
Low Vision Service Activities Review and Use of the Electronic Health Record
*Corresponding Author(s):
Paola SassoNational Centre Of Services And Research For The Prevention Of Blindness And Rehabilitation Of Visua, International Agency For The Prevention Of Blindness, IAPB Italia Onlus, Rome, Italy
Tel:+39 0635510819,
Email:pablitasax@hotmail.it
Abstract
Aim: The aim of this study was to describe two years activities in a low vision rehabilitation center based on a multidisciplinary approach by means of a new Electronic Health Record (EHR) in order to highlight the benefits.
Methods: Clinical and functional data of patients assessed at our low vision center were collected and analyzed retrospectively through the use of nLIFE, a new EHR. nLIFE is easily customizable to follow different needs and scenarios. nLIFE is updated with different modules including advanced search ability. Eye disease, National Eye Institute 25 item Visual Function Questionnaire (VFQ-25), Best Corrected Visual Acuity (BCVA), Contrast Sensitivity (CS), Fixation stability, Microperimetric retinal sensitivity, Reading Speed (RS) and aids prescribed were evaluated. All data came from different modules and tools and were processed in an ad-hoc database.
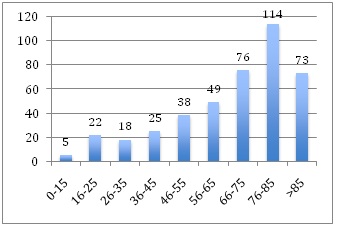
Results: A total of 420 EHRs of patients who attended the low vision center between January 2015 and December 2016 were included in the analysis. Mean age was 66.7 years (SD 20.7). Age related Macular Degeneration (AMD) was the most frequent disease with a prevalence of the atrophic one. BCVA was collected for 593 eyes with a mean of 0.89 (± 0,34) LogMAR and CS was 0.76 (± 0.41) LogC. Three hundred eight patients underwent a specialized psychological assessment. Moreover, 259 subjects completed the VFQ-25. Glare and reading were the most frequent demands.
Conclusion: EHR appears to be a valid tool for supporting clinicians. nLIFE is based on the state of the art of web technology with the possibility to receive data from different sources and multidisciplinary modules. It can review clinical and research data locally or through Internet and by using all device type.
Keywords
INTRODUCTION
Visual disability negatively impacts on daily life activities. Visually impaired became unable to perform many Activities of Daily Living (ADLs) such as reading, recognizing faces, watching television and driving resulting in a poor quality of life. According to some author’s findings, visual impairment has an effect on psychological status and quality of life and it can be related to feelings of inadequacy and higher level of depressive symptoms [2-5]. Based on clinical and psychological features of visually impaired, an holistic and multidisciplinary approach should be recommended. Our National Center of Services and Research for the Prevention of Blindness and Rehabilitation of Visually Impaired, IAPB Italia onlus, has a multidisciplinary team including psychologist, ophthalmologist, orthoptist, orientation and mobility teacher and expert in tiphlology. As our standard procedure, first of all the psychologist approaches the patient focusing on psychological status and personal demands. A complete ophthalmological examination is performed subsequently.
Considering patient’s residual visual function and needs, a customized rehabilitation program is defined. Therefore, patients can start with the devices training sessions supported by the orthoptist in order to identify and correctly use magnifying aids.
In the recent years, our team adopted an Electronic Health Record (EHR), a digital version of patient’s paper charts implemented with several tools, in order to achieve specified improvement in patient care delivery, provide more effective methods of communicating and sharing information among multidisciplinary team and better manage patient medical records as reported by other authors [6-10]. The EHR is based on an electronic medical database that resides on a web server (Figure1). Therefore, inside of an integrated health system, the EHR adoption can impact on the improvement of clinical care and research quality. Before EHR adoption our center used paper charts to collected clinical data divided in specific sections considering the different professional roles.
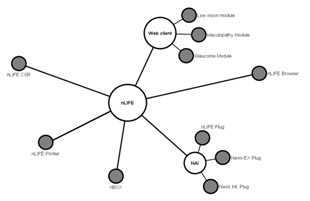
Figure 1: The architecture of the web-based electronic health record.
