
Journal of Ophthalmology & Clinical Research Category: Clinical
Type: Research Article
UBM - A Tracker for Trabeculectomy
*Corresponding Author(s):
Shreya ThatteDepartment Of Ophthalmology, Sri Aurobindo Medical College And PG Institute, Indore, Madhya Pradesh, India
Tel:+91 9302104864,
Email:shreyathatte@gmail.com
Received Date: Apr 10, 2017
Accepted Date: May 23, 2017
Published Date: Jun 06, 2017
Abstract
Introduction
Trabeculectomy is the gold standard surgery performed for reduction of Intraocular Pressure (IOP) in controlling glaucoma. The success of surgery depends on status of bleb function post trabeculectomy. Ultrasound Biomicroscopy (UBM) is one of the important tools for bleb function monitoring.
Materials and methods
A randomized cross sectional interventional study of 50 eyes with more than 3 months follow up of primary fornix based trabeculectomy where in UBM examination was undertaken to assess bleb function.
Results
UBM analysis showed well-functioning bleb in 86.0% eyes and 14.0% as failure (4% PACG, 10% POAG). Failed cases were distinctly co-related with positive findings of 14.0% of scleral reflectivity and 12.0% route under the scleral flap. As per individual case, treatment for inner window blockers iris, vitreous, membrane and fibrosis was provided. UBM was helpful for the assessment of bleb function, cause of bleb failure and its management especially with patients who showed inconclusive gonioscopy and slit lamp procedure.
Conclusion
UBM is certainly useful for evaluating the anatomical patency of surgically created passage in post trabeculectomy patients. It provided assessments of bleb function and establishing cause in case of failure.
Trabeculectomy is the gold standard surgery performed for reduction of Intraocular Pressure (IOP) in controlling glaucoma. The success of surgery depends on status of bleb function post trabeculectomy. Ultrasound Biomicroscopy (UBM) is one of the important tools for bleb function monitoring.
Materials and methods
A randomized cross sectional interventional study of 50 eyes with more than 3 months follow up of primary fornix based trabeculectomy where in UBM examination was undertaken to assess bleb function.
Results
UBM analysis showed well-functioning bleb in 86.0% eyes and 14.0% as failure (4% PACG, 10% POAG). Failed cases were distinctly co-related with positive findings of 14.0% of scleral reflectivity and 12.0% route under the scleral flap. As per individual case, treatment for inner window blockers iris, vitreous, membrane and fibrosis was provided. UBM was helpful for the assessment of bleb function, cause of bleb failure and its management especially with patients who showed inconclusive gonioscopy and slit lamp procedure.
Conclusion
UBM is certainly useful for evaluating the anatomical patency of surgically created passage in post trabeculectomy patients. It provided assessments of bleb function and establishing cause in case of failure.
Keywords
Bleb function; Intraocular pressure; Route under the scleral flap; Scleral reflectivity; Trabeculectomy; Ultrasound biomicroscopy
INTRODUCTION
Trabeculectomy is the most popular form of glaucoma filtration surgery and remains the “gold standard” for surgical reduction of Intraocular Pressure (IOP) in uncontrolled glaucoma [1]. It has a success rate of 67% to 94% [2].This partial-thickness filtration operation reduces intra ocular pressure via the creation of a limbal fistula through which aqueous humor drains into the subconjunctival space, establishing a filtering bleb. Long-term success depends on preoperative and intraoperative conditions. Yet, it also depends highly on the persistence of filtration efficiency at the bleb site. Therefore, postoperative observation and care of developing filtering bleb in clinical practice is an important tool in reaching the target pressure after filtration surgery in higher percentage of the patients [1].
Bleb function is believed to depend on the degree of bleb fibrosis and obstruction of intrascleral aqueous humor flow [3]. Bleb appearance has been assessed using slit-lamp bio microscopy, gonioscopy, Ultrasound Bio Microscopy (UBM) and Optical Coherence Tomography (OCT). Examining bleb morphology for indications of fibrosis or blockage of fluid flow should be useful in evaluating bleb function.
Slit-lamp bio microscopy only illustrates bleb morphology and not the bleb’s internal structures. Gonioscopy helps in assessing the internal window and the peripheral iridectomy anatomical position and shape. Cross-sectional imaging modalities such as UBM and Anterior Segment Optical Coherence Tomography (AS-OCT) can depict internal structure of blebs. This therefore, provides information about the structure and possible functionality of filtering blebs [4], complimentary to that obtained by slit-lamp bio microscopy and gonioscopy.
