
Journal of Ophthalmology & Clinical Research Category: Clinical
Type: Research Article
Tisseel Fibrin Glue vs Sutures for Conjunctival Closure in Glaucoma Drainage Implant Surgery
*Corresponding Author(s):
Nicholas LancasterNational Capital Consortium, Rockville Pike, Bethesda, United States
Tel:+1 2533477386 (C), +1 3012951339 (W),
Fax:+1 3012951481
Email:Nicholas.d.lancaster.mil@mail.mil
Received Date: Jun 14, 2016
Accepted Date: Aug 02, 2016
Published Date: Aug 17, 2016
Abstract
Objective
To evaluate the safety and efficacy of Tisseel Fibrin Glue for closure of conjunctiva in the setting of Glaucoma Drainage Implant (GDI) surgery compared to standard suture closure of the conjunctiva.
Methods
Retrospective non-randomized case-control study reviewing 35 consecutive cases of GDI implantation using traditional suture closure of conjunctiva by one surgeon compared with 22 consecutive cases of GDI implantation using Tisseel fibrin glue (Baxter, AG, Vienna, Austria) closure of conjunctiva by a second surgeon. Six-month follow-up data for each group, including Intraocular Pressure (IOP) measurements and need for IOP lowering medications as well as operative times and complication rates were evaluated.
Results
There was no significant difference between the Tisseel group and the suture group in IOP levels prior to GDI surgery, nor was there a significant difference by the 6 month post-operative visit. The mean number of pre-op glaucoma drops was significantly less in the Tisseel group, 2.7 drops, than in the suture group, 3.0 drops (p=0.01). The number of post-op glaucoma drops used in the Tisseel group was significantly less than that used in the suture group for all time periods. The mean (SD) number of IOP lowering drops used on POW#1 was 1.3 (1.3) in the Tisseel group, for a mean decrease from preop of 1.4 drops, and 2.3 (1.0) in the suture group, for a mean decrease from preop of 0.7 drops. On POM#1 the mean (SD) number of IOP lowering drops used was 1.7 (1.4) in the Tisseel group, for a mean decrease from preop of 1.0 drops, and 2.7 (0.6) in the suture group, for a mean decrease from preop of 0.3 drops. On POM#3 the mean (SD) number of IOP lowering drops used was 1.2 (1.0) in the Tisseel group, for a mean decrease from preop of 1.5 drops, and 2.0 (1.1) in the suture group, for a mean decrease from preop of 1.0 drops. On POM#6 the mean (SD) number of IOP lowering drops used was 1.2 (0.8) in the Tisseel group, for a mean decrease from preop of 1.5 drops, and 1.9 (1.0) in the suture group, for a mean decrease from preop of 1.1 drops. The mean decrease in number of glaucoma drops used from pre-op to post-op was greater in the Tisseel group compared to the suture group and was statistically significant at all-time points. The mean surgical time (SD) was significantly less for the Tisseel group, 74.5 (23.2) min, than for the suture group, 113.6 (27.6) min (p<0.001). Complication rates were similar between the two groups, with iritis, CME, and choroidal effusions being most common. In the suture group there were 2 cases of conjunctival erosion, and in the fibrin glue group there was one case of conjunctival retraction and one case of post-operative bleb related endophthalmitis.
Conclusion
The results of our study support the conclusion that the use of fibrin glue for conjunctival closure in GDI surgery is associated with faster surgical times and possibly to decreased use of IOP lowering drops in the post-operative period, while having no impact on IOP, when compared to traditional sutures closure of conjunctiva. A larger, randomized study, with increased control of surgical technique is needed to further investigate these relationships.
To evaluate the safety and efficacy of Tisseel Fibrin Glue for closure of conjunctiva in the setting of Glaucoma Drainage Implant (GDI) surgery compared to standard suture closure of the conjunctiva.
