
Eye Position Changes Under General Anesthesia in Infantile Strabismus: Differences Between Esotropia and Exotropia
*Corresponding Author(s):
Chiara FariselliOphthalmology Unit, Santa Maria Della Scaletta Hospital, Via Montericco, 4 - 40026 Imola (Bologna), Italy
Email:fariselli.chiara@gmail.com
Abstract
Purpose: To study the different trends of eye position changes under narcosis in Infantile Intermittent Exotropia (IXT) compared to Infantile Esotropia (ET). To discuss the possible causes of the difference.
Methods: Twenty-nine patients, aged 2 to 15 years, undergoing surgery for infantile concomitant strabismus at University Eye Clinic of Bologna, between January 2017 and December 2019, took part in this prospective study. Of them, 13 had basic or simulated divergence excess IXT and 16 had ET. Eye position was measured preoperatively and under general anesthesia with a modified Paliaga Test for the measure of interlimbal distance (ILD). In IXT patients the prolonged occlusion test was performed preoperatively. Neuromuscular blocking agents were not used to induce general anaesthesia.
Results: In IXT patients the difference between preoperative and intraoperative ILD was not statistically significant (Wilcoxon, p>0.05), and showed a great variability, as under narcosis ILD decreased in 38.46%, did not change in 30.77%, and increased in 30.77% of patients; while in ET patients it increased under narcosis, with a statistical significance (Wilcoxon, p=0.002).
Conclusion: Differences in the determinants of the ocular deviation may be suspected in ET and IXT, particularly regarding the role of esotonus, that is the baseline innervation to the extraocular muscles which opposes the position of rest in the awake state and which is suppressed under narcosis. While esotonus is increased in ET, it could be even decreased in IXT where other innervational phenomena, like active divergence, may be involved in determining the deviation.
Keywords
Exotropia; Esotropia; Esotonus; General anesthesia; Interlimbal distance
INTRODUCTION
Pathogenesis of childhood concomitant strabismus is still little known, though various studies have investigated its primum movens postulating new hypotheses [1], and several possible risk factors have been identified [2,3]. In the onset and development of infantile concomitant strabismus there is a sharing of both hereditary and environmental factors. Accommodative and non-accommodative innervational causes have been thought to be somehow implicated in the pathogenesis of concomitant strabismus a long time ago [4]. The innervational factors which may concur to ocular misalignment include: accommodation that may be over- or under- stimulated also in relation to refractive errors, convergence that is linked to accommodation with an innate relationship, proximal convergence, and fusional convergence and divergence.
Beside these innervational factors also tonic convergence, the so-called esotonus, has been more recently suspected to be involved in the origin of Infantile Esotropia (ET). Esotonus is the result of the baseline innervation of the extraocular muscles in the waking state which opposes the normal position of rest of the eyes [5] which is generally believed to be one of slight divergence [6]. The term esotonus seems to be more correct than that of tonic convergence, because while convergence is an active binocular function driven by the sensory input, esotonus is a passive discharge that resets the anatomic position of rest of the eyes [7] and maintains roughly a binocular alignment in the waking state in normal people, even in the absence of sensory input, for example in the darkness. It arises from firing of the reticular formation in the brainstem during the waking state. Excessive esotonus somehow induced by unbalanced visual input at an early age has been hypothesized to be a cause of ET or a factor opposing to divergence in Intermittent Exotropia (IXT) [1,5,7-12].
The absolute position of rest of the eyes can be equated with their anatomical position under general anesthesia [13,14]. Eye position under narcosis in both orthophoric and strabismus patients has been reported to be one of divergence or less convergence in ET patients [15]. On the other hand, the effects of narcosis on the eye position in Exotropia (XT) patients are less linear [15,16]. The neurotransmission to the extraocular muscles is slowed down and blocked during general anesthesia, so esotonus and the other innervational factors which may influence the eye position, i.e, accommodation, accommodative convergence to accommodation ratio (AC/A) and fusional movements, are suspended and the eyes assume their position of rest [16,17]. A lot of studies analyzed the eye position under general anesthesia in young and adult strabismic patients, but in most of them neuromuscular blocking agents have been used to induce narcosis and it is well known that such drugs, mostly depolarizing agents, may influence the tonus of the extraocular muscles and probably the eye position [18].