Imaging technique AS-OCT, is useful in the evaluation of the iridocorneal angle and post trabeculectomy blebs. It is faster than UBM and eliminates the need for a water bath and eyecup in contact with the globe, therefore is a more comfortable procedure for the patient. However, it has limitations of inability to evaluate any aetiology behind the iris. Impression cytology and In vivo confocal microscopy, alone and together, are also new methods to evaluate the bleb but there are many limitations to its extent of evaluation. Incidentally, there has been limited work undertaken in it. The vascular assessment of the bleb using indocyanine green is a new method to assess the bleb, yet it is also not used because of its invasive nature and limited amount of research work in it [4,5].
Therefore, in this case series only UBM was taken into consideration to observe efficacy in monitoring bleb functions as also to record its capability in non-functioning of bleb to establish probable cause of its failure.
Charles Pavlin and Stuart Foster [5-7] developed UBM at the Princess Margaret Hospital at Toronto, Canada in 1989. UBM is a high frequency (50MHz) ultrasound technology using water bath that permits non-invasive in vivo imaging of the structural details of the anterior ocular segment at near microscopic resolution. This also helps to observe functioning of bleb [8,9].
Bleb function is believed to depend on the degree of bleb fibrosis and obstruction of intrascleral aqueous humor flow [3]. Bleb appearance has been assessed using slit-lamp bio microscopy, gonioscopy, Ultrasound Bio Microscopy (UBM) and Optical Coherence Tomography (OCT). Examining bleb morphology for indications of fibrosis or blockage of fluid flow should be useful in evaluating bleb function.
Slit-lamp bio microscopy only illustrates bleb morphology and not the bleb’s internal structures. Gonioscopy helps in assessing the internal window and the peripheral iridectomy anatomical position and shape. Cross-sectional imaging modalities such as UBM and Anterior Segment Optical Coherence Tomography (AS-OCT) can depict internal structure of blebs. This therefore, provides information about the structure and possible functionality of filtering blebs [4], complimentary to that obtained by slit-lamp bio microscopy and gonioscopy.
Imaging technique AS-OCT, is useful in the evaluation of the iridocorneal angle and post trabeculectomy blebs. It is faster than UBM and eliminates the need for a water bath and eyecup in contact with the globe, therefore is a more comfortable procedure for the patient. However, it has limitations of inability to evaluate any aetiology behind the iris. Impression cytology and In vivo confocal microscopy, alone and together, are also new methods to evaluate the bleb but there are many limitations to its extent of evaluation. Incidentally, there has been limited work undertaken in it. The vascular assessment of the bleb using indocyanine green is a new method to assess the bleb, yet it is also not used because of its invasive nature and limited amount of research work in it [4,5].
Therefore, in this case series only UBM was taken into consideration to observe efficacy in monitoring bleb functions as also to record its capability in non-functioning of bleb to establish probable cause of its failure.
Charles Pavlin and Stuart Foster [5-7] developed UBM at the Princess Margaret Hospital at Toronto, Canada in 1989. UBM is a high frequency (50MHz) ultrasound technology using water bath that permits non-invasive in vivo imaging of the structural details of the anterior ocular segment at near microscopic resolution. This also helps to observe functioning of bleb [8,9].
AIM
Evaluation and assessment of trabeculectomy bleb function using ultrasound bio microscopy, and to find out probable etiology in case of failed bleb.
MATERIALS AND METHODS
This was a randomized cross sectional interventional study of 50 eyes, with more than 3 months follow up cases of fornix-based trabeculectomy. The limbal-based trabeculectomy cases were excluded in order to maintain the homogeneity. The study was initiated after clearance from ethical committee and strictly abiding the declaration of Helsinki.
Inclusion criteria
Patients reporting to outpatient department of the institute post 3 months of fornix based trabeculectomy operation without use of any antimetabolites.
Exclusion criteria
1. Bleb infection
2. Post operated cases of trabeculectomy within 3 months post operation
3. Abnormal morphology of the anterior segment
4. Any other associated ocular disease
The 50 patients with more than 3 months post trabeculectomy, who randomly presented themselves in outpatient department for follow up, were assessed after a signed/informed consent form from the patients for study related examination irrespective of the cause and type of glaucoma. This study constituted patients with
1. Primary Open-Angle Glaucoma (POAG)
2. Pseudo exfoliative glaucoma
3. Primary Angle-Closure Glaucoma (PACG) (post failure of treatment by iridotomy or iridectomy)
4. Neovascular glaucoma
5. Angle recession glaucoma
Patient data recorded for the study included Name, Gender, Age, Date of trabeculectomy, Details of Postoperative secondary interventions. In addition, use of systemic and topical medications including the anti-glaucoma drugs was noted. Ophthalmic examinations in more than 3 months of trabeculectomy consisted of IOP, best corrected visual acuity, slit lamp bio-microscopy, gonioscopy and ultrasound bio-microscopy along with perimetry and fundus photograph to observe post-surgical status in relation to glaucoma, as done routinely.