The aim of this study was to describe two years activities in our low vision rehabilitation center based on a multidisciplinary approach using an EHR in order to highlight the benefits of the tool and its impact on clinicians care delivering.
METHODS
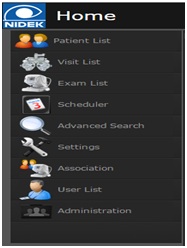
Visually impaired patients who had access to our low vision centre were informed by our staff about the likelihood of using their own clinical data for research purposes and they gave their informed consent. Clinical and functional data of patients were collected and analyzed retrospectively through the use of nLIFE, a new EHR developed by Nidek Technologies. nLIFE is easily customizable to follow different needs, scenarios from stand-alone configuration to big networks. It can communicate with different devices and automatically import the results of specific exams as microperimetry or visual field analyzer (Figure 2). The filling of information is divided on several sections in order to properly fit different kind of medical data. nLIFE is updated with different modules including advanced search ability and scheduling of resources to implement a full field approach to medical data management (Figure 3).

Figure 2: nLIFE is easily customizable to follow different needs, scenarios from stand-alone configuration to big networks.
As standard procedure, low vision assessment begins with psychological interview. The psychologist investigates patients’ psychological status and demands, motivation to start with the vision rehabilitation intervention, grief stage of disease and National Eye Institute 25 item Visual Function Questionnaire (VFQ-25). If necessary, the patient is supported by the psychologist during the whole rehabilitation pathway.
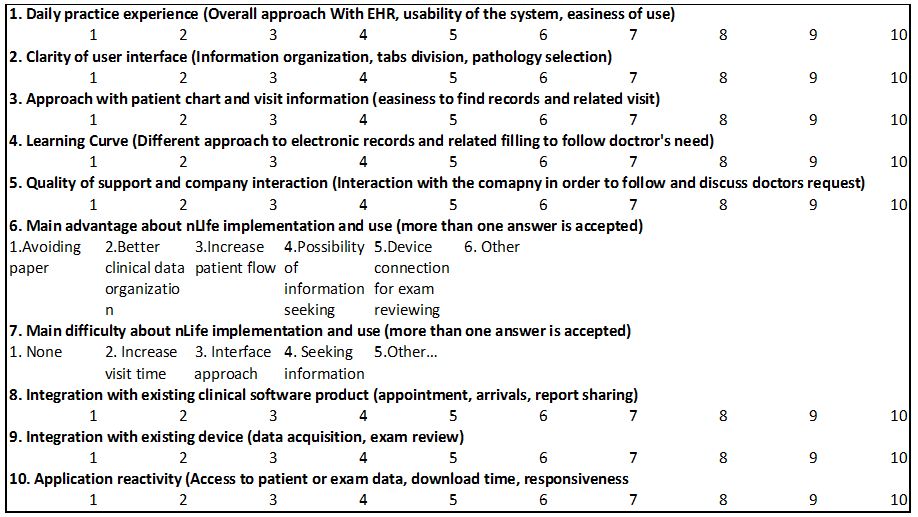
All patients underwent complete ophthalmic evaluation including BCVA using the Early Treatment Diabetic Retinopathy (ETDRS) charts (Precision Vision, Woodstock, IL, USA, IL) and recorded as logMAR at a distance of 4 meters, Slit-lamp examination, binocular ophthalmoscopy and Contrast Sensitivity (CS) measured with Pelli-Robson charts (Precision Vision, Woodstock, IL, USA, IL) adding +1 spherical diopters to the best distance correction expressed as LogC (Logarithm of Contrast), fixation stability and retinal sensitivity analyzed with the microperimeter MP1 (Nidek Technologies, Padua, Italy). Fixation stability was classified according to Fujii Classification [11] and Bivariate Contour Ellipse Area (BCEA) encompassing 1 SD, 68.2% was performed. The area of the ellipse was calculated in degrees with Steinman’s technique [12]. MP1 retinal sensitivity was automatically imported by the tool. After the multidisciplinary meeting, the team discussed the rehabilitation approaches to help people with difficulties expressed. Therefore, every patient participates to low vision training sessions. Patients who were trained to restore reading, during the last training were tested and Reading Speed (RS) with the most appropriate low vision aid was evaluated. RS was calculated as words per minute (counting the number of corrected words during 1 minute) on an Italian Newspaper text printed in a 9-point Times New Roman typeface. Patients were asked to read as quickly as possible. Once completed the rehabilitation training program; patients received the prescription of low vision devices. All data came from different modules and tools and were processed in an ad-hoc database (Figures 4A & 4B). According to inclusion criteria, nLIFE advanced research tool allowed to save and export the database into an excel file. A survey was conducted among the operators of the multidisciplinary team, in order to describe the user experience of nLIFE during practice activities. Every question was related to specific aspect about user approach, organization of information, usability, customization and support experience. About the question related to a satisfaction evaluation, the indicator was given by ten point scale, in which 1 means not satisfied at all and 10 means very much satisfied (Table 1).