Data from literature make necessary a deeper evaluation of the relationship in IXT between eye position in the waking state and that under general anesthesia in absence of neuromuscular blocking agents. In the current study, the change of eye position under narcosis in infantile IXT patients has been analyzed, and compared with that of infantile ET patients. Basing on the assumption that esotonus is exaggerated in infantile ET [7,8,12], the aim of the study was to investigate if a difference in the possible determinants of ocular deviation exists between IXT and ET, namely if in IXT unlike ET esotonus may be defective or if a role of an active divergence mechanism may be postulated in divergent congenital strabismus.
MATERIALS AND METHODS
This prospective study includes 29 patients operated for concomitant strabismus at the University Eye Clinic of St. Orsola-Malpighi Hospital, Bologna, Italy, between January 2017 and December 2019. The inclusion criteria were concomitant strabismus and 15 years or less of age to limit errors due to muscle contracture. We excluded patients with coexistent restrictive or paralytic strabismus, vertical strabismus, previous extraocular muscle surgery, history of orbital trauma, other ophthalmic, neurological or systemic diseases that could affect ocular alignment, and patients in whom neuromuscular depolarizing and non-depolarizing blocking agents were used. Thirteen patients were affected by infantile IXT and 16 patients by infantile ET. This study and data collection conformed to the local laws. All patients’ parents gave informed written consent after the purpose of the study was explained and the procedure conformed to the tenets of the Declaration of Helsinki. Informed written consent to use patients’ photographs for research purpose and to be published was obtained during the preoperative visit.
In the first part of the study the 29 patients (14 females and 15 males), aged 2 to 15 years, underwent comprehensive ophthalmological and orthoptic examination the day before surgery. During this visit, all patients underwent a careful measurement of the angle of strabismus in Prism Diopters (PD), using a very dissociating alternate cover test with Berens horizontal prism bar. All measurements during the dissociating alternate cover test were taken through the full optical correction at distance fixation, thus the influence of innervational factors others than esotonus, i.e. accommodation, accommodative convergence to accommodation ratio (AC/A), and fusional movements, was minimized. In each group, patients were distinguished according to the amplitude of the angle of strabismus. In particular, the term “small squint angle” has been assigned to the exo- esodeviations with an angle ≤ 30 PD at distance fixation, and the term “large squint angle” has been assigned to the exo- esodeviations with an angle ≥ 35 PD at distance fixation. Then, a modified Paliaga Test was performed by the same investigator (C.S.) for all patients, in order to test the Interlimbal Distance (ILD) between the two eyes in millimeters with the patient fixating at distance. During this test the examiner was on the right of the patient, who fixed a letter or a figure five meters away. The examiner put a millimetric ruler on the level of the eyebrow arch without any inclination. The measurement was carried out starting from the lateral limbus of the fixing eye (normally the preferred eye) to the nasal limbus of the deviated eye in exotropia patients, and from the nasal limbus of the fixing eye to the temporal limbus of the deviated eye in esotropia patients. The measurement was performed in this way, and not nasal to nasal or temporal to temporal limbus, in order to have a clearly visible limbus available for the measurement in the deviated eye also in patients with large deviations. The measurement was repeated three times by the same investigator (C.S.) and the mean of the three measurements was recorded. During the same preoperative visit, IXT patients underwent also the prolonged occlusion test, in order to interrupt the fusional mechanism. The test consisted of the bandage of the deviated eye for 30 minutes. After the prolonged occlusion test the modified Paliaga Test for distance fixation and the prism and cover test for distance and near were quickly repeated in order to avoid the recovery of fusional convergence.
In the operating room, general anesthesia was induced by following two protocols, according to age: patients older than 3 years received venous/inhalation Balanced General Anesthesia (BGA) with propofol, fentanyl, and sevoflurane; children younger than 3 years received Inhaled General Anesthesia (IGA) with sevoflurane. The dosage of drugs varied based on age and weight of the patient, and the depth of anesthesia was assessed by monitoring the Minimum Alveolar Concentration (MAC) or by Bispectral Index (BIS) monitor. Narcosis was induced for a mean surgery duration of 40 minutes, i.e. 20 minutes per muscle (bilateral medial rectus recession in ET patients and unilateral medial rectus duplication plus lateral rectus recession in IXT patients). Six minutes after the induction of general anesthesia, the Paliaga Test was repeated before starting surgery. The measurement was carried out by the same investigator (C.S.), with the same ruler and following the same scheme used in the preoperative visit. The examiner was at the head of the patient and the eyelids were kept up manually by a second operator. The measurement was quickly repeated three times by the same investigator (C.S.), within a minute, and the mean of the three measurements was recorded.