Methods
Retrospective non-randomized case-control study reviewing 35 consecutive cases of GDI implantation using traditional suture closure of conjunctiva by one surgeon compared with 22 consecutive cases of GDI implantation using Tisseel fibrin glue (Baxter, AG, Vienna, Austria) closure of conjunctiva by a second surgeon. Six-month follow-up data for each group, including Intraocular Pressure (IOP) measurements and need for IOP lowering medications as well as operative times and complication rates were evaluated.
Results
There was no significant difference between the Tisseel group and the suture group in IOP levels prior to GDI surgery, nor was there a significant difference by the 6 month post-operative visit. The mean number of pre-op glaucoma drops was significantly less in the Tisseel group, 2.7 drops, than in the suture group, 3.0 drops (p=0.01). The number of post-op glaucoma drops used in the Tisseel group was significantly less than that used in the suture group for all time periods. The mean (SD) number of IOP lowering drops used on POW#1 was 1.3 (1.3) in the Tisseel group, for a mean decrease from preop of 1.4 drops, and 2.3 (1.0) in the suture group, for a mean decrease from preop of 0.7 drops. On POM#1 the mean (SD) number of IOP lowering drops used was 1.7 (1.4) in the Tisseel group, for a mean decrease from preop of 1.0 drops, and 2.7 (0.6) in the suture group, for a mean decrease from preop of 0.3 drops. On POM#3 the mean (SD) number of IOP lowering drops used was 1.2 (1.0) in the Tisseel group, for a mean decrease from preop of 1.5 drops, and 2.0 (1.1) in the suture group, for a mean decrease from preop of 1.0 drops. On POM#6 the mean (SD) number of IOP lowering drops used was 1.2 (0.8) in the Tisseel group, for a mean decrease from preop of 1.5 drops, and 1.9 (1.0) in the suture group, for a mean decrease from preop of 1.1 drops. The mean decrease in number of glaucoma drops used from pre-op to post-op was greater in the Tisseel group compared to the suture group and was statistically significant at all-time points. The mean surgical time (SD) was significantly less for the Tisseel group, 74.5 (23.2) min, than for the suture group, 113.6 (27.6) min (p<0.001). Complication rates were similar between the two groups, with iritis, CME, and choroidal effusions being most common. In the suture group there were 2 cases of conjunctival erosion, and in the fibrin glue group there was one case of conjunctival retraction and one case of post-operative bleb related endophthalmitis.
Conclusion
The results of our study support the conclusion that the use of fibrin glue for conjunctival closure in GDI surgery is associated with faster surgical times and possibly to decreased use of IOP lowering drops in the post-operative period, while having no impact on IOP, when compared to traditional sutures closure of conjunctiva. A larger, randomized study, with increased control of surgical technique is needed to further investigate these relationships.
INTRODUCTION
Glaucoma Drainage Implant (GDI) surgery is increasingly being utilized in cases of refractory glaucoma [1]. In GDI surgery, a peritomy is created in the beginning of the surgery and one of the last steps is to return the conjunctiva to its original position and secure it in place. Traditionally conjunctival closure has been accomplished by suturing the conjunctiva to the sclera with absorbable sutures, which can be one of the most time consuming steps of the surgery. Recently, Kahook and Noecker [2] described using fibrin glue in place of sutures to secure the conjunctiva after GDI surgery, and found it to decrease surgery time and decrease conjunctival inflammation, while having no effect on post-operative intraocular pressure. However, the above study had a small number of patients (28 total) and only followed patients for 3 months.
We investigated the use of fibrin glue as a substitute for sutures in conjunctival closure after GDI surgery and followed patients for 6 months. Operating time, Intraocular Pressure (IOP), number of IOP lowering drops, and complication rates were compared between a group of patients with traditional suture closure of conjunctiva and a group of patients with Tisseel fibrin glue conjunctival closure following GDI surgery.
