Prioritized Redistribution of Cerebral Blood Flow for Crossed Cerebellar Diaschisis after Intravascular Laser Phototherapy in a Stroke Survivor with Prior Coronary Artery Disease
*Corresponding Author(s):
Shin-Tsu ChangDepartment Of Physical Medicine And Rehabilitation, Taichung Veterans General Hospital, Taichung, Taiwan, Department Of Physical Medicine And Rehabilitation, Tri-Service General Hospital, School Of Medicine, National Defense Medical Center, Taipei, Taiwan
Tel:+886 935605578,
Email:ccdivlaser1959@gmail.com
Abstract
Crossed Cerebellar Diaschisis (CCD) is considered a poor prognostic factor in post-stroke recovery. We postulated that the benefits of intravascular laser phototherapy in promoting brain blood circulation might also facilitate simultaneous eradication of CCD. Three courses of laser phototherapy (helium-neon laser with wavelength 632.8 nM) were applied, with each course consisting of one-hour daily phototherapy for ten consecutive days. We assessed the outcome by comparing brain images before and after the intervention. The results showed that CCD in the pre-intervention images was not evident in the post-intervention images. Post-intervention images also revealed better perfusion in the non-CCD-sided cerebellum. Unexpectedly, there appeared to be a relative decrease in uptake within the left thalamus and bilateral frontal lobes. Phototherapy was thus shown to induce prioritized redistribution of cerebral blood circulation leading to activity-dependent neurologic recovery.
Keywords
Activity-dependent; Crossed cerebellar diaschisis; Helium-neon laser; Hemorrhagic stroke; Intravascular laser irradiation of blood; Redistribution
INTRODUCTION
Stroke causes great suffering and impairment of motor, sensory, coordinative, speech, and cognitive functions. A combination of brain stimulation and neurodevelopmental therapy can improve motor function and structural connectivity [1]. Crossed Cerebellar Diaschisis (CCD) is a rare neurologic sequel that may occur after stroke. It involves decreased blood flow and decreased metabolism in the cerebellum contra lateral to a supratentorial stroke [2] and indicates a poor outcome [3]. CCD may manifest in either ischemic or hemorrhagic stroke, and can occur in any stage of stroke, though rarely in the chronic stage. Complete recovery from CCD has rare reported.
Intravascular Laser Irradiation of Blood (ILIB) is an innovative modality that has been applied in recent decades for various treatments, such as pain control [4], certain immunologic and rheumatologic disorders [5], and spinal cord injury with changes in biochemical profiles [6]. ILIB has the advantage of allowing to increase perfusion in the diaschisis areas, including basal ganglion, to enhance neurologic recovery, like cognitive function [1,7-9]. We were interested in determining where phototherapy could induce prioritized redistribution of cerebral blood circulation leading to activity-dependent neurologic recovery.
We report a case of a 52-year-old male with prior coronary artery disease suffering from chronic stroke with CCD who was treated with ILIB.
CASE PRESENTATION
The patient was a 52-year-old male with old history of coronary artery disease who suffered from left limb weakness due to hemorrhagic stroke at the right middle cerebral artery territory 4 years ago (in 2016). After craniectomy, he received regular rehabilitation including physical and occupational therapy for 2 more years. Despite therapy, he still had weakness of the left limbs and spasticity. The patient reported that wrist/shoulder extension of the affected limb occurred while yawning, especially when his left upper limbs was flaccid (Brunnstrom stage I in Aug. 2016). He visited our clinic, where neurologic examination revealed decreased muscle strength in the left limbs as 2. Evaluation of spasticity revealed a score of 2 on the Modified Ashworth Scale (MAS) in the left elbow extensor and left knee extensor, and 1 in the left elbow flexor and left knee flexor. He achieved maximum scores on the Mini-mental state examination (MMSE) and Barthel index (BI). The brain perfusion scan with Tc-99m Ethyl Cysteinate Dimer (ECD) brain perfusion study of single photon emission computed tomography (SPECT) revealed no uptake in the right frontoparietal junction, and decreased uptake in the right striatum, right thalamus, and left cerebellum (Figure 1). The finding of the left cerebellum was consistent with CCD, i.e., right vascular event with reduced perfusion in the left cerebellum. Three courses of ILIB were recommended. The protocol was performed using a Helium-Neon (He-Ne) laser device between Sep 27, 2019 and Dec 9, 2019. This protocol has been described in detail elsewhere [10].