RESULTS
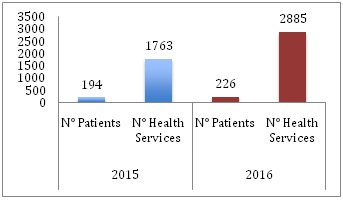
Graph 1: Distribution of both patients assessed and health services during 2015 and 2016.
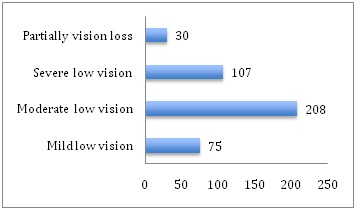
According to the Italian low vision classification (Law 238/2001), we classified patients on the basis of their residual vision. Graph 3 shows the distribution of patients for range vision loss: 208 (50%) patients had a moderate low vision, 107 (25%) had severe low vision, 75 (18%) mild low vision and 30 (7%) partially vision loss.
| Disease | N° | % |
| AMD | 171 | 41 |
| Hereditary retinal dystrophies | 61 | 15 |
| Degenerative myopia | 55 | 13 |
| Glaucoma | 28 | 7 |
| Other retinal disorders | 12 | 3 |
| Diabetic retinopathy | 22 | 5 |
| Disorders of optic nerve and visual pathways | 31 | 7 |
| Albinism | 8 | 2 |
| Cataract and corneal disorders | 6 | 1 |
| Other | 26 | 6 |
The leading cause of visual impairment among our patients was Age related Macular Degeneration (AMD) with a prevalence of the atrophic type: 113 patients (66%) were affected by the atrophic form and 58 (34%) by the exudative one.
Functional outcomes
Psychological outcomes
| EyeDisease | Grief stage | ||||
| Acceptance | Depression | Denial | Anger | Regret | |
| AMD | 46 | 53 | 1 | 8 | 20 |
| Hereditary retinal dystrophies | 21 | 10 | 4 | 7 | 2 |
| Degenerative myopia | 16 | 16 | 1 | 3 | 5 |
| Glaucoma | 8 | 3 | 1 | 4 | 4 |
| Otherretinaldisorders | 2 | 3 | 1 | 6 | 0 |
| Diabeticretinopathy | 3 | 11 | 1 | 1 | 2 |
| Disorders of optic nerve and visual pathways | 9 | 4 | 1 | 1 | 4 |
| Albinism | 4 | 2 | 0 | 1 | 0 |
| Cataract and cornealdisorders | 1 | 2 | 0 | 0 | 1 |
| Other | 9 | 5 | 1 | 0 | 0 |
During the first psychological assessment, the grief stage was defined. One hundred-nine subjects (35%) presented depressive symptoms while others 119 (39%) reported to have accepted their eye disease. Regret was found in 38 (12%) patients, anger in 31 (10%) and denial in 11 (4%). Patients were also scheduled by both eye disease and grief stage as reported in table 3. Most of the patients (48%) between those who were classified with depression symptoms had a diagnosis of AMD. Moreover, 259 subjects completed the VFQ-25 and items mean and SD were reported in table 4.