We investigated the use of fibrin glue as a substitute for sutures in conjunctival closure after GDI surgery and followed patients for 6 months. Operating time, Intraocular Pressure (IOP), number of IOP lowering drops, and complication rates were compared between a group of patients with traditional suture closure of conjunctiva and a group of patients with Tisseel fibrin glue conjunctival closure following GDI surgery.
METHODS
This was a 2 surgeon, retrospective, non-randomized case-control study involving 22 consecutive patients who underwent GDI surgery and had their conjunctiva closed with fibrin glue compared with 35 consecutive patients who underwent GDI surgery closed with sutures from October 1st 2011 to April 30th2014. All patients received a Baervelt 350 mm2 (Advanced Medical Optics, Santa Anna, California, USA) implant. All patients in the fibrin glue group received Tisseel Fibrin Glue (BaxterAG, Vienna, Austria). All patients in the fibrin glue group were operated on by the same surgeon, and all patients in the sutures group were operated on by the same second surgeon.
In the fibrin glue group the fibrin glue was used only to close the conjunctiva. In both groups a half-moon corneal patch graft was used to cover the tube and was secured in place by vicryl sutures passed partial thickness through the sclera.
Patients included in the study could have any form of glaucoma. Patients were excluded who underwent combined procedures (such as GDI combined with cataract surgery.) Number of pre-operative glaucoma drops was established by reviewing the patient’s pre-operative encounter. Pre-operative IOP was established by reviewing the 3 encounters prior to surgery and averaging the IOP of these 3 encounters. IOP’s were measured using Goldman applanation tonometry. Post-operative visits occurred one day after surgery (POD1), one-week after surgery (POW1), one-month after surgery (POM1), three-months after surgery (POM3), and six-months after surgery (POM6). At each visit the number of glaucoma drops and IOP were recorded, as well as any post-operative complications. The post-operative visit that occurred closest to the POW1, POM1, etc., visit was recorded as the POW1, POM1, etc. visit. If there was no visit that was closest to POW1, POM1, or POM3 then “no visit” was entered. If there was no visit within 1.5 months of POM6 visit “no visit” was entered. If the patient had a visit prior to and after POW1 (or POM1, etc.) that were equidistant, the average of the 2 IOPs was used. For all IOP measurements, if 2 measurements were recorded by the technician they were averaged. If the IOP was rechecked by the physician, the physician’s IOP recheck was used.
Means are reported with Standard Deviations (± SD). Surgical time was compared between groups using a two-sample t-test. Age was compared across groups with an exact Wilcoxon test. Sex was compared across groups using Fisher’s exact test.
To analyze eye drops prescribed over time, we used a poisson log linear Generalized Estimating Equation (GEE) with time of measurement as a within subject variable and closure type as a between subjects variable. To analyze IOPs over time, we utilized a linear GEE with time of measurement as a within subject variable and closure type as a between subjects variable. Significant effects were evaluated using Wald’s chi square test and pairwise least-square mean contrasts. Data were analyzed using IBM/SPSS Statistics (version 21, IBM/SPSS, Chicago IL) and R (R Foundation, Vienna, Austria).
In the fibrin glue group the fibrin glue was used only to close the conjunctiva. In both groups a half-moon corneal patch graft was used to cover the tube and was secured in place by vicryl sutures passed partial thickness through the sclera.
Patients included in the study could have any form of glaucoma. Patients were excluded who underwent combined procedures (such as GDI combined with cataract surgery.) Number of pre-operative glaucoma drops was established by reviewing the patient’s pre-operative encounter. Pre-operative IOP was established by reviewing the 3 encounters prior to surgery and averaging the IOP of these 3 encounters. IOP’s were measured using Goldman applanation tonometry. Post-operative visits occurred one day after surgery (POD1), one-week after surgery (POW1), one-month after surgery (POM1), three-months after surgery (POM3), and six-months after surgery (POM6). At each visit the number of glaucoma drops and IOP were recorded, as well as any post-operative complications. The post-operative visit that occurred closest to the POW1, POM1, etc., visit was recorded as the POW1, POM1, etc. visit. If there was no visit that was closest to POW1, POM1, or POM3 then “no visit” was entered. If there was no visit within 1.5 months of POM6 visit “no visit” was entered. If the patient had a visit prior to and after POW1 (or POM1, etc.) that were equidistant, the average of the 2 IOPs was used. For all IOP measurements, if 2 measurements were recorded by the technician they were averaged. If the IOP was rechecked by the physician, the physician’s IOP recheck was used.