2. Post operated cases of trabeculectomy within 3 months post operation
3. Abnormal morphology of the anterior segment
4. Any other associated ocular disease
The 50 patients with more than 3 months post trabeculectomy, who randomly presented themselves in outpatient department for follow up, were assessed after a signed/informed consent form from the patients for study related examination irrespective of the cause and type of glaucoma. This study constituted patients with
1. Primary Open-Angle Glaucoma (POAG)
2. Pseudo exfoliative glaucoma
3. Primary Angle-Closure Glaucoma (PACG) (post failure of treatment by iridotomy or iridectomy)
4. Neovascular glaucoma
5. Angle recession glaucoma
Patient data recorded for the study included Name, Gender, Age, Date of trabeculectomy, Details of Postoperative secondary interventions. In addition, use of systemic and topical medications including the anti-glaucoma drugs was noted. Ophthalmic examinations in more than 3 months of trabeculectomy consisted of IOP, best corrected visual acuity, slit lamp bio-microscopy, gonioscopy and ultrasound bio-microscopy along with perimetry and fundus photograph to observe post-surgical status in relation to glaucoma, as done routinely.
Statistical Analysis
Correlation was calculated between two numeric variables. Significance of association and difference between categorical variables has been assessed by calculating chi square test. Calculations were done for all values for 95% confidence level. SPSS version 21 was used for the calculation of all statistical tests.
IOP evaluation
IOP was measured with Goldman applanation tonometry during the afternoon hours. While evaluating post trabeculectomy patients on UBM, three groups were formed according to IOP values as set by Avitabile et al., [10]. The groups were as under (Table 1).
| Group | 1 | 2 | 3 |
| IOP | < 10 mm of Hg | 10-18 mm of Hg | >18 mm of Hg |
UBM evaluation
1. The patients were examined on 35MHz (Optos OTI Scan 3000) ultrasound bio-microscopy after anaesthetized with topical anesthetic agent and the eye cup was fitted and filled with saline.
2. The crystal of the transducer was placed in saline approximately 2 mm from the eye surface.
3. The eye was scanned in each clock hour from the center of the cornea to the ora serrata.
4. The bleb area was examined and the probe’s direction was changed accordingly to examine the bleb.
5. Special consideration was given to the scleral reflectivity and the route under the scleral flap and findings of same were noted and graded.
UBM evaluation was classified into three groups according to Avitabile et al., given in 1998 [10]. This classification was latest amongst all and simplest to use and utilizes both the criteria (scleral reflectivity and route under the scleral flap), which was also recommended by previous studies by Yamamoto (1995) and Mc Whae (1996).
2. The crystal of the transducer was placed in saline approximately 2 mm from the eye surface.
3. The eye was scanned in each clock hour from the center of the cornea to the ora serrata.
4. The bleb area was examined and the probe’s direction was changed accordingly to examine the bleb.
5. Special consideration was given to the scleral reflectivity and the route under the scleral flap and findings of same were noted and graded.
UBM evaluation was classified into three groups according to Avitabile et al., given in 1998 [10]. This classification was latest amongst all and simplest to use and utilizes both the criteria (scleral reflectivity and route under the scleral flap), which was also recommended by previous studies by Yamamoto (1995) and Mc Whae (1996).
OBSERVATION AND RESULTS
This observation with various etiological types of glaucoma to post trabeculectomy IOP was noted to know relation of bleb function in terms of IOP, which shows no significance with type of glaucoma.
In the good blebs (48%) IOP was in normal range, while in the poor bleb (10%) IOP was more than 18 mm of Hg. The fair category (42%) had IOP in both the controlled and the uncontrolled level. This shows that the type of blebs is directly significant for the maintenance of normal IOP post trabeculectomy.
From the chi square test result, that came out to be highly significant (0.000), which approves that the IOP is positively correlated to the UBM findings. Better the score of the bleb; the better the IOP levels are attained.
The route under the scleral flap was not visible in 11 (22%) patients. Out of these 11 patients 6 had IOP more than 18 mmHg. While in 39 (78%) patients the route was visible and only 1 patient had IOP more than 18 mmHg rest all patients had normal IOP. This one patient had an encapsulated bleb which was responsible for the increase in IOP despite functioning inner ostium and the visibility of the route under the scleral flap.
This clearly shows that the visualization of the route under the scleral flap in the post trabeculectomy patients on UBM is positively correlated to IOP which is also highly significant (p=0.00). The visualization of the route is a good sign for the evaluation of the surgery.
There is high positive significant correlation of type of reflectivity of the scleral flap judged on UBM to the IOP. The more is the reflectivity, the higher range of the IOP levels is present.
