
To identify the severity of burnout syndrome in frontline health care workers and identify some mental symptoms, comparing periods of the COVID-19 pandemic.
Methods
Study design
The study was conducted in two stages using a descriptive cross-sectional design. The first stage of the study was conducted from August through September 2020 and organized among frontline health care workers caring only for imported cases at the National Center for Communicable Diseases (NCCD), the Central Military Hospital, the National Center for Zoonotic Diseases, the National Center for Mental Health and among some residents who worked in isolation facilities. The second phase of this study was conducted in November 2020, when the domestic outbreak was reported and was organized only among frontline health care workers of the NCCD who worked with cluster cases.
Inclusion criteria
We considered all respondents, such as frontline health care workers, who worked with imported/cluster cases of SARS-CoV2 infected patients, people in isolation who came from infection-outbreak countries and people working in surveillance, screening, disinfection and other COVID-19-related services. Citizenship, nationality, age and gender were not taken into account when recruiting participants in the study; individuals gave written informed consent and we obtained the approval of the health organizations where the individuals worked. Anyone declining to participate in the study was excluded. We used a questionnaire that included general demographic questions, such as age, gender, educational status, occupation, position, marital status, family, living condition, household monthly income, working years and questions to solicit information related to pandemic care, such as the experience of pandemic care and current duties.
Method of evaluating fear of the COVID-19 infection
We used a 5-point question, with a higher score reflecting a greater fear of COVID-19 infection.
Method of evaluating the anxiety of frontline staff
We used the Generalized Anxiety Disorder 7-item (GAD-7) [17], a self-completed questionnaire for assessing anxiety level that is widely used in primary health care. The reliability of the answers to the questions was 0.90 using Cronbach’s alpha coefficient.
Method of evaluating the depression of frontline staff
We usedthe Patient Health Questionnaire 9-item (PHQ-9) [18], a self-completed questionnaire for assessing depression that is widely used in primary health care. The reliability of the answers to the questions was 0.90 using Cronbach’s alpha coefficient.
Method of evaluating the stress level of frontline staff
We used the Impact of Event Scale-Revised (IES-R) [19], a self-completed questionnaire for assessing stress impact and the reliability of the answers to the questions was 0.94 using Cronbach’s alpha coefficient.
Method of evaluating burnout of frontline staff
We used the Maslach Burnout Inventory (MBI) [20], a self-completed questionnaire for assessing burnout syndrome and the reliability of the answers to the questions was 0.86 using the Cronbach’s alpha coefficient.
Ethical statement
Ethical approval was obtained from the Medical Ethics Committee of the Ministry of Health on July 08, 2020 (No. 172). All subjects gave written informed consent. The data were collected only after the administrative approvals were obtained by signed consent.
Statistical Analysis
The statistical analysis of the results of the survey was done using descriptive analysis using SPSS 21.0 and STATA 16.0. The data were processed by Microsoft Word and Microsoft Excel and were initially analyzed using descriptive statistics, mean, standard deviation, Pearson correlation and multiple logistic regression analysis. The non-parametric correlation was significant at the p<0.01 level and p<0.05 level (two-tailed). All reference categories were “Yes,” and the dependent variables were seven variables leading to burnout, with a binary outcome answered by “Yes” or “No.” Multiple regression analysis showed the relationships between burnout and the above seven variables. The reliability of the answers to the questions in the questionnaires for assessing the mental health state of the health care workers was calculated using Cronbach’s alpha.
Results
A total of 435 health care workers aged 21-63 years participated in the study. Of the respondents, 369 (84.8%) were health care workers who worked during the sporadic period of the COVID-19 pandemic. The average age of the respondents was 38.4 ± 8.7 years and the average of years working in the health care sector was 11.3 ± 8.8. Some demographic variables of the respondents are summarized in (Table 1).