Means are reported with Standard Deviations (± SD). Surgical time was compared between groups using a two-sample t-test. Age was compared across groups with an exact Wilcoxon test. Sex was compared across groups using Fisher’s exact test.
To analyze eye drops prescribed over time, we used a poisson log linear Generalized Estimating Equation (GEE) with time of measurement as a within subject variable and closure type as a between subjects variable. To analyze IOPs over time, we utilized a linear GEE with time of measurement as a within subject variable and closure type as a between subjects variable. Significant effects were evaluated using Wald’s chi square test and pairwise least-square mean contrasts. Data were analyzed using IBM/SPSS Statistics (version 21, IBM/SPSS, Chicago IL) and R (R Foundation, Vienna, Austria).
RESULTS
The median age of the fibrin glue closure group (81 y, range: 9-90) was significantly higher than the age of the suture closure group (74 y, range: 28-86), p = 0.04. The sex distribution in the fibrin glue (12M/9F) and suture (17M/18F) groups was well balanced. The number of preoperative IOP lowering medications ranged from 1 to 4, while the number of POW#1 IOP lowering medications ranged from 0 to 4, the number of POM#1IOP lowering medications ranged from 0 to 3, the number of POM#3IOP lowering medications ranged from 0 to 4, and the number of POM#6IOP lowering medications ranged from 0 to 3. The preoperative IOPs ranged from 9.67 to 37.3 mmHg, while the POD#1 IOPs ranged from 1 to 44 mmHg, the POW#1 IOPs ranged from 2 to 36 mmHg, the POM#1 IOPs ranged from 4 to 40 mmHg, the POM#3 IOPs ranged from 5 to 31 mmHg, and the POM#6 IOPs ranged from 4 to 29 mmHg.
As depicted in figure 1, cases closed with sutures took an average of 113.6 (± 27.6) min to complete, whereas cases closed with fibrin glue took an average of 74.5 (± 23.2) min to complete, a mean difference of 39.1 min. This difference in time to complete surgery across the two closure types was statistically significant, p < 0.001.
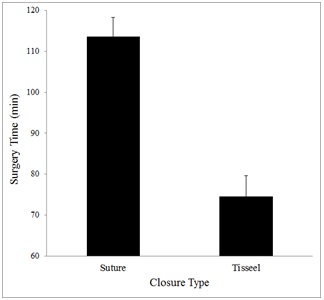
Figure 1: Depicts the mean surgery time (in minutes) to finish surgery with each type of closure. Error bars are Standard Error of the Mean (SEM).
Figure 2, shows the number of prescribed medications over time for each closure type, which shows two general trends: subjects were prescribed fewer eye drops after the surgery was completed, and subjects whose surgeries were closed with fibrin glue were prescribed fewer eye drops than those closed by sutures. Statistical analysis of these data confirmed a significant main effect of closure type, p = 0.01, and a main effect of measurement time, p < 0.001. There was also a significant interaction of closure type and time, p < 0.001, confirming that there was a larger difference in drops prescribed after each closure than existed preoperatively. Figure 3, shows the intraocular pressure over time for each closure type. While there was a significant decrease in intraocular pressure over time in both groups (p < 0.001), there was no significant difference between closure types.
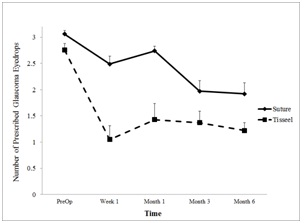
Figure 2: Depicts the mean number of prescribed drops at times pre- and post-operatively after surgery with each type of closure. Error bars are SEM.
