
Refractive Changes Induced by Recession of the Medial Rectus and the Inferior Oblique Muscles
*Corresponding Author(s):
Leshno AriGoldschleger Eye Institute, Sheba Medical Center, Tel Hashomer, Israel
Tel:+972 35302874,
Fax:+972 35302872
Email:arileshno@gmail.com
Abstract
Purpose
To investigate refractive changes after strabismus correction by combined recession of the Medial Rectus (MR) and Inferior Oblique (IO) muscles.
Methods
We reviewed cases of combined MR and IO recession. Individuals with both preoperative refraction measurement and one month postoperative measurements were included. Double-angle mathematical methods for subtraction of refraction were used in order to calculate the surgical induced refractive change. Paired-sample Wilcoxon signed rank test and one-sample binomial tests were used to identify significant postoperative refractive changes. The prevalence of clinically significant changes was also evaluated.
Results
Fifty-five eyes from 28 subjects met the criteria and were included in the final analysis. A substantial rate (>50%) of clinically significant refractive changes resulting in a myopic shift and a positive increase in cylinder power towards with-the-rule direction were observed after combined recession of MR and IO. The rate of significant changes in terms of SE was lower. There was no correlation between the recession extent and amount of refractive change and no significant differences were observed between types of IO weakening procedure.
Conclusion
Refractive changes are a significant side effect of combined recession of MR and IO, and patients should be informed regarding the possibility of such complication prior to the procedure and close postoperative observation is warranted to prevent amblyopia.
Keywords
INTRODUCTION
Marshal, who was the first to describe in 1936 the relations between strabismus surgery and refractive change, reported a change in astigmatism in 60% of the patients [1], later reports found a weaker association between strabismus surgeries and induced refractive error, with a leading finding of a transient astigmatic change after horizontal recti muscle surgery towards with-the-rule direction [2-7]. There is no consensus among previous publications as to the clinical significance of the refractive changes [3,5-10]. Though several publications found no statistically significant change in Spherical Equivalent (SE) [2-5], there are reports of a transient myopic shift [5,11,12]. Hong et al., reported a significant change in SE towards myopia in a pediatric population operated for exotropia [7]. Although due to their study design such results might have been due to the strong accommodation in children, our group recently observed similar changes in showed that similar refractive changes occur also in adults13 and that are significantly different than those observed in the non-operated eye [14].
Most of the previous studies included single muscle surgery [2,3,5,8,12,15,16]. While there are several publications on surgeries involving both horizontal extra-ocular muscles [2,7], we did not find any series describing refractive change after combined horizontal and oblique muscles strabismus surgery.
Inferior Oblique (IO) muscle weakening procedures are used to for correction of IO overaction, which commonly develops in individuals with infantile esotropia. In many such cases, the procedure is done concomitantly with medial rectus recession. The purpose of this study is to determine the change in refractive error after strabismus surgery that involves both the MR and IO muscles by using the mathematical methods for analyzing and reporting aggregate surgically induced refractive changes as described by Holladay et al. [17]. In addition to the statistical significance of the refractive change, we evaluated the proportion of clinically significant (≥ 0.5 Diopter of change) refractive changes as well.
MATERIALS AND METHODS
Subjects
Cycloplegic refraction was performed 30 minutes after instillation of 1% cyclopentolate and, 2 minutes apart [18]. All refractions were performed by one of the authors (XX) by using a hand held retinoscopy in a darkened room.
One of the authors (XX) performed all of the surgeries between August 1988 and September 2014, which included fornix conjunctival incisions and recession of the MR muscle combined with either recession or myectomy of the IO muscle.
For each patient the following data was reviewed: age of patient at time of surgery, sex, motor alignment before and after the surgery at near and distance fixation, type of surgery performed, extent of recession of each muscle and refraction before and after the surgery.
The study was approved by the institutional review board of XXXXXXXXXXX and was fully compliant with the principles of the Declaration of Helsinki.