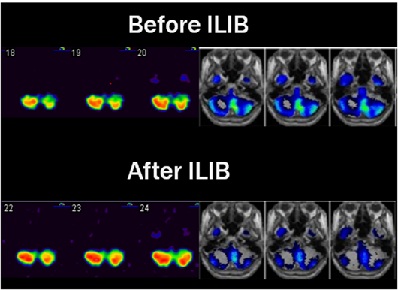 Figure 1: Regional cerebral perfusion SPECTs before and after ILIB. The white to red area indicates better perfusion than the blue and green area. As shown in left panel, before ILIB, SPECT showed hypoperfusion in the left cerebellum area compared with the right cerebellum. After ILIB, there was remarkably increased uptake in the left cerebellum, and uptake even increased on the right side simultaneously. As shown in the right panel, there was a relative decrease in perfusion in the left cerebellum of Regional Cerebral Blood Flow (rCBF). Before ILIB, a relative decrease in perfusion in rCBF in the left cerebellum (Green-blue) was noted. After ILIB treatment, left cerebellum blood flow increased (Blue).
Figure 1: Regional cerebral perfusion SPECTs before and after ILIB. The white to red area indicates better perfusion than the blue and green area. As shown in left panel, before ILIB, SPECT showed hypoperfusion in the left cerebellum area compared with the right cerebellum. After ILIB, there was remarkably increased uptake in the left cerebellum, and uptake even increased on the right side simultaneously. As shown in the right panel, there was a relative decrease in perfusion in the left cerebellum of Regional Cerebral Blood Flow (rCBF). Before ILIB, a relative decrease in perfusion in rCBF in the left cerebellum (Green-blue) was noted. After ILIB treatment, left cerebellum blood flow increased (Blue).
During the past 4 years of therapy, his muscle strength had not changed at all. However, after completing three courses of ILIB, the muscle strength of the affected side improved from 2 to 3-4.Spasticity also improved with MAS of the left elbow extensor/flexor: 1/1, left knee extensor/flexor: 1/1. He also reported better sleep quality and physical endurance. Brunnstrom stage progressed from stage I to III-IV. Wrist/shoulder extension while yawning never happened after ILIB. He achieved maximum scores on the MMSE and BI measured as before. The post-intervention SPECT image showed remarkably increased uptake in the left cerebellum (Figure 1), which had previously disclosed decreased uptake in the pre-intervention image. Unexpectedly, there was a relative decrease in uptake in the left thalamus and bilateral frontal lobe (Figure 2).
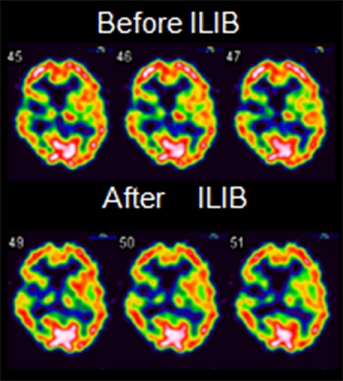 Figure 2: Regional cerebral perfusion SPECTs before and after ILIB. There is decreased uptake in the left thalamus after ILIB. Simultaneously, a relative decrease in uptake in the bilateral frontal lobe is noted.
Figure 2: Regional cerebral perfusion SPECTs before and after ILIB. There is decreased uptake in the left thalamus after ILIB. Simultaneously, a relative decrease in uptake in the bilateral frontal lobe is noted.
DISCUSSION
The occurrence of CCD indicates a poor outcome [3], which may manifest in either ischemic or hemorrhagic stroke. It can occur in any stage of stroke, though rarely in the chronic stage. CCD is rare and complete recovery has never been reported in the literature. In the treatment of the case presented herein, we wondered whether it might be possible to eradicate CCD and enhance neurological recovery. The outcome of treatment was much better than expected as, after ILIB, there was evidence of increased uptake of pre-intervention CCD and slightly increased non-CCD-sided cerebellum (Figure 1). The post-intervention SPECT showed decreased uptake in the left thalamus and bilateral frontal lobe (Figure 2). Both of these interesting findings could be attributed to prioritized redistribution.
We believe that brain circulation priority should be highly determined upon vital brain areas, like brainstem. The ultimate purpose of redistribution is to improve the crucial function of cerebellum, and simultaneously to reduce the prosperity of the abundant blood supply in the frontal lobe and thalamus, without causing any neural dysfunction of those areas. Our findings are consistent with a study conducted on sheep, which found that during hypovolemic shock, redistribution took place in the brain, i.e., decreased cortical cerebral perfusion occurred without changing the subcortical perfusion at all, indicating that crucial neural functions required for survival are better protected than higher cortical functions [11].