As shown in (Table 1), females (p = 0.009), health care workers aged 25-44 years and medical doctors and nurses (p = 0.001) with higher education (p = 0.03) were more likely to be involved in this study at any period of the COVID-19 pandemic.
|
Variables |
Sporadic period |
Cluster period |
Total (n) |
||
|
Number of participants (n) |
Percent (%) |
Number of participants (n) |
Percent (%) |
||
|
Sex |
|||||
|
Male |
86 |
23.3 |
6 |
9.1 |
92 |
|
Female |
283 |
76.7 |
60 |
90.9 |
343 |
|
Total |
369 |
100 |
66 |
100 |
435 |
|
Age group |
|
|
|
|
|
|
Under 24 y.o. |
11 |
3.0 |
1 |
1.5 |
12 |
|
25-34 y.o. |
136 |
36.9 |
18 |
27.3 |
154 |
|
35-44 y.o. |
127 |
34.4 |
20 |
30.3 |
147 |
|
45-54 y.o. |
83 |
22.5 |
24 |
36.4 |
107 |
|
55-64 y.o. |
12 |
3.2 |
3 |
4.5 |
15 |
|
Total |
369 |
100 |
66 |
100 |
435 |
|
Education |
|
|
|
|
|
|
Higher |
245 |
66.4 |
30 |
45.4 |
275 |
|
High |
70 |
19.0 |
19 |
28.8 |
89 |
|
Secondary |
15 |
4.1 |
4 |
6.1 |
19 |
|
Technical and vocational education |
7 |
1.9 |
4 |
6.1 |
11 |
|
Specialized secondary education |
29 |
7.8 |
8 |
12.1 |
37 |
|
Primary |
3 |
0.8 |
1 |
1.5 |
4 |
|
Total |
369 |
100 |
66 |
100 |
435 |
|
Occupation |
|
|
|
|
|
|
Medical doctor |
122 |
33.1 |
9 |
13.6 |
131 |
|
Nurse |
84 |
22.8 |
29 |
43.9 |
113 |
|
Epidemiologist |
17 |
4.6 |
0 |
0 |
17 |
|
Biomedical specialist |
6 |
1.6 |
2 |
3.0 |
8 |
|
Medical specialist |
60 |
16.3 |
7 |
10.6 |
67 |
|
Other |
80 |
21.6 |
19 |
28.9 |
99 |
|
Total |
369 |
100 |
66 |
100 |
435 |
Table 1: Some demographic variables of the total respondents.
As shown in (Table 2), of the total respondents, 84%-92.4% had fear of the COVID-19 infection, 23.6%-51.1% were anxious, 49.1%-69.1% were depressed, 19%-34.8% were severely stressed and 6.7%-13.6% had statistically significant burnout syndrome. Also, 51.5%-67.7% of frontline health care workers in the COVID-19 pandemic reported that they had previous experience with an outbreak of infection, such as SARS, H1N1, or hand-foot-mouth disease (p = 0.001).