As depicted in figure 1, cases closed with sutures took an average of 113.6 (± 27.6) min to complete, whereas cases closed with fibrin glue took an average of 74.5 (± 23.2) min to complete, a mean difference of 39.1 min. This difference in time to complete surgery across the two closure types was statistically significant, p < 0.001.
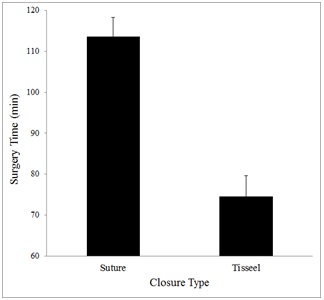
Figure 1: Depicts the mean surgery time (in minutes) to finish surgery with each type of closure. Error bars are Standard Error of the Mean (SEM).
Figure 2, shows the number of prescribed medications over time for each closure type, which shows two general trends: subjects were prescribed fewer eye drops after the surgery was completed, and subjects whose surgeries were closed with fibrin glue were prescribed fewer eye drops than those closed by sutures. Statistical analysis of these data confirmed a significant main effect of closure type, p = 0.01, and a main effect of measurement time, p < 0.001. There was also a significant interaction of closure type and time, p < 0.001, confirming that there was a larger difference in drops prescribed after each closure than existed preoperatively. Figure 3, shows the intraocular pressure over time for each closure type. While there was a significant decrease in intraocular pressure over time in both groups (p < 0.001), there was no significant difference between closure types.
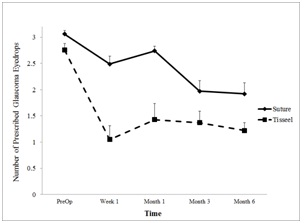
Figure 2: Depicts the mean number of prescribed drops at times pre- and post-operatively after surgery with each type of closure. Error bars are SEM.
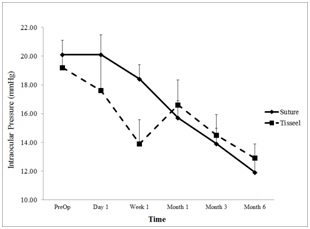
Figure 3: Depicts the mean intraocular pressure at times pre- and post-operatively after surgery with each type of closure. Error bars are SEM.
Complication rates were similar between the 2 groups. In the suture group, 14/35 (40%) patients had some post-operative complication, with iritis (3 cases), CME (6 cases) and choroidal effusions (4 cases) being the most common. In the suture group there were 2 cases of conjunctival erosion, one of which required suturing of the conjunctiva, the other of which required explanting the Baervelt 350 mm2 GDI. In the fibrin glue group, 9/22 (41%) patients had some post-operative complication, with iritis (3 cases), CME (3 cases) and choroidal effusions (4 cases) being the most common. In the fibrin glue group there was one case of conjunctival retraction over the patch graft, and one case of post-operative bleb related endophthalmitis occurring on POM#2, resulting in apars-plana vitrectomy and intravitreal injections of ceftazidime and vancomycin. Subsequently this eye developed a wound leak from a sclerostomy and underwent a bleb revision with IOL explant and endocyclophotocoagulation.
DISCUSSION
Sutures have been used in ophthalmic surgery for generations, and are still the preferred method for tissue closure in most situations. However, sutures may induce inflammation, and suturing can be very time consuming, thus many ophthalmic surgeons have begun using glues in place of sutures in certain situations.
Glues as an aid to ophthalmic surgery have come into widespread use, with fibrin glue finding the most diverse uses. Cyanoacrylate glues are used in corneal disease due to their high tensile strength, often to plug small globe perforations or to bolster thin areas that are in danger of perforating. However their propensity for inducing inflammation, persistence as a foreign body, and impermeability to fluids and metabolites make them unsuitable for intraocular use or for use under the conjunctiva. Fibrin glue, on the other hand, does not induce an inflammatory reaction, is easily and completely broken down by the body, and is permeable to fluids and metabolites, making it suitable for sub-conjunctival use, and even intraocular use [3].