STATISTICAL ANALYSIS
Statistical analysis was performed using the SPSS statistics software package (SPSS, Chicago, Illinois, USA) version 22. Nonparametric analyses were performed due to the small sample size. Regarding the comparisons among paired data, the nonparametric Wilcoxon signed ranks test was applied (related samples). Regarding the comparisons among groups, the nonparametric Mann-Whitney U-test was applied (independent samples). The Spearman’s coefficient ρ was used for correlations. For all statistical tests, the same level of significance was used (p < 0.05).
RESULTS
The current study comprised an IXT group of 13 patients (6 males and 7 females), with a mean age at surgical intervention of 8.46 ± 3.33 years (mean ± standard deviation) (range: 3 to 15 years), and an ET group of 16 patients (9 males and 7 females), with a mean age at surgical intervention of 5.44 ± 2.83 years (range: 2 to 11 years).
Squint angle and ILD of IXT group and ET group are reported in table 1. According to Duane’s classification, IXT patients belonged to “basic exodeviation” or “simulated divergence excess pattern”. No patient had convergence insufficiency or true divergence excess. In these patients the prolonged occlusion test was performed and no significant difference was found between the ILD before and after the occlusion test (Wilcoxon, p>0.05). Thus, changes in ILD passing from the waking state after the occlusion test to the unconscious state under general anesthesia were statistically analyzed. A remarkable variability of results was observed and, specifically, ILD under general anesthesia decreased in 5 out of 13 patients (38.46%), did not show any change in 4 patients (30.77%), and increased in 4 patients (30.77%) (Figure 1). The total difference between the alert state and the general anesthesia state was not statistically significant in IXT patients (Wilcoxon, p>0.05). (Figure 2a).
|
Patients |
Squint Angle (PD) |
Interlimbal Distance (mm) |
|||||
|
In the alert state |
Under general anesthesia
|
||||||
|
Before the occlusion test |
After the occlusion test |
Before the occlusion test |
After the occlusion test |
||||
|
At distance fixation |
At near vision |
At distance fixation |
At near vision |
||||
|
Intermittent exotropia patients |
-33.46 ± 6.58 |
-31.15 ± 6.50 |
-33.46 ± 6.58 |
-33.46 ± 6.25 |
60.12 ± 6.30 |
60.42 ± 5.60 |
60.04 ± 4.96 |
|
Esotropia patients |
+35 ± 8.11 |
+35.75 ± 8.97 |
- |
- |
48.22 ± 6.58 |
- |
53.31 ± 7.15 |
Table 1: Squint angle and interlimbal distance of exotropia and esotropia patients, presented as mean ± standard deviation. Abbreviations: PD - Prims Diopters; mm - Millimeters.
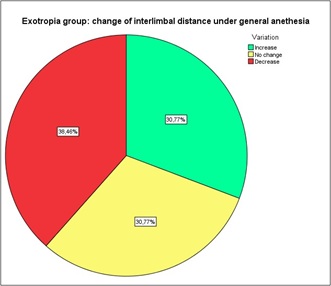 Figure 1: Change of interlimbal distance under general anesthesia in exotropia patients. 38.46% of exotropic patients showed a decreased, 30.77% an increased, and 30.77% the same interlimbal distance under general anesthesia, compared to the waking state.
Figure 1: Change of interlimbal distance under general anesthesia in exotropia patients. 38.46% of exotropic patients showed a decreased, 30.77% an increased, and 30.77% the same interlimbal distance under general anesthesia, compared to the waking state.
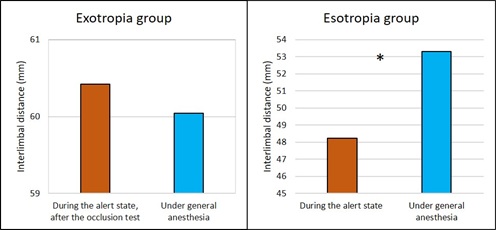 Figure 2: Difference between the interlimbal distance measured in the preoperative visit and that measured under general anesthesia. a) Difference between the interlimbal distance measured in the preoperative visit after the occlusion test and that measured under general anesthesia in exotropia patients. The difference was not statistically significant (Wilcoxon, p>0.05). b) Difference between the interlimbal distance measured in the preoperative visit and that measured under general anesthesia in esotropia patients. The asterisk shows that the difference was statistically significant (Wilcoxon, p=0.002).