| EyeDisease | Grief stage | ||||
| Acceptance | Depression | Denial | Anger | Regret | |
| AMD | 46 | 53 | 1 | 8 | 20 |
| Hereditary retinal dystrophies | 21 | 10 | 4 | 7 | 2 |
| Degenerative myopia | 16 | 16 | 1 | 3 | 5 |
| Glaucoma | 8 | 3 | 1 | 4 | 4 |
| Otherretinaldisorders | 2 | 3 | 1 | 6 | 0 |
| Diabeticretinopathy | 3 | 11 | 1 | 1 | 2 |
| Disorders of optic nerve and visual pathways | 9 | 4 | 1 | 1 | 4 |
| Albinism | 4 | 2 | 0 | 1 | 0 |
| Cataract and cornealdisorders | 1 | 2 | 0 | 0 | 1 |
| Other | 9 | 5 | 1 | 0 | 0 |
A total of 258 patients underwent to psychological counseling and support during their vision rehabilitation pathway.
Rehabilitation data
| Needs | N° | % |
| Outside glare | 228 | 24 |
| Reading | 213 | 22 |
| Distance/ watching TV | 149 | 15 |
| Inside glare | 114 | 12 |
| Writing | 56 | 6 |
| PC | 48 | 5 |
| Using mobile phone | 47 | 5 |
| Home activities | 38 | 4 |
| Orientation and mobility | 32 | 3 |
| Knitting | 25 | 2 |
| Hobbies (bricolage, playingcards…) | 16 | 2 |
| Aids | N° | % |
| Photoselective spectral lenses | 190 | 36 |
| Video magnifiers | 107 | 21 |
| Refractive error correction | 81 | 16 |
| Hand-heldmagnifier | 84 | 16 |
| Spectacle magnifier | 38 | 7 |
| Telescopes | 14 | 3 |
| Screen magnifier /Screen reader | 6 | 1 |
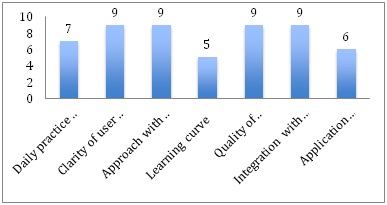
THE EXPERIENCE AND SATISFACTION SURVEY
| Main advantage about nLIFE implementation and use | Avoiding paper | Possibility of information seeking | Device Connection for exam reviewing |
| Main difficulty about nLIFE implementation and use | Increase visit time | ||
| Integration with existing clinical software product | Not applicable |
DISCUSSION
The use of EHR in different medical settings and particularly into ophthalmic practices has been limited and it has been reported that only the 34% of ophthalmology units have adopted an EHR system into the practice [8,9] in comparison to 50% of all physicians, maybe related to the particular needs of ophthalmic evaluation as drawing the ocular fundus or writing the refractive correction. We believe that all the learning difficulties for the use of the tool should be overcome also for epidemiological data analysis in consideration of the evolving need of changing population demographics, where the number of patients with visual impairment who need to access to the low vision rehabilitation center will increase. Moreover low vision rehabilitation is a sub-specialty of ophthalmology that required different professional figures involved in a multidisciplinary team as the ophthalmologist, orthoptist, psychologist, orientation and mobility teacher, with an ever-increasing impact on the concepts of research, education, and services for the visually impaired patient. The Electronic Health Record appears to be a valid tool for supporting clinicians in our multidisciplinary approach in order to collect high amounts of data, consult the different evaluations, increase patient engagement, build shared models and standardization across institutions, create new knowledge and facilitate personalized care. Moreover, the ability to combine vast amounts of data allows cross-sectional research. The low vision multidisciplinary approach involves medical and surgical care, acquisition and interpretation of imaging, high-volume documentation coming from different tools and based on numerical, text-based and imaging-based documentation.