|
Variables |
Sporadic period |
Cluster period |
Total (n) |
p-value |
||
|
Number of participants (n) |
Percent (%) |
Number of participants (n) |
Percent (%) |
|||
|
Fear of COVID-19 infection (by Likert score of 0-5) |
||||||
|
No fear (0-1) |
59 |
16.0 |
5 |
7.6 |
64 |
0.001 |
|
Mild (2-3) |
156 |
42.3 |
14 |
21.2 |
170 |
|
|
Moderate (4) |
80 |
21.7 |
21 |
31.8 |
101 |
|
|
High (5) |
74 |
20.0 |
26 |
39.4 |
100 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
GAD-7 score |
||||||
|
Minimal (0-4) |
245 |
66.4 |
27 |
40.9 |
272 |
0.001 |
|
Mild (5-9) |
99 |
26.8 |
28 |
42.4 |
127 |
|
|
Moderate (10-14) |
21 |
5.7 |
8 |
12.1 |
29 |
|
|
Severe (15-21) |
4 |
1.1 |
3 |
4.6 |
7 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
PHQ-9 score |
||||||
|
Minimal (1-4) |
188 |
50.9 |
21 |
31.9 |
209 |
0.004 |
|
Mild (5-9) |
143 |
38.8 |
29 |
43.9 |
172 |
|
|
Moderate (10-14) |
29 |
7.9 |
14 |
21.2 |
43 |
|
|
Moderately severe (15-19) |
2 |
0.5 |
0 |
0 |
2 |
|
|
Severe (20-27) |
7 |
1.9 |
2 |
3.0 |
9 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
IES-R score |
||||||
|
0-23 |
299 |
81 |
43 |
65.2 |
342 |
0.009 |
|
24-32 |
34 |
9.2 |
8 |
12.1 |
43 |
|
|
33-38 |
12 |
3.3 |
7 |
10.6 |
19 |
|
|
39 and above |
24 |
6.5 |
8 |
12.1 |
32 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
Burnout syndrome |
||||||
|
Have no burnout syndrome |
348 |
94.3 |
57 |
86.4 |
405 |
0.019 |
|
Have burnout syndrome |
21 |
5.7 |
9 |
13.6 |
30 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
Table 2: Some mental health variables of the frontline health care workers during the COVID-19 pandemic.
Table 3 summarizes the results of three components of burnout syndrome among frontline health care workers during the sporadic and cluster periods of the COVID-19 pandemic. As shown in (Table 3), 89.7% of the respondents who worked at the frontline of health care during the sporadic period of the COVID-19 pandemic had Emotional Exhaustion (EE), which is a component of burnout syndrome and the mean score of EE was 7.78 ± 6.25. Among the respondents, 73.4% had Depersonalization (D), which is a component of burnout syndrome and the mean score of D was 4.30 ± 5.09 during the sporadic period of the COVID-19 pandemic. Furthermore, 70.7% of the respondents had Personal Accomplishment (PA), which is a component of burnout syndrome and the mean score of PA was 34.48 ± 15.82 during the sporadic period of the pandemic.
|
Variables |
The sporadic period of the COVID-19 pandemic |
The cluster period of the COVID-19 pandemic |
Total (n) |
Chi-square
p-value |
||
|
Cases (n) |
Percent (%) |
Cases (n) |
Percent (%) |
|||
|
Level of emotional exhaustion |
||||||
|
Never |
38 |
10.3 |
3 |
4.5 |
41 |
6.751 0.08 |
|
Low |
294 |
79.7 |
50 |
75.8 |
344 |
|
|
Moderate |
30 |
8.1 |
11 |
16.7 |
41 |
|
|
High |
7 |
1.9 |
2 |
3.0 |
9 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
Level of depersonalization |
||||||
|
Never |
98 |
26.6 |
15 |
22.7 |
113 |
5.903 0.116 |
|
Low |
161 |
43.6 |
25 |
37.9 |
186 |
|
|
Moderate |
82 |
22.2 |
15 |
22.7 |
97 |
|
|
High |
28 |
7.6 |
11 |
16.7 |
39 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
Level of personal accomplishment |
||||||
|
Never |
123 |
33.3 |
27 |
40.9 |
150 |
3.215 0.36 |
|
Low |
47 |
12.7 |
6 |
9.1 |
53 |
|
|
Moderate |
91 |
24.7 |
19 |
28.8 |
110 |
|
|
High |
108 |
29.3 |
14 |
21.2 |
122 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
|
Burnout syndrome |
||||||
|
Have no burnout syndrome |
348 |
94.3 |
57 |
86.4 |
405 |
5.504 0.019 |
|
Have burnout syndrome |
21 |
5.7 |
9 |
13.6 |
30 |
|
|
Total |
369 |
100 |
66 |
100 |
435 |
|
Table 3: Burnout syndrome among frontline health care workers during COVID-19 pandemic.