Figure 2: Difference between the interlimbal distance measured in the preoperative visit and that measured under general anesthesia. a) Difference between the interlimbal distance measured in the preoperative visit after the occlusion test and that measured under general anesthesia in exotropia patients. The difference was not statistically significant (Wilcoxon, p>0.05). b) Difference between the interlimbal distance measured in the preoperative visit and that measured under general anesthesia in esotropia patients. The asterisk shows that the difference was statistically significant (Wilcoxon, p=0.002).
Regarding ET group, in 14 out of 16 patients (87.50%) the ILD increased under general anesthesia; in 1 patient (6.25%) the ILD didn’t show any change; and in 1 patient (6.25%) the ILD decreased (Figure 3). In infantile ET group, the difference between the ILD measured at distance fixation in the preoperative visit and that measured under general anesthesia was found to be statistically significant (Wilcoxon, p=0.002) (Figure 2b).
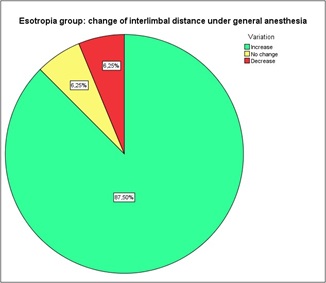 Figure 3: Change of interlimbal distance under general anesthesia in esotropia patients. 87.50% of esotropic patients showed an increased, 6.25% a decreased, and 6.25% the same interlimbal distance under general anesthesia, compared to the waking state.
Figure 3: Change of interlimbal distance under general anesthesia in esotropia patients. 87.50% of esotropic patients showed an increased, 6.25% a decreased, and 6.25% the same interlimbal distance under general anesthesia, compared to the waking state.
The difference of the ILD between IXT and ET patients was found to be statistically significant in the alert state (Mann-Whitney, p<0.001), and also under general anesthesia (Mann-Whitney, p=0.009). The change in the ILD between the awake state and under narcosis was significantly different between IXT and ET patients (Mann-Whitney, p=0.04) (Figure 4).
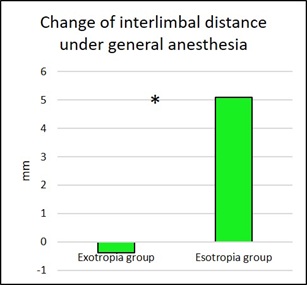 Figure 4: Change of interlimbal distance under general anesthesia between exotropia and esotropia patients. The asterisk shows that the change in interlimbal distance between the awake state and that under narcosis is significantly different between infantile intermittent exotropia and infantile esotropia patients (Mann-Whitney, p=0.04).
Figure 4: Change of interlimbal distance under general anesthesia between exotropia and esotropia patients. The asterisk shows that the change in interlimbal distance between the awake state and that under narcosis is significantly different between infantile intermittent exotropia and infantile esotropia patients (Mann-Whitney, p=0.04).
Two correlations were analyzed: between the age at surgical intervention and the change of the ILD, and between the preoperative squint angle at distance in PD and the change of the ILD. Non statistically significant correlations were found, either in IXT or in ET group (p>0.05).
Finally, comparisons of the ILD measured in the preoperative visit with that measured under general anesthesia were performed distinguishing patients according to the amplitude of the angle of strabismus. ET patients with a “small squint angle” (6 patients, 3 females and 3 males) presented a statistically significant difference between ILD measured in the alert state and that measured under general anesthesia (Wilcoxon, p = 0.04). This statistical significance was stronger in ET patients with a “large squint angle” (9 patients, 4 females and 5 males) (Wilcoxon, p = 0.02). Otherwise, in IXT patients there was no statistically significant difference between the preoperative ILD and that measured under narcosis, either for patients with a “small squint angle” (5 patients, 2 females and 3 males) or for patients with a “large squint angle” (8 patients, 5 females and 3 males) (Wilcoxon, p>0.05).