In corneal surgery the use of fibrin glue has found many uses. Its use has been described in anterior lamellar keratoplasty to glue the graft onto the host bed in what is referred to as Sutureless Anterior Lamellar Keratoplasty (SALK) [4]. Its use in pterygium surgery, to glue an amniotic membrane graft or conjunctival autograft to the scleral bed, is now common practice in many surgical centers.
In 2013 an ophthalmic technology assessment evaluated the use of fibrin glue vs sutures for closure of conjunctival incisions in strabismus surgery. While no level 1 studies were found, 5 level 2 studies were identified and analyzed, the results of which led to the conclusion that the use of fibrin glue to close limbal conjunctival incisions in strabismus surgery resulted in less postoperative inflammation and required shorter operating time compared to sutures, but it increased the percentage of wounds requiring subsequent repair with sutures [5].
In glaucoma surgery fibrin glue has been studied extensively. Choudari et al., have described its use in securing a corneal patch graft over the tube in Ahmed glaucoma valve surgery [6]. Freeman et al., compared fibrin glue to sutures in pediatric GDI surgeries for securing the tube to the sclera, the pericardial patch graft over the tube, and closing the conjunctiva and found no differences in complication rates or post-operative IOPs [7]. Martinez-de-la-Casa et al., compared the use of fibrin glue vs 10-O nylon sutures for conjunctival closure in trabeculectomy surgeries and found that each modality was equal in terms if IOP lowering and the use of fibrin glue shortened surgery times and was associated with decreased patient discomfort, though, there were a higher incidence of wound dehiscence in the fibrin glue group [8].
In 2006 Kahook and Noecker reported on the use of fibrin glue vs. sutures in GDI surgery, finding that fibrin glue was associated with less postoperative inflammation and shorter surgery times, while having no effect on postoperative IOP.
Our study supports the association with use of fibrin glue for conjunctival closure and faster surgery times. Faster surgical times are important as operating room time is expensive, thus shorter surgical times save money. A limitation of our study includes the use of two surgeons, one for each arm of the study, which could affect surgery time as one surgeon may naturally be a faster surgeon. However, the result of shorter surgery time was also found in Kahook and Noecker’s study [2] in which the same surgeon was used in both arms.
The statistically significant difference in number of IOP lowering eye drops used between the two groups was an unexpected result. Patients in the suture closure group were using more IOP lowering drops before surgery than those in the fibrin glue group and the difference in number of IOP lowering drops increased after the surgery. Both the initial difference in number of IOP lowering drops and the increase in the difference between the 2 groups were statistically significant. IOP differences between the groups were not statistically significant at PreOp or during the post-operative period, except at POW1. The difference in number of IOP lowering drops at PreOp may be a difference in practice patterns between the 2 glaucoma surgeons, with the surgeon for the suture group being more aggressive in prescribing IOP lowering drops before going to surgery. However, the statistically significant increase in the difference in number of IOP lowering drops from PreOp to PostOp suggests an increase in effectiveness of GDI surgery when fibrin glue is used vs. sutures for closure of conjunctiva.With more IOP lowering drops being used by the suture group postoperatively, if suture assisted GDI surgery and fibrin glue assisted GDI surgery are equivalent in terms of IOP lowering, one would expect the suture group to have lower IOPs than the fibrin glue group, which was not demonstrated in our results. Our results suggest that the use of fibrin glue to close conjunctiva in GDI surgery may be associated with a lower number of IOP lowering drops postoperatively. This could be explained by the decrease in inflammation associated with the use of fibrin glue, as reported by Kahook and Noecker [2], causing less fibrosis and encapsulation of the forming bleb.
