
Edema Palpebral Revealing in a Dermatobia hominis Infection: A Case Report
*Corresponding Author(s):
Diomandé IADepartment Of Ophthalmology, Center Hospital University Of Bouaké, Cote D'Ivoire
Tel:+225 46804233 / +225 03123230,
Email:diomandgosse@ymail.com
Abstract
Myiasis due to Dermatobia homisis is a dermatological affection that infects both animals and humans. Its location is variable but preferentially, it touches the discovered areas. It is a disease that is preferentially rampant in developing countries. Our work reports a case identified in a city of West Africa (Bouake in Cote d’ivoire). This clinical presentation reflects the comorbidities factors that sometimes favor the evolution of pathologies towards complications.
Keywords
INTRODUCTION
CASE REPORT
On clinical examination the patient had visual acuity from a long distance without correction of 10/10 in both eyes and read Parinaud 6 in near vision. Just as ocular motility and convergence were normal. Slit lamp examination noted a diffuse conjunctival hyperemia in the Right Eye (RE) associated with red eyelid edema located at the free edge of the upper eyelid. This examination made it possible to objectify blepharitis with intense inflammation of the free edge of the upper eyelid. Before the extraction of the macaque worm (Figure 1).
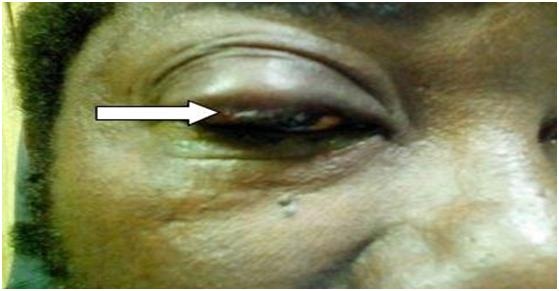
Figure 1: Eye showing signs of conjunctival hyperemia associated with red eyelid edema and the worm‘s head in a circular hole before the extraction at the free edge of the upper eyelid.
At this level there was an orifice allowing intermittently perceiving the head of the larva, which at each retraction allowed a non-purulent yellow exudates. The anterior and posterior segments were without particularity. Examination of the controlateral eye was normal. Furthermore, no satellite lymphadenopathy was noted at loco regional examination.
The general state of the patient as well as the vegetative constants was without particularity. We proceeded to extract the pathogen through the orifice mechanically by digital pressure of the palpebral rim.
The pathogen extracted had the appearance of a voluminous “maggot” of greyish coloring and had left an orifice (Figures 2&3).

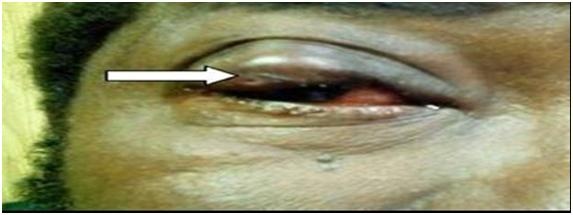
Parasitological examination permitted to confirm that it was Dermatobia hominis or “macaque worm”. Treatment after the parasite extraction included antibiotic ointment, oral anti-inflammatory and anti-tetanus vaccine. The evolution was simple at the 3rd day with a disappearance of symptoms and the scarring of the orifice left by the macaque worm.
DISCUSSION
The localization of myiasis is general ubiquitous but preferentially it touches the discovered zones (the thigh, the breast, the back, or the face) [6,7].
As observed in our patient the facial location is Palpebral. Thus any persistent Palpebral edema should be the subject of a careful ophthalmological examination because it can sometimes mask an ophthalmological or severe general pathology. The poorness of paraclinical investigations confirming the diagnosis of Palpebral affections requires a rigorous interrogation in search of anamnestic arguments and a detailed clinical examination in order to make an accurate diagnosis [7].
In our patient we found a notion of eyelid bite during a stay in the Guyanese forest thus reflecting a contact with the vector agent. This fact would confirm the epidemiological argument in favor of a Dermatobia hominis Palpebral infection.
This argument is in accordance with the literature, for various authors have confirmed the high frequency of this furuncular in South America [1,4]. The oculo-adnexal involvement of the myiasis has also been described by several authors, also Suzzoni and col. found a case of ophthalmomiasis in the area of Toulouse (France) [8] the same report made by Dorchies and col. in Djibouti [9].
The myiases observed around the world are most often cases exported from South America, because according to Clyti and col. a case out of 190 tourists would be infected during their stay in South America [1,10].
The treatment of Dermatobia hominis myiasis is essentially based on the mechanical extraction of larvae. The risk of aesthetic damage exists, especially in women. However a treatment based on the deprivation of the larva in oxygen by application of Vaseline on the orifice of the lesion could prevent this damage. Also the mechanical extraction of larvae can be facilitated by intralesional injection of lidocaine and the prior application of a 1% ivermectin solution [11,12].
CONCLUSION
REFERENCES
- Clyti E, Pages F, Pradinaud R (2008) Le point sur Dermatobia hominis myiase «furonculeuse» d'Amérique du sud. Méd Trop 68: 7-10.
- Hohenstein EJ, Buechner SA (2004) Cutaneous myiasis due to Dermatobia hominis. Dermatology 208: 268-270.
- Hochedez P, Caumes E (2018) Common skin infections in travelers. J Travel Med 15: 252-262.
- Schwartz E, Gur H (2002) Dermatobia hominis myiasis, an emerging disease among travelers to the Amazon basin of Bolivia. J Travel Med 9: 97-99.
- Roberts LS, Janovy J (2000) Gerald D. Schmidt & Larry S. Robert’s foundations of parasitology (6thedn). McGraw-Hill Education, New York, USA.
- Robbins K, Khachemoune A (2010) Cutaneous myiasis: a review of the common types of myiasis. Int J Dermatol 49: 1092-1098.
- Dicko A, Faye O, Traore P, Coulibaly K, Sagara H, et al. (2009) Myiase Furonculeuse : Un Nodule Douloureux Tropical a Ne Pas Meconnaitre. Mali Med: 75-76.
- Suzzoni-Blatger J, Villeneuve L, Morassin .B, Chevallier J (2000) A case of external human ophthalmomyiasis Oestrus ovis in Tolouse (France).J Fr Ophtalmol 23: 1020-1022.
- Dorchies PP, Larrouy G, Deconinck P, Chantal J (1995) L'ophtalmomyiase externe humaine: revue bibliographique à propos de cas en République de Djibouti. Bull Soc Path Exot 88: 86-89.
- Kaoueh E, Kallel K, Belhadj S, Chaker E (2010) Myiase furonculeuse à Dermatobia hominis au retour d'Amérique du sud: premier cas importé en Tunisie. Méd Trop 70: 135-136.
- Boggild AK, Keystone JS, Kain KC (2002) Furuncula rmyiasis: a simple and rapid method for extraction of intact Dermatobia hominis larvae. Clin Infect Dis 35: 336-338.
- Loong PT, Lui H, Buck HW (1992) Cutaneous myiasis: a simple and effective technique for extraction of Dermatobia hominis larvae. Int J Dermatol 31: 657-659.
Citation: Diomandé IA, Diomandé GF, Dossa JB, Bilé PEFK, Diabaté Z, et al. (2019) Edema Palpebral Revealing in a Dermatobia hominis Infection: A Case Report. J Ophthalmic Clin Res 6: 048.
Copyright: © 2019 Diomandé IA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