DISCUSSION
The present study analyzed the relationship between eye position in the awake state and that under general anesthesia in infantile IXT compared to infantile ET in a manner that made it possible to minimize measurement errors. To get comparable results, and to reduce the error due to the use of different methods for eye position measurement, we standardized the procedure which was the same in the awakened state and under general anesthesia. In this way, data collection of eye position in the two conditions is more accurate and makes it possible to do more reliable comparisons than when using, for example, the cover test in the awake state and the Hirschberg/Krismky prism test under narcosis [19]. Using a general anesthesia without both depolarizing and non-depolarizing neuromuscular blocking agents eliminated any bias due to the action of these drugs on the neuromuscular junction. Considering only young patients prevented to get results distorted by muscle contracture. The change in the ILD between the awake state and the state under narcosis was significantly different between infantile IXT and infantile ET patients (p = 0.04). Moreover, a remarkable variability of results was found in IXT patients, in contrast with a more uniform behavior in ET. In fact, under general anesthesia in IXT patients the divergence of the visual axes decreased in 38.46%, did not change in 30.77%, and increased in 30.77%. Conversely, ET patients showed a statistically significant increase in the ILD under general anesthesia (p = 0.002). This different behavior of infantile IXT and infantile ET patients under general anesthesia requires us to make some considerations.
The global tonus acting on the extraocular muscles and determining the eye position has two main components: the tonus driven by the sensory input including accommodation, convergence, motor and proximal fusion; and a baseline tonus of non-retinal origin which allows a certain grade of ocular alignment or misalignment in the waking state in absence of sensory input. The tonus driven by the sensory input can be suppressed in the awake patient by a dissociating cover test at distance fixation, with the refractive error fully corrected, eventually after a prolonged monocular occlusion in exotropia patients, leaving the baseline tonus as the only innervational factor determining the awake eye position in such conditions. General anesthesia suspends the global tonus and this causes an exo-shift in both normals and ET patients, whereas in IXT patients the effect is variable. It has been postulated that the baseline tonus acting upon the extraocular muscles results from divergence and convergence of non- retinal origin, and an alteration in the general level of non-retinal ocular tonus may cause mechanically disjunctive horizontal eye movements [7]. When the general level of this tonus is increased or decreased, the medial rectus muscles have greater gain or loss in mechanical effect than the lateral rectus muscles [7]. As reported by many authors, esotonus is suspected to be increased in infantile ET [7-12]. If during the period of neuroplasticity of the visual system the two eyes lose their perfect coupling, the baseline innervation so-called esotonus takes over and a convergent strabismus can develop [7,9,10]. This happens in case of unilateral visual loss early in life, the so-called “functional monophthalmic syndrome” [11], and in essential infantile esotropia which can be assimilated to a double monophthalmic syndrome. During general anesthesia, the neurotransmission to the extraocular muscles is slowed down and blocked [16,17], and the effect of shutting off the tonus to all the muscles produces a greater decrement in the mechanical effect of the medial rectus muscles than of the lateral rectus muscles, with a resultant slight to moderate exodeviation [7]. In the same way, during sleep, death and blindness the eyes are divergent [20]. According to some authors, under general anesthesia the loose of the tension of the extraocular muscles [21] and the block of the neurotransmission allow the eyes to acquire the divergent position also due to the anatomical morphology of the orbital structure [17], which manifests as a residual divergence of the orbital axis [22].
It has been postulated that when an unequal visual input derives from the two eyes early in life, dissociated, i.e., driven by unbalanced visual input, ocular movements are generated. The monocular fixation allows the primitive tonus system to induce a “convergent” position of the visual axes that, depending on the baseline anatomical position of the eyes, can manifest as an intermittent exodeviation or an intermittent esodeviation [5]. When esotonus is superimposed upon a baseline exodeviation, an intermittent exodeviation is produced [23]. But sometimes monocular fixation induces sufficient dissociated esotonus to override the baseline exodeviation, inducing an ET. According to Jampolsky’s theory on “Ocular Divergence Mechanisms”, another explanation is possible regarding IXT, distinguishing two different basic fusion-free positions for IXT patients: an exotropic position, from which a convergence mechanism operates to keep the eyes fused at parallelism; or a parallelism of the visual axes, on which an active divergence mechanism acts, carrying the eyes to exotropia [7].