Among the respondents, 95.5% who worked at the frontline of health care during the cluster period of the COVID-19 pandemic had EE and the mean score of EE was 10.17 ± 8.28. Of the respondents, 77.3% had D during the cluster period of the pandemic and the mean score of D was 6.55 ± 7.79. During the cluster period of the pandemic, 78.8% of the respondents had PA and the mean score of PA was 33.23 ± 16.09.
In other words, physicians and health care workers working at the frontline of the COVID-19 pandemic saw an increase in the incidence of these three symptoms of burnout syndrome by 5.8%-9.1%, but no statistically significant differences between the pandemic periods were observed (Figure 1). Shows the results of the COVID-19 pandemic using a comparison of the symptoms of burnout syndrome in frontline physicians, nurses, nd other health care workers according to their roles.
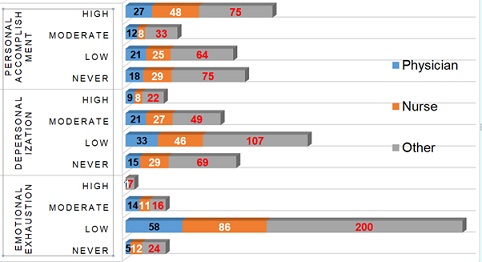 Figure 1: Three components of burnout syndrome in frontline health care workers (by their roles).
Figure 1: Three components of burnout syndrome in frontline health care workers (by their roles).
As seen in (Figure 1), 76.9%-93.6% of the total 78 physicians who worked at the frontline of the COVID-19 pandemic care had burnout syndrome (EE 93.6%; D 80.8%; PA 76.9%) at mild to high levels, while 73.6%-89.1% of the 110 responding nurses who cared for infected cases had burnout syndrome (EE 89.1%; D 73.6%; PA 73.6%) at mild to high levels. Of the 247 respondents in other roles (laboratory staff, worker at an isolation facility, management, meal prepper, driver, epidemiologist, etc.) at the frontline of pandemic health care, 69.6%-90.3% had burnout syndrome (EE 90.3%; D 72.1%; PA 69.6%) at mild to moderate levels. An average of two-thirds of physicians and other health workers at the frontline of pandemic care were assessed with burnout syndrome. Nurses who cared for infected cases were more burned out than others (Table 4). Summarizes the results of correlation analysis for the factors related to the burnout of frontline health workers during the cluster period of the COVID-19 pandemic. These factors were used as independent variables for the univariate and multivariate regression. Burnout was significantly related to cluster period, previous experience, fear of infection, anxiety, depression, high IES-R score and immune suppression.
|
Variables |
Burnout |
Cluster period |
Working at the NCCD |
Physician |
Nurse |
Previous experience |
Fear of infection |
Anxiety |
Depression |
High IES-R score |
Immune suppression |
|
Burnout |
1 |
||||||||||
|
Cluster period |
0.112* |
1 |
|||||||||
|
Working at the NCCD |
0.068 |
0.388** |
1 |
||||||||
|
Physician |
0.015 |
-0.064 |
-0.064 |
1 |
|||||||
|
Nurse |
0.05 |
0.137** |
0.067 |
-0.272** |
1 |
||||||
|
Previous experience |
0.105* |
0.107* |
0.301** |
0.022 |
0.197** |
1 |
|||||
|
Fear of infection |
0.148* |
0.212** |
0.138** |
0.012 |
-0.072 |
0.004 |
1 |
||||
|
Anxiety |
0.202** |
0.189** |
-0.023 |
0.01 |
-0.046 |
-0.067 |
0.092 |
1 |
|||
|
Depression |
0.207** |
0.137** |
0.05 |
-0.018 |
0.083 |
0.018 |
0.024 |
0.564** |
1 |
||
|
High IES-R score |
0.164** |
0.129** |
0.016 |
-0.012 |
0.031 |
0.017 |
0.028 |
0.183** |
0.115* |
1 |
|
|
Immune suppression |
0.236** |
0.077 |
0.029 |
0.006 |
-0.002 |
-0.005 |
0.110* |
0.273** |
0.218** |
-0.06 |
1 |
*p<0.05, ** p<0.01
Table4: Results of correlation analysis for the factors related to the burnout of frontline health care workers during the cluster period of the COVID-19 pandemic.