Statistical Analysis
Lastly we evaluated the clinical significance of the changes. A change in refractive power of 0.5D or more was considered clinically significant. One-sample binomial test was used to evaluate whether the proportion of clinically significant changes was greater than an acceptable 10%. All statistical analyses were performed using IBM SPSS statistics 22 program (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). A P-value less than 0.05 were considered statistically significant.
RESULTS
A total of 55 eyes from 28 subjects, met the above criteria and were included in the final analysis, of which 31 in the IOR group and 24 in the IOM group. The mean age of the 13 males and 15 females was 3.28 ± 2.11 and 5.93 ± 5.85 years respectively. Table 1 summarizes the baseline characteristics of the study group. No significant differences between the two surgical groups were found in terms of age or preoperative spherocylinder.
|
Procedure type |
|
Eye no. (subjects) |
Age (years) |
Extent of MR recess (mm) |
Extent of IO recess |
Preoperative Refractive measurements |
|||
|
(mm) |
Sphere |
Cylinder |
Axis |
SE |
|||||
|
MR recession |
Mean |
31 |
5.61 |
4.69 |
13.16 |
1.49 |
0.94 |
85.48 |
1.96 |
|
+ |
SD |
-16 |
5.73 |
1.17 |
1.97 |
3.66 |
0.87 |
60.82 |
3.68 |
|
IO recession |
Range |
1-22 |
3.0-6.5 |
8.0-15.0 |
-11.5-5.5 |
0.0-3.5 |
0-180 |
-11.3-5.5 |
|
|
MR recession |
Mean |
24 |
3.58 |
5.01 |
- |
1.7 |
0.92 |
73.54 |
2.16 |
|
+ |
SD |
-12 |
2.62 |
1.25 |
- |
1.57 |
0.82 |
48.47 |
1.58 |
|
IO myectomy |
Range |
1-9 |
3.0-7.0 |
- |
-1.8-5.0 |
0.0-3.3 |
0-180 |
-0.8-5.6 |
|
|
Total |
Mean |
55 |
4.73 |
4.86 |
13.16 |
1.58 |
0.93 |
80.27 |
2.05 |
|
SD |
-28 |
4.71 |
1.21 |
1.97 |
2.92 |
0.84 |
55.6 |
2.93 |
|
|
Range |
|
1-22 |
3.0-7.0 |
8.0-15.0 |
-11.5-5.5 |
0.0-3.5 |
0-180 |
-11.3-5.6 |
|
A summary of preoperative and 1 month postoperative cycloplegic refraction is depicted in table 2. All power parameters (e.g. sphere, cylinder and SE) changed significantly between two measurements (P < 0.05). Statistical significance maintained after stratification according to IO weakening procedure.
|
Procedure type |
Parameter (diopter) |
Preoperative |
1M Postoperative |
P valuea |
|
MR recession + IO recession (N=31) |
Sphere |
1.49 ± 3.66 |
1.25 ± 3.61 |
0.011 |
|
Cylinder |
0.94 ± 0.87 |
1.36 ± 1.18 |
0.007 |
|
|
SE |
1.96 ± 3.68 |
1.93 ± 3.67 |
0.465 |
|
|
MR recession + IO myectomy (N=24) |
Sphere |
1.70 ± 1.57 |
1.25 ± 2.02 |
0.001 |
|
Cylinder |
0.92 ± 0.82 |
1.33 ± 0.84 |
0.001 |
|
|
SE |
2.16 ± 1.58 |
1.92 ± 1.97 |
0.020 |
|
|
Total (N=55) |
Sphere |
1.58 ± 2.92 |
1.25 ± 3.00 |
<0.0001 |
|
Cylinder |
0.93 ± 0.84 |
1.35 ± 1.03 |
<0.0001 |
|
|
SE |
2.05 ± 2.93 |
1.92 ± 3.03 |
0.024 |
Since the outcome of astigmatic correction depends on the axis as well as the magnitude of the toric change, vector analysis was used to examine these changes. After calculating the SIRC for each eye, the method described by Holladay and colleagues [17] for evaluating and reporting astigmatism for aggregate data was applied. Table 3 summarizes the SIRC according to surgical approach. Overall the magnitude of surgically induced cylinder was found to be significantly different from zero (+0.53 ± 0.67, p < 0.0001) as well as the induced SE (-0.13 ± 0.40, p = 0.028) (Table 3). Statistical significance was maintained in both surgical approaches with the exception for the surgically induced SE which was non-significant in the IO recession group. Figure 1 illustrates the surgically induced cylinder power using a double-angle plot.