Our study has found that in a multidisciplinary context the staff questionnaire on users’ experience reported a good daily practice experience, a satisfying clarity of user interface, approach with patient chart and visit information and integration with existing devices.
nLIFE is based on the state of the art of web technology with the possibility to receive data from different sources and different modules. The EHR was set in order to be a web and technology devices (Computer, tablet, smart phone, etc.) based on multiple disciplines information system that collects, stores and displays patient’s data. The EHR has been efficacious in improving quality of practice for reviewing clinical and research data locally or through internet and by using all type of devices. The multidisciplinary team was currently able to share exams and images directly from devices to the EHR by electronic upload. The advance search ability tool allowed to extract and export functional and clinical data in an excel sheet automatically and quickly. Moreover the multidisciplinary team was able to interact on the EHR at the same time. The use of the paper medical chart would not allow a quick extrapolation and rapid clinical processing of a large number of data. The tool reduced the operator’s error likelihood during data entry in the database and it allowed matching the items of the evaluation performed by the various professionals of the multidisciplinary team.
We easily analyzed a large number of data coming from the health records of 420 visually impaired patients reviewing 2 years activity of our low vision centre.
As reported by World Health Organization (WHO), visual impairment is highly prevalent in the worldwide and is expected to increase rapidly as the population ages [1,15,16]. Aging diseases as AMD seem to be the most common causes of low vision in the developed countries [17,18]. Our review highlights that the most of our patients (27%) had an age between 75 and 86 years, confirming the impact of the advancing age between low vision patients and the most frequent cause of low vision between our patients was AMD with a greater prevalence of the atrophic form respect to the exudative one. The other causes of low vision were represented by hereditary retinal dystrophies and pathological myopia. Matched data analysis, interestingly, showed the effect of the eye disease on the psychological status. A depression status was found more frequent in patients with a diagnosis of AMD and diabetic retinopathy compared to the other low vision causes. On the other hand, a more acceptance status revealed other visual impaired conditions such as hereditary retinal dystrophies, glaucoma and optic nerve disease. As previously described vision impairment compromises quality of life and limits social interaction and independence [19]. Most older persons with vision loss due to aging disease, reported poorer levels of functioning in ADLs, symptoms of depression and poor motivation to start with a visual rehabilitation program [20-26]. Elderly people with low vision are unable to perform ADLs, resulting in a psychological burden.
The analysis of the VFQ25 revealed that our patients expressed poor functioning in “Near activities”, “Distance activities”, “Vision specific mental Health”, “Peripheral vision” items, reflecting their own difficulties and demands. Near activity included reading ability that was the most important goal for patients examined and it was requested by 51% of the whole sample. In order to restore reading ability, a relevant number of video magnifiers CCTV (Closed Circuit Television) were prescribed. The visual acuity reduction, the high prevalence of people with AMD, who need a strong enlargement, could explain the large number of CCTV that allows reading with high level of magnification. Moreover, glare caused by scattering of light within the eye is a great deal for the patients resulting in eye discomfort and impaired visual functioning and it was another important demand expressed by our subjects. The rehabilitation solution was the use of the photo selective spectral lenses. Another important factor to be considered is the need for visually impaired to improve distance viewing and watching television and just the refractive error correction was the most suitable prescribed low vision aid for far in order to enhance the image and improve functional vision. This analysis has a limitation that should be considered: the sample size was actually small for some estimation about clinical and functional data.
CONCLUSION
REFERENCES
- Pascolini D, Mariotti SP (2012) Global estimates of visual impairment: 2010. Br J Ophthalmol 96: 614-618.
- Crews JE, Campbell VA (2001) Health conditions, activity limitations, and participation restrictions among older people with visual impairment. J Vis Impair Blind 95: 453-467.
- Horowitz A, Brennan A, Reinhardt JP (2005) Prevalence and risk factors for self-reported visual impairment among middle-aged and older adults. Research on Aging 27: 307-326.
- Desrosiers J, Wanet-Defalque MC, Témisjian K, Gresset J, Dubois MF, et al. (2009) Participation in daily activities and social roles of older adults with visual impairment. Disabil Rehabil 31: 1227-1234.
- Hayman KJ, Kerse NM, La Grow SJ, Wouldes T, Robertson MC, et al. (2007) Depression in older people: visual impairment and subjective ratings of health. Optom Vis Sci 84: 1024-1030.
- DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, et al. (2008) Electronic health records in ambulatory care--a national survey of physicians. N Engl J Med 359: 50-60.