ILIB is an innovative treatment that has been used in recent decades for pain control, spinal cord injury, and stroke [4]. ILIB has been recognized to promote microcirculation, and many studies have shown various influences on hematologic, immunologic, and rheumatologic disorders [5]. Moreover, ILIB was found to change biochemical profiles in patients with spinal cord injury [6]. With respect to ischemic stroke, ILIB has the advantage of inducing reperfusion in the basal ganglion, which improves cognitive function [7-9]. We speculate that ILIB promoted brain circulation, resulting in eradication of CCD as well as redistribution of blood flow from the frontal lobe and thalamus to the cerebellum.
Regarding interventions for stroke, some studies showed if the patient received thrombolytic agents within the golden hour, CCD might disappear [10,12]. In our patient, however, craniectomy minimized the impact of hematoma, but it could not eradicate CCD. As shown in figure 3, for ischemic stroke, injection of thrombolytic agents results in earlier recovery of brain perfusion, and thus, CCD disappears in the chronic stage; however, for hemorrhagic stroke, the mass effect relieved by earlier operation could not prevent CCD formation. Further study is needed to determine the precise mechanism by which CCD forms after hemorrhagic stroke.
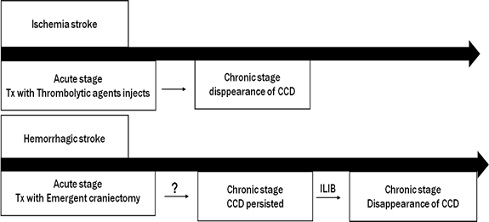 Figure 3: Comparison of CCD development between ischemic and hemorrhagic stroke in different treatment strategies. Some studies showed earlier application of thrombolytic agents could decrease the possibility of CCD formation. However, craniectomy, the most common method of treating hemorrhagic stroke, is beneficial in acute stroke. CCD is still observed in chronic stroke.
Figure 3: Comparison of CCD development between ischemic and hemorrhagic stroke in different treatment strategies. Some studies showed earlier application of thrombolytic agents could decrease the possibility of CCD formation. However, craniectomy, the most common method of treating hemorrhagic stroke, is beneficial in acute stroke. CCD is still observed in chronic stroke.
Our patient once mentioned stretching of the affected limb occurred while yawning, a phenomenon termed Parakinesia Brachialis Oscitans (PBO). This phenomenon occurred less frequently after his muscle strength improved, with simultaneous improvement shown on the post-intervention image, which might be due to the disappearance of CCD contributing to improved self-control of theaffectedlimbs.CCD and PBO have been shown to have similar neuroanatomic pathways because of the simultaneous occurrence of CCD and PBO [13].
A number of studies have investigated redistribution in brain circulation. A fetus study analyzed the relationship between fetal blood flow and birth outcomes by measuring the blood flow of the umbilical artery and cerebral artery. The authors found a higher ratio contributes to higher risk of pre-term birth after comparing two arterial index ratios, suggesting the redistribution of fetal blood flow impacts fetal development [14]. An investigation of cerebral blood flow in an extremely cold environment found that temperature change shows regional differences which contribute to the redistribution of cerebral oxygen delivery in response to thermal and hypoxic exposure [15]. With regard to thalamus perfusion in response to diabetic control, it was found that change of blood sugar level in human subjects contributes to redistribution of cerebral blood flow in the thalamus [16]. We believe that the ILIB intervention caused neurologic recovery by prioritizing redistribution of cerebral blood circulation.
In conclusion, CCD was diminished following treatment with ILIB. In addition to the improvement in CCD, uptake in both sides of the cerebellum improved in order to recover balance function, which is governed by the cerebellum, and simultaneously decreased uptake in the left thalamus and bilateral frontal lobes. We postulate that ILIB alters brain circulation, thereby facilitating the eradication of CCD or promoting redistribution. These findings highlight the importance of brain SPECT images in monitoring neurologic recovery.
ACKNOWLEDGEMENTS
The authors would like to thank the patient who participated in this report.
DISCLOSURES
The authors report no conflicts of interest. This study received no funding.