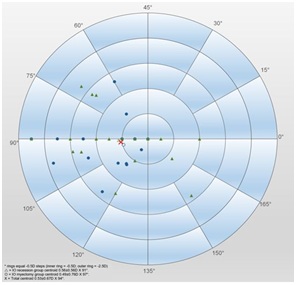 Figure 1: Double angle polar plot of astigmatism data using the value of the cylinder for the magnitude and the axis of the astigmatism for the angle.
Figure 1: Double angle polar plot of astigmatism data using the value of the cylinder for the magnitude and the axis of the astigmatism for the angle.
|
Parameter (Diopter power), Mean ± SD |
Sphere |
Cylinderb |
Axis (deg.) b |
SE |
P valuec |
P valued |
|
IO weakening procedure |
||||||
|
Recession (N = 31) |
-0.45± 0.39 |
0.56 ± 0.56 |
91 |
-0.04 ± 0.26 |
<0.0001 |
0.403 |
|
Myectomy (N = 24) |
-0.75 ± 0.83 |
0.49 ± 0.76 |
97 |
-0.24 ± 0.51 |
0.0044 |
0.034 |
|
Total (N = 55) |
-0.61 ± 0.53 |
0.53 ± 0.67 |
94 |
-0.13 ± 0.40 |
<0.0001 |
0.028 |
cSurgically induced cylinder different from zero.
dSurgically induced SE different from zero.
In a subset of 10 cases a third cycloplegic refraction measurement was available from a subsequent follow-up visit (mean 323 ± 121 days after the surgery), which did not differ significantly from the 1-month postoperative measurement.
We observed a substantial proportion of cases with clinically significant refractive changes after surgery. Figure 2 depicts the proportion of cases where the refractive change was of clinical significance in each parameter. Using one sample binomial test we found all proportions to be significantly different from an acceptable 10% rate for changes equal or greater than 0.5D as well as for changes equal or greater than 0.75D (P < 0.0001). Statistical significance was maintained in all sub-groups after stratification according to surgical technique.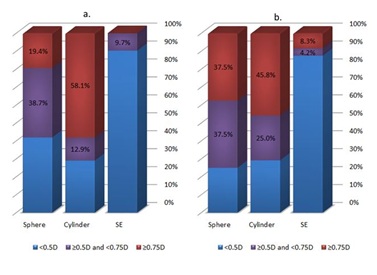 Figure 2: Proportion of cases with clinically significant surgically induced changes in refraction in the IO recession (a) and the IO myectomy (b) groups
Figure 2: Proportion of cases with clinically significant surgically induced changes in refraction in the IO recession (a) and the IO myectomy (b) groups
No significant association was found between the extent of MR or IO recession and the changes in refractive measurements.
DISCUSSION
As our main research question regards the clinical significance of the refractive change, we present in figure 1 the surgically induced astigmatism data using the value of the cylinder for the magnitude and the axis of the astigmatism for the angle. For each point on the plot; the larger the distance from the center of the plot, the larger is the cylindrical power induced by the surgery, although most of the points are within a 1D of astigmatism, over a third of patients had an astigmatic change >1D and in three cases the astigmatic change is >2D.