Unlike previous studies [15], we did not used neuromuscular blocking agents considering that they act directly on muscle tone leading to a flaccid paralysis, and that succinylcholine induces an unpredictable contraction of the extraocular muscles after about 30 seconds from intravenous injection for at least 10 minutes [18,24]. The inhalational anesthetics used for induction and maintenance of general anesthesia (such as sevoflurane) eliminate the active muscle tone, which includes the so-called esotonus, without inducing any other muscle contraction. But narcosis is able to suppress, besides esotonus, also other innervational phenomena that contribute to the position of the visual axes in the waking state. In order to minimize the influence of these innervational factors on the eye position in the alert state, the measures of the position of the visual axes in the waking state were taken using a very dissociating alternate cover test through the full optical correction of the refractive error at distance fixation in all strabismic patients, and after prolonged occlusion of one eye in exotropia patients. In such conditions the non-retinal derived ocular tonus is probably the only determinant of the basic ocular deviation during monocular distance fixation of the dominant eye alone, without the influence of other retinal stimuli (fusion, accommodation...) [7] Like in other studies, in the current study the changes in ocular alignment following general anesthesia showed a different behavior pattern between XT and ET patients. In some studies, IXT patients have been reported to be more exotropic when deeply anesthetized than in the awake state [19,25]. In particular, the eyes of patients with dissociated horizontal deviation display a large baseline exodeviation under general anesthesia that far exceeds the exodeviation measured in the awake state. These findings suggest that monocular fixation generates a dissociated esotonus which produces a smaller intermittent exodeviation (or even an esodeviation) in the awake state [5]. Other authors, conversely, reported a non-consistent tendency in eye position under general anesthesia in exotropic patients. Ohmi et al. analyzed 80 exotropic patients and observed a wide range of eye positions under general anesthesia, from eso- to exodeviation [16]. Alike, Ku et al. found in exotropic patients a tendency toward changing eye position to different directions after anesthesia [15]. In the present study, when considering the mean values, no statistically significant difference was found in XT patients as regards eye position passing from the waking state to narcosis, as some patients showed a decreased, some an increased, and some other the same ILD under general anesthesia, compared to the waking state. This behavior pattern may be due to the existence of different types of XT, according to Duane’s classification, and to the presence of different innervational patterns involved in the various forms of XT, including not only a convergence insufficiency pattern, but also a divergence excess pattern. The effect of general anesthesia on the various innervational patterns may be different, and also the effect on the esotonus can be masked or somehow confused, depending on the drugs used and the type of anesthesia. The decrease of the ILD under general anesthesia showed by some XT patients could be explained according to Jampolsky’s theory of the existence of an active divergence mechanism [7], which should be suppressed under narcosis together with esotonus and sensory driven tonus. Finally, if it seems established that an unequal sensory input at an early age is the first causal factor for infantile ET where the esotonus gets out of control, in IXT the visual input from the two eyes can be considered balanced, at least intermittently in the early stages. So, the role of binocular sensory input on the esotonus in XT is not clear. Trying to interpret the results of narcosis on eye position in IXT, and specifically to give an explanation for the three possible responses that can be observed (i.e., exo-shift, no shift, and eso-shift), one may assume that in IXT esotonus is generally defective, because eye position does not modify on average under general anesthesia in IXT patients, unlike ET patients and also normal subjects. So, in IXT a deficiency of esotonus may be suspected as a causal factor that is the opposite of what happens in ET.
So, in IXT a deficiency of esotonus may be suspected as a causal factor that is the opposite of what happens in ET. Regarding IXT patients where even an eso-shift occurs under general anesthesia, about one third of patients in this case series, also an active divergence tonus may be supposed to be implicated in IXT.
In summary, according to Jampolsky [7], the baseline tonus acting upon the extraocular muscles results from a balance between divergence and convergence tonus of non-retinal, i.e. non-sensory, origin, and an alteration of this balance may lead to a predisposition towards convergent or divergent strabismus.
CONFLICT OF INTEREST
The Authors declare that there is no conflict of interest.
FUNDING
The authors received no financial support for the research, authorship, and/or publication of this article.
AVAILABILITY OF DATA
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Ghadban R, Liebermann L, Klaehn LD, Holmes JM, Brodsky MC (2014) Relative roles of luminance and fixation in inducing dissociated vertical divergence. Invest Ophthalmol Vis Sci 56: 1081-1087.
- Chew E, Remaley NA, Tamboli A, Zhao J, Podgor MJ, et al. (1994) Risk factors for esotropia and exotropia. Arch Ophthalmol 112: 1349-1355.