Working during the cluster period of the COVID-19 pandemic was significantly related to working at the NCCD, working as a nurse caring for infected cases, previous experience, fear of infection, anxiety, depression and high IES-R score. Unexpectedly, burnout and cluster period were not significantly related to working as a physician. In this study, univariate and multiple regression analyses were conducted. A summary of the variables associated with influencing factors for COVID-19-related burnout among the 435 respondents are provided in (Table 5).
|
Variables |
Univariate analysis |
Multivariate analysis |
||
|
Beta |
p value |
Beta |
p value |
|
|
Cluster period |
0.382 (0.167-0.876) |
0.023 |
0.987 |
0.980 |
|
Previous experience |
0.403 (0.175-0.927) |
0.033 |
2.477 |
0.047 |
|
Fear of infection |
0.288 (0.125-0.662) |
0.003 |
2.741 |
0.030 |
|
Anxiety |
0.194 (0.084-0.447) |
0.001 |
1.416 |
0.517 |
|
Depression |
0.107 (0.032-0.359) |
0.001 |
5.068 |
0.021 |
|
High IES-R score |
0.179 (0.060-0.537) |
0.002 |
4.608 |
0.022 |
|
Immune suppression |
0.140 (0.058-0.341) |
0.001 |
4.383 |
0.005 |
Table 5: Analysis of variables associated with influencing factors for COVID-19-related burnout in frontline nurses during the cluster period of the pandemic.
As summarized in table 5, previous experience (odds ratio [OR] = 0.40), fear of infection (OR = 0.29), anxiety (OR = 0.19), depression (OR = 0.11), high IES-R score (OR = 0.18) and immune suppression (OR = 0.14) were not affected alone in the cluster period of COVID-19-related burnout syndrome by univariate regression analysis. However, previous experience (OR = 2.47; p = 0.047), fear of infection (OR = 2.74; p = 0.03), depression (OR = 5.07; p = 0.021), high IES-R score (OR = 4.61; p = 0.022) and immune suppression (OR = 4.38; p = 0.005) were significantly associated with the COVD-19 pandemic-related burnout syndrome, with nearly 2.5-5.1 fold risks in the multivariate regression analysis.
Discussion
In other outbreaks of the coronavirus group, such as theSARS-CoV-1 outbreak [21], many psychiatric symptoms (posttraumatic stress disorder, anxiety, depression, etc.) were recorded in the community and among medical staff, just as during the outbreak of the new SARS-CoV-2 virus [22,23]. Scholars in the U.K., Lebanon and China have found that high levels of anxiety, depression and fear were registered among physicians and nurses working with isolated cases of the new coronavirus infection [24-26]. Also, physicians and nurses working in frontline or isolation facilities feared spreading the infectionto their families and close friends [27,28]. According to the results of the study, which included sampling from 194 cities in China, the psychological impact of the COVID-19 pandemic was rated as moderate to severe, with the findings assessing moderate to severe anxiety and depression in the population [29].
In 14 studies on health care workers in departments of infectious diseases, internal medicine and intensive care wards, depression and anxiety symptoms were more commonly reported among those with less stressful experience and the severity of mental symptoms was influenced by age, gender, occupation, specialization, type of activities performed and proximity to COVID-19 patients [30,31]. According to our findings, the fear of infection, anxiety and depression of frontline health care providers at any time during the pandemic were statistically significant and close to the results of the studies mentioned above.