We also presented separately in figure 2 the proportion of cases in which refractive change was clinically significant. In 10.9% of eyes the SE change was ≥ 0.5D, the change in the cylinder power alone and the sphere power alone were ≥ 0.5 in 70.9% and 65.5% of the eyes respectively.
A major disagreement among previous publications, regards the duration and therefore clinical significance of the refractive changes. While some investigators concluded that the refractive error change was transient [5,8], others reported a long lasting clinically significant refractive change [3,6,7,9,10]. In some studies the absolute refractive change was not found significant but there was a clinically significant change in a subset of patients; Nardi et al., concluded that the change in refractive error after horizontal muscle surgery is transient and insignificant, although they found residual astigmatism of >1D and of >0.5D at 30 days post-op among 6% and 12% of their patients, respectively [8]. Rajavi et al., also concluded the refractive change to be non-significant although 16% of their patients had astigmatic power change equal or more than 1D 3 months after the surgery [5]. Schworm et al., reported a lasting induced astigmatism of more than 3D in 4% of their patients 3 months after the surgery [16]. Unfortunately, we do not have a longer than one month follow up for all our cases, as many do not return for further examination after the strabismus has resolved and some object further Cycloplegic examinations, in a subgroup of 10 eyes (18.1%) a third cycloplegic refraction performed at least 161 days postoperatively, found the operative induced change to be stable.
According to the results of this study, refractive error after strabismus surgery of combined IO and MR rectus recession changes significantly. Although the mean change is not clinically significant, there was a clinical significant change in over 50% of the patients, similar to previous reports [ADD REFF], which might interfere with binocular vision, amblyopia treatment or even cause amblyopia in very young subjects.
Several mechanisms were offered to explain the change in refraction. The main theory regarding the change in the spheric power and cylinder power and axis relates to corneal changes [1,3,11,23-25]. However the operation conducted in most of these studies involved horizontal muscles alone. Kushner et al., demonstrated that oblique muscle surgery produce a long term cyclotortion which leads to a suitable change in the cylinder axis of approximately 10 degrees [15]. The induced cylinder axis in the current study was similar to that reported in previous studies on MR recession alone, meaning that the additional IO recession did not seem to have a major effect. A possible explanation is that the weakening procedure used by Kusnher et al., consisted of a recession to a point 3mm posterior and 2mm temporal to the temporal end of the inferior rectus insertion rather that 14mm recession or myectomy as was done in the present study. It should be noted that no significant differences were observed between the two IO weakening techniques that were reviewed in the present study in terms of refractive changes.
The results of this study should be interpreted within the context of its limitations. This is a retrospective review and it is subject to the selection and follow-up bias inherent to all retrospective reviews. In addition, there is a variation in age at time of surgery which has not only implications in terms of risk of amblyopia development, but might also prove to be a risk factor for postoperative refractive changes.
In summary we agree with previous reports [3,6,7,9], in which the refractive change was found to be clinically significant. Therefore, we strongly support informing all patients prior to strabismus surgery about a reasonable risk of refractive change and as we believe all patients should be re- refracted one-month post operatively and afterwards again as needed.
REFERENCES
- Marshall D (1936) Changes in refraction following operation for strabismus. Arch Ophthalmol 15: 1020-1031.
- Bagheri A, Farahi A, Guyton DL (2003) Astigmatism induced by simultaneous recession of both horizontal rectus muscles. J AAPOS 7: 42-46.
- Preslan MW, Cioffi G, Min YI (1992) Refractive error changes following strabismus surgery. J Pediatr Ophthalmol Strabismus 29: 300-304.
- Denis D, Bardot J, Volot F, Saracco JB, Maumenee IH (1995) Effects of strabismus surgery on refraction in children. Ophthalmologica 209: 136-140.
- Rajavi Z, Mohammad Rabei H, Ramezani A, Heidari A, Daneshvar F (2008) Refractive effect of the horizontal rectus muscle recession. Int Ophthalmol 28: 83-88.