Our study is limited by its retrospective, non-randomized nature, as well as the use of separate surgeons for each arm of the study. Though both surgeons completed their glaucoma training at the same institution, and, except for conjunctival closure, use similar surgical technique when performing GDI surgery, there may be subtle differences in surgical technique that could affect our results. An additional limitation is the relatively short follow up time of only 6 months. The results of our study support the conclusion that the use of fibrin glue for conjunctival closure in GDI surgery is associated with faster surgical times and possibly to decreased use of IOP lowering drops in the post-operative period, while having no impact on IOP. A larger, randomized study, with increased control of surgical technique is needed to further investigate these relationships.
Glues as an aid to ophthalmic surgery have come into widespread use, with fibrin glue finding the most diverse uses. Cyanoacrylate glues are used in corneal disease due to their high tensile strength, often to plug small globe perforations or to bolster thin areas that are in danger of perforating. However their propensity for inducing inflammation, persistence as a foreign body, and impermeability to fluids and metabolites make them unsuitable for intraocular use or for use under the conjunctiva. Fibrin glue, on the other hand, does not induce an inflammatory reaction, is easily and completely broken down by the body, and is permeable to fluids and metabolites, making it suitable for sub-conjunctival use, and even intraocular use [3].
In corneal surgery the use of fibrin glue has found many uses. Its use has been described in anterior lamellar keratoplasty to glue the graft onto the host bed in what is referred to as Sutureless Anterior Lamellar Keratoplasty (SALK) [4]. Its use in pterygium surgery, to glue an amniotic membrane graft or conjunctival autograft to the scleral bed, is now common practice in many surgical centers.
In 2013 an ophthalmic technology assessment evaluated the use of fibrin glue vs sutures for closure of conjunctival incisions in strabismus surgery. While no level 1 studies were found, 5 level 2 studies were identified and analyzed, the results of which led to the conclusion that the use of fibrin glue to close limbal conjunctival incisions in strabismus surgery resulted in less postoperative inflammation and required shorter operating time compared to sutures, but it increased the percentage of wounds requiring subsequent repair with sutures [5].
In glaucoma surgery fibrin glue has been studied extensively. Choudari et al., have described its use in securing a corneal patch graft over the tube in Ahmed glaucoma valve surgery [6]. Freeman et al., compared fibrin glue to sutures in pediatric GDI surgeries for securing the tube to the sclera, the pericardial patch graft over the tube, and closing the conjunctiva and found no differences in complication rates or post-operative IOPs [7]. Martinez-de-la-Casa et al., compared the use of fibrin glue vs 10-O nylon sutures for conjunctival closure in trabeculectomy surgeries and found that each modality was equal in terms if IOP lowering and the use of fibrin glue shortened surgery times and was associated with decreased patient discomfort, though, there were a higher incidence of wound dehiscence in the fibrin glue group [8].
In 2006 Kahook and Noecker reported on the use of fibrin glue vs. sutures in GDI surgery, finding that fibrin glue was associated with less postoperative inflammation and shorter surgery times, while having no effect on postoperative IOP.
Our study supports the association with use of fibrin glue for conjunctival closure and faster surgery times. Faster surgical times are important as operating room time is expensive, thus shorter surgical times save money. A limitation of our study includes the use of two surgeons, one for each arm of the study, which could affect surgery time as one surgeon may naturally be a faster surgeon. However, the result of shorter surgery time was also found in Kahook and Noecker’s study [2] in which the same surgeon was used in both arms.