Burnout syndrome is caused by chronic stress in the workplace and, according to Maslach and Jackson [32],has three basic dimensions: EE, D and PA. The burnout of the health care workers depends on the safety and fate of critically ill patients [33,34]. Furthermore, many studies are suggesting that burnout is more linked to anxiety, depression, familial stress, alcohol and drug abuse and suicide among health care workers [35-37].
Although the burnout of health care workers related to the COVID-19 pandemic has not been fully studied, it may be associated with a variety of workplace problems, job conditions and psychological responses, such as anxiety and depression. There are several risks in the pandemic situation, including increased workloads for health care workers in times of extreme stress, rapid changes related to new care guidelines, using new guidelines in clinical practice, the need for high-risk relocation, the need to avoid infecting loved ones, etc. Therefore, during the first six months of the pandemic, health care workers may become burnt out due to job changes, workplace safety and psychological trauma [24,38,39].
Researchers argue that the risk of burnout among physicians is greater because they exceed the level of experience and are more prone to stress than other professionals. Furthermore, burnout is associated with decreased PA and low efficiency among physicians as well as reduced job satisfaction [40,41]. Irritability and dissatisfaction with work can negatively affect personal well-being, willingness to work and the ability to care for patients [42,43]. Furthermore, physician burnout increases the risk of professional mistakes, which can adversely affect the patient’s condition [44-46]. It is important to consider that increased levels of depression among physicians and health professionals may increase the risk of suicide [47-50].
According to Portuguese researchers, the high levels of stress and depression among 2,008 health care workers at the frontline of the COVID-19 pandemic were statistically significant, with a high incidence of the three dimensions of burnout syndrome [51].
As our results show, burnout syndrome among frontline health care workers during the COVID-19 pandemic is associated with nearly 2.5-5.1 fold increased risks related to their work experience, fear of infection, depression, high impact of severe stress and immune suppression due to severe stress. This result, as many researchers have noted, suggests that the outbreak of COVID-19 is a sign that health workers are becoming overwhelmed and exhausted.
Limitations of the study
There were several difficulties in conducting this study. First, there had been no previous study on mental health problems during an acute infection outbreak in our country, so special attention should be paid to infection control and ethics. Second, there was a tendency for respondents to be limited to a few organizations, as confirmed cases of COVID-19 were treated only at the NCCD at the beginning of the sporadic and cluster periods and close contacts with confirmed cases and isolated cases of underlying comorbidities were observed and isolated in other medical facilities. Third, the printed questionnaires with research information could not be removed from inside the facility under the infection control regime, there was limited access to the staff at the facility due to limited internal and external networks and there were possible ethical issues related to privacy. Additionally, the data of this study were collected from July through December 2020, so more data were gathered from respondents who worked during the sporadic period than from those who worked during the cluster period of the COVID-19 pandemic. Finally, it was not possible to fully determine whether the psychiatric symptoms and burnout experienced by health care workers were present before the COVID-19 pandemic or whether these symptoms emerged during the pandemic.
Conclusion
Burnout syndrome among frontline health care workers in the COVID-19 pandemic was not more strongly associated with any period of the pandemic, but it represented nearly 2.5-5.1 fold increased risks related to their work experience, fear of infection, depression, high impact of severe stress and immune suppression due to the impact of severe stress.
References
- Siddaway AP (2020) Multidisciplinary research priorities for the COVID-19 pandemic. Lancet Psychiatry 7: 43.
- Lima CKT, Carvalho PMM, Lima IAAS, Saraiva SJ, Souza RE, et al. (2020) The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res 287:
- Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, et al. (2020) Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7: 228-229.
- Röhr S, Müller F, Jung F, Apfelbacher C, Seidler A, et al. (2020) Psychosoziale Folgen von Quarantänemaßnahmen bei schwerwiegenden Coronavirus-Ausbrüchen: E in Rapid Review [Psychosocial impact of quarantine measures during serious Coronavirus outbreaks: A rapid review]. Psychiatr Prax 47: 179-189.