- Cotter SA, Varma R, Tarczy-Hornoch K, McKean-Cowdin R, Lin J, et al. (2011) Risk factors associated with childhood strabismus: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology 118: 2251-2261.
- Donders FC (UK) On the anomalies of accommodation and refraction of the eye, with a Preliminary Essay on Physiological Dioptrics, The New Sydenham Society, London, UK.
- Brodsky MC (2007) Dissociated horizontal deviation: clinical spectrum, pathogenesis, evolutionary underpinnings, diagnosis, treatment, and potential role in the development of infantile esotropia (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 105: 272-293.
- Cogan DG (1956) Neurology of the ocular muscles. In: Thomas CC (ed.), Springfield, Illinois, USA.
- Jampolsky A (1970) Ocular divergence mechanisms. Trans Am Ophthalmol Soc 68: 730-822.
- Brodsky MC, Fray KJ (2007) Does infantile esotropia arise from a dissociated deviation? Arch Ophthalmol 125: 1703-1706.
- To cross or not to cross? (2006) In: Hoyt C, et al. (eds.), Proceedings of the Ocular Motor Tonus Symposium. Smith-Kettlewell Eye Research Institute, Tiberon, California, USA.
- Jampolsky A (1978) Unequal visual inputs in strabismus management: A comparison of human and animal strabismus. In: Symposium on Strabismus: Transactions of the New Orleans Academy of Ophthalmology. St Louis, MO: CV Mosby: 422-425.
- Spielmann A (1987) Adduction, latent nystagmus, infantile strabismus and the opto-motor syndrome of congenital uniocular organic amblyopia. In: Kaufmann H (ed.), Proceedings of the 16th Meeting of the European Strabismological Association. Giessen, Germany: 291-294.
- Brodsky MC, Gräf MH, Kommerell G (2005) The reversed fixation test: A diagnostic test for dissociated horizontal deviation. Arch Ophthalmol 123: 1083-1087.
- Toselli C (1953) Studies on the position of absolute ocular rest in curarized subjects. Boll Ocul 32: 333-340.
- Meyers MP (1951) The position of eyes under general anesthesia. Am J Ophthalmol 34: 1749-1752.
- Ku HC, Lee SY, Lee YC (2005) Change of eye position in patients with orthophoria and horizontal strabismus under general anesthesia. Korean J Ophthalmol 19: 55-61.
- Ohmi E, Ogli K, Kani K (1979) Eye position and electromyographic observation of squint eyes under general anesthesia. Ophthalmologica 178: 166-171.
- Breinin GM (1957) The position of rest during anesthesia and sleep; electromyographic observations. AMA Arch Ophthalmol 57: 323-326.
- Lennerstrand G, Bolzani R, Tian S, Benassi M, Fusari M, et al. (2010) Succinylcholine activation of human horizontal eye muscles. Acta Ophthalmologica 88: 872-876.
- Apt L, Isenberg S (1977) Eye position of strabismus patients under general anesthesia. Am J Ophthalmol 84: 574-579.
- Grut HE (1980) A contribution to the pathogeny of concomitant squinting. Trans Ophthalmol Soc UK 10: 1.
- Burford GE (1941) Involuntary eyeball motions during anesthesia and sleep, relationship to cortical rhythmic potentials. Anesth Anal 20: 191.
- Worth C, Chavasse B (1959) Squint (9th) Bailliere Tyndal & Cox ed. London: 714-718.
- Brodsky MC, Fray KJ (2007) Dissociated horizontal deviation after surgery for infantile esotropia: Clinical characteristics and proposed pathophysiologic mechanisms. Arch Ophthalmol 25: 1683-1692.
- France NK, France TD, Woodburn JD, Burbank DP (1980) Succinylcholine alteration of the forced duction test. Ophthalmology 87: 1282-1287.
- Romano PE, Gabriel L, Bennett WL, Snyder BM (1988) Stage I intraoperative adjustment of eye muscle surgery under general anesthesia: consideration of graduated adjustment. Graefes Arch Clin Exp Ophthalmol 226: 235-240.
Citation: Fariselli C, Calzolari G, Roda M, Schiavi C (2020) Eye Position Changes Under General Anesthesia in Infantile Strabismus: Differences Between Esotropia and Exotropia. J Ophthalmic Clin Res 7: 072.
Copyright: © 2020 Chiara Fariselli, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