REFERENCES
- Lee JH, Kyeong S, Kang H, Kim DH (2019) Structural and functional connectivity correlates with motor impairment in chronic supratentorial stroke a multimodal magnetic resonance imaging study. Neuroreport 30: 526-531.
- Takasawa M, Watanabe M, Yamamoto S, Hoshi T, Sasaki T, et al. (2002) Prognostic value of subacute crossed cerebellar diaschisis: Single-photon emission CT study in patients with middle cerebral artery territory infarct. AJNR American Journal of Neuroradiology 23: 189-193.
- Kim Y, Lim SH, Park GY (2019) Crossed cerebellar diaschisis has an adverse effect on functional outcome in the subacute rehabilitation phase of stroke: A case-control study. Arch Phys Med Rehabil 100: 1308-1316.
- Wu PY, Penn IW, Lin PH, Wang JC, Chuang E, et al. (2018) Effects of intravenous laser irradiation of blood on pain, function and depression of fibromyalgia patients. Gen Med (Los Angeles) 6: 310.
- Dmitriev A, Iudin V, Arapov N, Martynov V (1989) Effect of intravascular laser irradiation of the blood on blood cells in pancreatitis. Klin Med (Mosk) 67: 108-110.
- Huang S-F, Tsai Y-A, Wu S-B, Wei Y-H, Tsai P-Y, Chuang T-Y (2012) Effects of intravascular laser irradiation of blood in mitochondria dysfunction and oxidative stress in adults with chronic spinal cord injury. Photomed Laser Surg 30: 579-586.
- Sung J-H, Chang S-T (2019) Reversal of impaired blood flow of the basal ganglion from the prior focal perfusion defect in a case of ischemic infarction: observation during the two stages of administration of intravenous laser irradiation of blood. J Med Stud Res 2: 011.
- Liu EY, Chang ST (2019) Benefits of intravascular laser irradiation of blood on motor and sensory recovery viewing from brain function images: Portrait of a case with chronic Sjögren’s syndrome, transverse myelitis and Guillain-Barré syndrome. Biomed J Sci & Tech Res 14: 2019.
- Chang JY, Liu CC, Liu IT, Chang ST (2019) Effects of intravascular laser irradiation of blood on cognitive function in a stroke survivor with hyperhomocysteinemia: Dual recuperations in thalamus and serum homocysteine. Biomed J Sci & Tech Res 16: 11864-11868.
- Yang WH, Lin SP, Chang ST (2017) Case report: Rapid improvement of crossed cerebellar diaschisis after intravascular laser irradiation of blood in a case of stroke. Medicine (Baltimore) 96: 5646.
- Schiffner R, Bischoff SJ, Lehmann T, Rakers F, Rupprecht S, et al. (2017) Redistribution of cerebral blood flow during severe hypovolemia and reperfusion in a sheep model: Critical role of α1-adrenergic signaling. Int J Mol Sci 18: 1031.
- Sobesky J, Thiel A, Ghaemi M, Hilker RH, Rudolf J, et al. (2005) Crossed cerebellar diaschisis in acute human stroke: A PET study of serial changes and response to supratentorial reperfusion. J Cereb Blood Flow Metab 25: 1685-1691.
- Wu YT, Chang ST, Chen LC, Li TY (2013) Concurrence of crossed cerebellar diaschisis and parakinesia brachialis oscitans in a patient with hemorrhagic stroke. Case Rep Med 2013: 519808.
- Kooijman MN, Gaillard R, Reiss IK, Hofman A, Steegers EA, et al. (2016) Influence of fetal blood flow redistribution on fetal and childhood growth and fat distribution: The Generation R Study. BJOG 123: 2104-2112.
- Chapman CL, Hess HW, Worley ML (2020) Heterogeneous redistribution of cerebral oxygen delivery to combined thermal and hypoxic exposure. The Journal of Physiology 598: 443-445.
- Hsu KC, Chang ST (2013) Correlation of thalamic blood flow redistribution with persistent complex regional pain syndrome in a stroke patient with poor diabetic control. J Diabetes Investig 4: 676-678.
Citation: Chen K-C, Lin Y-C, Tu W-C, Liu I-T, Cheng Y-Y, et al. (2020) Prioritized Redistribution of Cerebral Blood Flow for Crossed Cerebellar Diaschisis after Intravascular Laser Phototherapy in a Stroke Survivor with Prior Coronary Artery Disease. J Brain Neursci 4: 012.
Copyright: © 2020 Shin-Tsu Chang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.