- Albott CS, Wozniak JR, McGlinch BP, Wall MH, Gold BS, et al. (2020) Battle buddies: Rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesth Analg 131: 43-54.
- Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, et al. (2020) The mental health of healthcare workers in the COVID-19 pandemic: A systematic review [Published online ahead of print, 2020 Oct 26]. J Diabetes Metab Disord 1967-1978.
- Restauri N, Sheridan AD (2020) Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: Intersection, impact and interventions. J Am Coll Radiol 17: 921-926.
- Khasne RW, Dhakulkar BS, Mahajan HC, Kulkarni AP (2020) Burnout among healthcare workers during COVID-19 pandemic in India: Results of a questionnaire-based survey. Indian J Crit Care Med 24: 664-671.
- Reynolds DL, Garay J R, Deamond SL, Moran MK, Gold W, et al. (2008) Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect 136: 997-1007.
- Wu P, Fang Y, Guan Z, Fan B, Kong J, et al. (2009) The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception and altruistic acceptance of risk. Can J Psychiatry 54: 302-311.
- Yoon M-K, Kim S-Y, Ko H-S, Myung SL (2016) System effectiveness of detection, brief intervention and referral to treatment for the people with post-traumatic emotional distress by MERS: A case report of community-based proactive intervention in South Korea. Int J Ment Health Syst 10: 51.
- Roy A, Singh A, Mishra S, Chinnadurai A, Mitra A, et al. (2020) Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry.
- Wright J (2020) How to identify the stages of grief in COVID-19 messages - PR Daily.
- O'Connor MF (2019) Grief: A brief history of research on how body, mind and brain a dapt. Psychosom Med 81: 731-738.
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, et al. (2020) The psychological impact of quarantine and how to reduce it: A rapid review of the evidence. Lancet 395: 912-920.
- Kluge HNP (2020) Statement-physical and mental health key to resilience during COVID-19 pandemic. WHO (World Health Orginasation), Goa, Switerzland.
- Spitzer RL, Kroenke K, Williams JBW, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 166: 1092-1097.
- Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 16: 606?613.
- Weiss DS (2007) The Impact of event scale: Revised. In: Wilson JP, Tang CS (eds.). Cross-cultural assessment of psychological trauma and PTSD (1st edn). Spinger, New York city, New York, USA. Pg no : 219-238.
- Maslach C. Jackson SE, Leiter MP (1996) Maslach Burnout Inventory Manual(3rded).Consulting psychologists press, USA.
- Cui J, Li F, Shi Z-L (2019) Origin and evolution of pathogenic coronaviruses. Nat rev microbiol 1: 181-192.
- Cheng SK-W, Tsang JS-K, Ku K-H, Wong C-W, Ng Y-K (2004) Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: a series of 10 cases. Br J psychiatry 184: 359-360.
- Lancee WJ, Maunder RG, Goldbloom DS (2008) Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr serv 59: 91-95.
- Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, et al. (2004) Psychosocial effects of SARS on hospital staff: a survey of a large tertiary care institution. CMAJ 170: 793-798.
- Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA (2016) Healthcare worker’s emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clinical medicine & research 14: 7-14.
- Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry 7: 300-302.
- Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, et al. (2003) The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Canadian medical association journal 168: 1245-1251.
- Fawaz M, Samaha A (2020) The psychosocial effects of being quarantined following exposure to COVID-19: A qualitative study of Lebanese health care workers. The International journal of social psychiatry. 66: 560-565.
- Wang C, Pan R, Wan X, Tan Y, Xu L, et al. (2020) Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J environ res public health 17: 1729.
- Bohlken J, Schömig F, Lemke MR, Pumberger M, Riedel-Heller SG (2020) COVID-19 Pandemic: Stress Experience of Healthcare Workers - A short current review. Psychiatr Prax 47: 190-197.