- Chun BY, Kim HK, Kwon JY (2010) Comparison of magnitude of astigmatism induced by lateral rectus recession. Optom Vis Sci 87: 61-65.
- Hong SW, Kang NY (2012) Astigmatic changes after horizontal rectus muscle surgery in intermittent exotropia. Korean J Ophthalmol 26: 438-445.
- Nardi M, Rizzo S, Pellegrini G, Lepri A (1997) Effects of strabismus surgery on corneal topography. J Pediatr Ophthalmol Strabismus 34: 244-246.
- Killer HE, Bähler A (1999) Significant immediate and long-term reduction of astigmatism after lateral rectus recession in divergent Duane’s syndrome. Ophthalmologica 213: 209-210.
- Fix A, Baker JD (1985) Refractive changes following strabismus surgery. Am Orthopt J 35: 59-62.
- Snir M, Nissenkorn I, Buckman G, Cohen S, Ben-Sira I (1989) Postoperative refractive changes in children with congenital esotropia: a preliminary study. Ophthalmic Surg 20: 57-62.
- Kutlutürk I, Eren Z, Koytak A, Sari ES, Alis A, et al. (2014) Surgically Induced Astigmatism Following Medial Rectus Recession: Short-Term and Long-Term Outcomes. J Pediatr Ophthalmol Strabismus 51: 171-176.
- Mezad-Koursh D, Leshno A, Ziv-Baran T, Stolovitch C (2017) Refractive Changes Induced by Strabismus Corrective Surgery in Adults. J Ophthalmol 2017: 1-8.
- Leshno A, Mezad-Koursh D, Ziv-Baran T, Stolovitch C (2017) A paired comparison study on refractive changes after strabismus surgery. J AAPOS 21: 460-462.
- Kushner BJ (1986) The effect of oblique muscle surgery on the axis of astigmatism. J Pediatr Ophthalmol Strabismus 23: 277-280.
- Schworm HD, Ullrich S, Höing C, Dittus C, Boergen KP (1997) Original papers: Does strabismus surgery induce significant changes of corneal topography? Strabismus 5: 81-89.
- Holladay JT, Moran JR, Kezirian GM (2001) Analysis of aggregate surgically induced refractive change, prediction error, and intraocular astigmatism. J Cataract Refract Surg 27: 61-79.
- Stolovitch C, Alster Y, Goldstein M, Loewenstein A, Lazar M (1998) Application of cyclopentolate 1% to the medial canthus in children. J Pediatr Ophthalmol Strabismus 35: 182-184.
- Naylor EJ (1968) Astigmatic difference in refractive errors. Br J Ophthalmol 52: 422-425.
- Holladay JT, Cravy TV, Koch DD (1992) Calculating the surgically induced refractive change following ocular surgery. J Cataract Refract Surg 18: 429-443.
- Retzlaff J, Paden PY, Ferrell L (1993) Vector analysis of astigmatism. Adding and subtracting spherocylinders. J Cataract Refract Surg 19: 393-398.
- Holladay JT, Dudeja DR, Koch DD (1998) Evaluating and reporting astigmatism for individual and aggregate data. J Cataract Refract Surg 24: 57-65.
- Kwitko S, Feldon S, McDonnell PJ (1992) Corneal topographic changes following strabismus surgery in Grave's disease. Cornea 11: 36-40.
- Thompson WE, Reinecke RD (1980) The changes in refractive status following routine strabismus surgery. J Pediatr Ophthalmol Strabismus 17: 372-374.
- Hainsworth DP, Bierly JR, Schmeisser ET, Baker RS (1999) Corneal topographic changes after extraocular muscle surgery. J AAPOS 3: 80-86.
Citation: Daphna M-Z, Tomer Z-B, Ofira Z, Sharon BM, Chaim S, et al. (2019) Refractive Changes Induced by Recession of the Medial Rectus and the Inferior Oblique Muscles. J Ophthalmic Clin Res 6: 053.
Copyright: © 2019 Mezad-Koursh Daphna, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