The statistically significant difference in number of IOP lowering eye drops used between the two groups was an unexpected result. Patients in the suture closure group were using more IOP lowering drops before surgery than those in the fibrin glue group and the difference in number of IOP lowering drops increased after the surgery. Both the initial difference in number of IOP lowering drops and the increase in the difference between the 2 groups were statistically significant. IOP differences between the groups were not statistically significant at PreOp or during the post-operative period, except at POW1. The difference in number of IOP lowering drops at PreOp may be a difference in practice patterns between the 2 glaucoma surgeons, with the surgeon for the suture group being more aggressive in prescribing IOP lowering drops before going to surgery. However, the statistically significant increase in the difference in number of IOP lowering drops from PreOp to PostOp suggests an increase in effectiveness of GDI surgery when fibrin glue is used vs. sutures for closure of conjunctiva.With more IOP lowering drops being used by the suture group postoperatively, if suture assisted GDI surgery and fibrin glue assisted GDI surgery are equivalent in terms of IOP lowering, one would expect the suture group to have lower IOPs than the fibrin glue group, which was not demonstrated in our results. Our results suggest that the use of fibrin glue to close conjunctiva in GDI surgery may be associated with a lower number of IOP lowering drops postoperatively. This could be explained by the decrease in inflammation associated with the use of fibrin glue, as reported by Kahook and Noecker [2], causing less fibrosis and encapsulation of the forming bleb.
Our study is limited by its retrospective, non-randomized nature, as well as the use of separate surgeons for each arm of the study. Though both surgeons completed their glaucoma training at the same institution, and, except for conjunctival closure, use similar surgical technique when performing GDI surgery, there may be subtle differences in surgical technique that could affect our results. An additional limitation is the relatively short follow up time of only 6 months. The results of our study support the conclusion that the use of fibrin glue for conjunctival closure in GDI surgery is associated with faster surgical times and possibly to decreased use of IOP lowering drops in the post-operative period, while having no impact on IOP. A larger, randomized study, with increased control of surgical technique is needed to further investigate these relationships.
ACKNOWLEDGEMENT
This academic paper is the original work of the 2 above authors and has not been previously published. It is not under consideration for publication elsewhere, and if accepted it will not be published in similar form elsewhere. No funding was provided for this research. This research was approved by our local IRB and was produced in an ethical and scientifically sound manner. Neither author nor family members of either author have any conflicts of interest relating to this research.
REFERENCES
- Arora KS, Robin AL, Corcoran KJ, Corcoran SL, Ramulu PY (2015) Use of various glaucoma surgeries and procedures in medicare beneficiaries from 1994 to 2012. Ophthalmology 122: 1615-1624.
- Kahook MY, Noecker RJ (2006) Fibrin glue-assisted glaucoma drainage device surgery. Br J Ophthalmol 90: 1486-1489.
- Panda A, Kumar S, Kumar A, Bansal R, Bhartiya S (2009) Fibrin Glue in Ophthalmology. Indian J Ophthalmol 57: 371-379.
- Agarwal T, Bandivadekar P, Sharma N, Sagar P, Titiyal J (2015) Sutureless anterior lamellar keratoplasty with phacoemulsification. Cornea 34: 615-620.
- Yang MB, Melia M, Lambert SR, Chiang MF, Simpson JL, et al. (2013) Fibrin glue for closure of conjunctival incision in strabismus surgery. Ophthalmology 120: 1935-1941.
- Choudhari NS, Neog A, Sharma A, Iyer GK, Srinivasan B (2013) Our experience of fibrin sealant-assisted implantation of Ahmed glaucoma valve. Indian J Ophthalmol 61: 23-27.
- Freeman PD, Kahook MY, Curtis TH (2010) Glaucoma drainage device implantation in children using fibrin glue. Journal of AAPOS 14: 169-171.
- Martinez-de-la-Casa JM, Rayward O, Saenz-Frances F, Mendez C, Bueso ES, et al. (2013) Use of a fibrin adhesive for conjunctival closure in trabeculectomy. Acta Ophthalmologica 91: 425-428.
Citation: Lancaster N, Kim WI (2016) Tisseel Fibrin Glue vs Sutures for Conjunctival Closure in Glaucoma Drainage Implant Surgery. J Ophthalmic Clin Res 3: 022.
Copyright: © 2016 Nicholas Lancaster, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!