- Hou Y, Zhou Q, Li D, Guo Y, Fan J, et al. (2020) Preparedness of Our Emergency Department During the Coronavirus Disease Outbreak from the Nurses' Perspectives: A Qualitative Research Study. Journal of emergency nursing 46: 848-861.
- Maslach C, Jackson SE (1981) The measurement of experienced burnout. J Organ Behav 2: 99-113.
- Shanafelt TD, Bradley KA, Wipf JE, Back AL (2002) Burnout and self-reported patient care in an internal medicine residency program. Ann intern med 136: 358-367.
- Dewa CS, Loong D, Bonato S, Trojanowski L (2017) The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open 7: 015141.
- McManus IC, Winder BC, Gordon D (2002) The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 359: 2089-2090.
- Brown SD, Goske MJ, Johnson CM (2009) Beyond substance abuse: stress, burnout and depression as causes of physician impairment and disruptive behavior. J am coll radiol 6: 479-485.
- Balch CM, Freischlag JA, Shanafelt TD (2009) Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch surg 144: 371-376.
- Tan BYQ, Kanneganti A, Lim LJH, Sim K, Chan YH, et al. (2020) Burnout and Associated Factors Among Health Care Workers in Singapore During the COVID-19 Pandemic. J am med dir assoc 21: 1751-1758.
- Coughlan C, Nafde C, Khodatars S, Jeanes AL, Habib S, et al. (2020) COVID-19: lessons for junior doctors redeployed to critical care. Postgrad med J 97: 188-191.
- Bianchi R, Schonfeld IS, Laurent E (2015) Is it time to consider the “burnout syndrome” a distinct illness? Front. public health3:158.
- Bridgeman PJ, Bridgeman MB, Barone J (2018) Burnout syndrome among healthcare professionals. Am J health syst pharm 75:147-152.
- Halbesleben JR, Rathert C (2008) Linking physician burnout and patient outcomes: Exploring the dyadic relationship between physicians and patients. Health Care Manage Rev 33: 29-39.
- Hewitt DB, Ellis RJ, Chung JW, Cheung EO, Moskowitz JT, et al. (2020) Association of surgical resident wellness with medical errors and patient outcomes. Ann Surg 8.
- Martin F, Poyen D, Bouderlique E, Gouvernet J, Rivet B, et al. (1997) Depression and burnout in hospital health care professionals. Int J Occup Environ Health 3: 204-209.
- Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, et al. (2008) Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 149: 334-341.
- Rothenberger DA (2017) Physician burnout and well-being: A systematic review and framework for action. Dis Colon Rectum 60: 567-76.
- Stehman CR, Testo Z, Gershaw RS, Kellogg AR (2019) Burnout, drop out, suicide: Physician loss in emergency medicine, part I. West J Emerg Med 20: 485-94.
- Toker S, Shirom A, Shapira I, Berliner S, Melamed S (2005) The association between burnout, depression, anxiety and inflammation biomarkers: C-reactive protein and fibrinogen in men and women. J Occup Health Psychol 10: 344-62.
- Melamed S, Shirom A, Toker S, Berliner S, Shapira I (2006) Burnout and risk of cardiovascular disease: Evidence, possible causal paths and promising research directions. Psychol Bull 132: 327-53.
- Elhadi M, Msherghi A, Elgzairi M, Alhashimi A, Bouhuwaish A, et al. (2020) Burnout syndrome among hospital healthcare workers during the COVID-19 pandemic and aivil war: A cross-sectional study. Front. Psychiatry11: 579563.
- Duarte I, Teixeira A, Castro L, Marina S, Ribeiro C, et al.(2020) Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health20: 1885.
Citation: Munkh E, Luvsannyandag B, Oyunsuren D, Naranzul D, Oyungerel R, et.al (2021) Burnout of Frontline Health Care Workers Working during Sporadic and Cluster Periods of the COVID-19 Pandemic: A Comparative Study. J Psychiatry Depression Anxiety 7: 41
Copyright: © 2021 Munkh E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.