- Kern LM, Barrón Y, Dhopeshwarkar RV, Edwards A, Kaushal R, et al. (2013) Electronic health records and ambulatory quality of care. J Gen Intern Med 28: 496-503.
- Chiang MF, Boland MV, Margolis JW, Lum F, Abramoff MD, et al. (2008) Adoption and perceptions of electronic health record systems by ophthalmologists: an American Academy of Ophthalmology survey. Ophthalmology 115: 1591-1597.
- Boland MV, Chiang MF, Lim MC, Wedemeyer L, Epley KD, et al. (2013) Adoption of electronic health records and preparations for demonstrating meaningful use: an American Academy of Ophthalmology survey. Ophthalmology 120: 1702-1710.
- Chiang MF, Boland MV, Brewer A, Epley KD, Horton MB, et al. (2011) Special requirements for electronic health record systems in ophthalmology. Ophthalmology 118: 1681-1687.
- Fujii GY, de Juan E Jr, Sunness J, Humayun MS, Pieramici DJ, et al. (2002) Patient selection for macular translocation surgery using the scanning laser ophthalmoscope. Ophthalmology 109: 1737-1744.
- Steinman RM (1965) Effect of target size, luminance, and color on monocular fixation. J Opt Soc Am 55: 1158-1165.
- Schoen C, Osborn R, Doty MM, Squires D, Peugh J, et al. (2009) A survey of primary care physicians in eleven countries 2009: perspectives on care, costs, and experiences. Health Aff (Millwood) 28: 1171-1183.
- Lau F, Price M, Boyd J, Partridge C, Bell H, et al. (2012) Impact of electronic medical record on physician practice in office settings: a systematic review. BMC Medical Informatics and Decision Making 12: 10.
- Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, et al. (2004) Global data on visual impairment in the year 2002. Bull World Health Organ 82: 844-851.
- Pascolini D, Mariotti SP, Pokharel GP, Pararajasegaram R, Etya'ale D, et al. (2004) 2002 global update of available data on visual impairment: a compilation of population-based prevalence studies. Ophthalmic Epidemiol 11: 67-115.
- Brown MM, Brown GC, Sharma S, Stein JD, Roth Z, et al. (2006) The burden of age-related macular degeneration: a value-based analysis. Curr Opin Ophthalmol 17: 257-266.
- Rubin GS (2001) Vision rehabilitation for patients with age-related macular degeneration. Eye (London, England) 15: 430-435.
- West SK, Rubin GS, Broman AT, Muñoz B, Bandeen-Roche K, et al. (2002) How does visual impairment affect performance on tasks of everyday life? The SEE Project. Salisbury Eye Evaluation. Arch Ophthalmol 120:774-780.
- Horowitz A, Reinhardt JP, Kennedy GJ (2008) Major and subthreshold depression among older adults seeking vision rehabilitation services. Am J Geriatr Psychiatry 13: 180-187.
- Grant P, Seiple W, Szlyk JP (2011) Effect of depression on actual and perceived effects of reading rehabilitation for people with central vision loss. J Rehabil Res Dev 48: 1101-1108.
- Karlsson JS (1998) Self reports of psychological distress in connection with various degrees of visual impairment. J Vis Impair Blind 92: 483-490.
- Dodds AG, Bailey P, Pearson A, Yates L (1991) Psychological factors in acquired visual impairment: The development of a scale of adjustment. J Vis Impair Blind 85: 306-310.
- Szlyk JP, Becker JE, Fishman GA, Seiple W (2000) Psychological profiles of patients with central vision loss. J Vis Impair Blind 94: 781-786.
- Rovner BW, Casten RJ (2002) Activity loss and depression in age-related macular degeneration. Am J Geriatr Psychiatry 10: 305-310.
- Bragg MW (2005) Vision loss, depression and rehabilitation. Int Congr Ser 1282: 40-41.
Citation: Sasso P, Silvestri V, Piscopo P, Amore FM (2017) Low Vision Service Activities Review and Use of the Electronic Health Record. J Ophthalmic Clin Res 4: 035
Copyright: © 2017 Paola Sasso, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