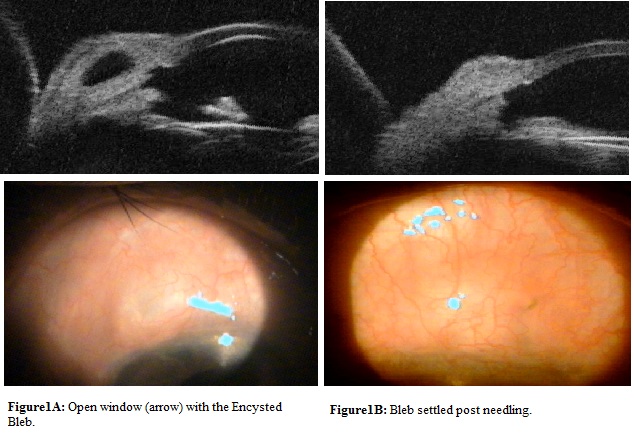
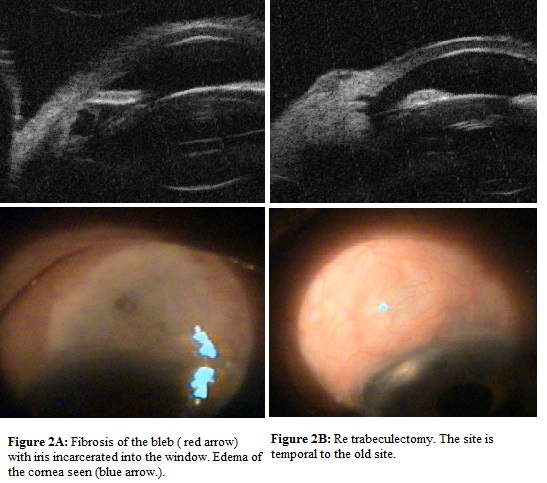
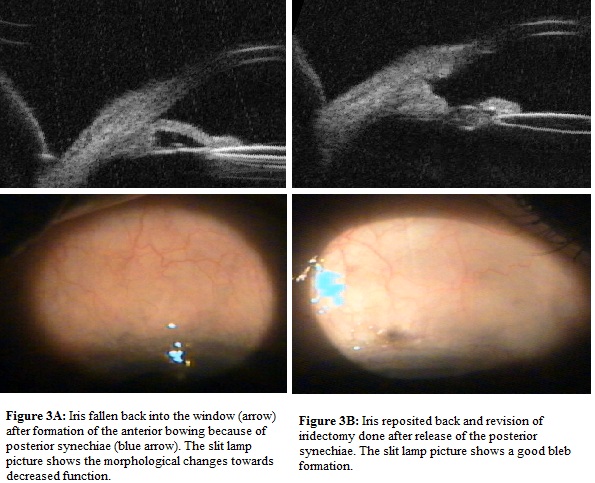
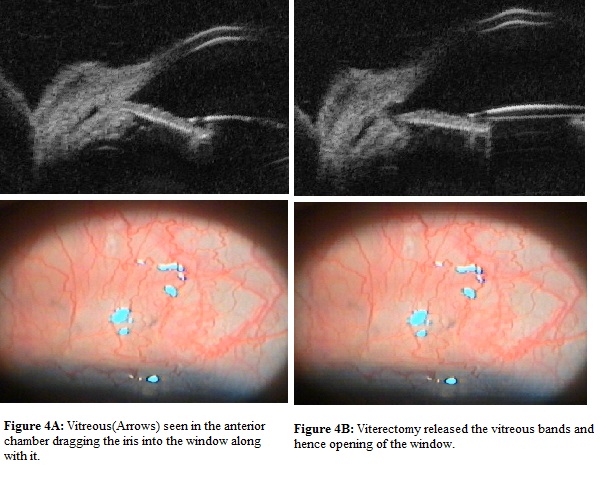
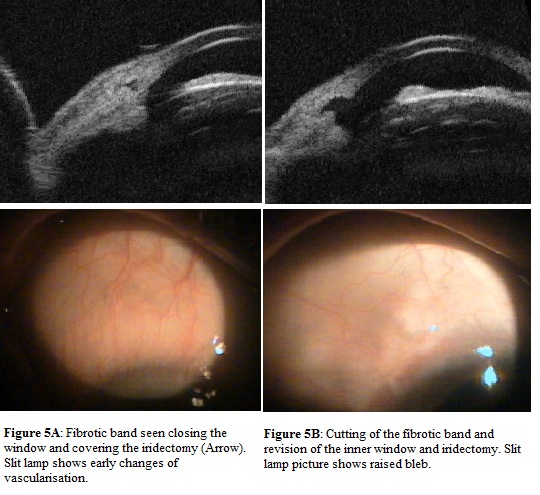
This table observed that morphologically poor bleb had reason to fail to function and reasons were identified and managed. One patient had encysted bleb, which was treated with needling to achieve functioning bleb (Figure 1 (A,B)). In two cases bleb was fibrosed and route under the flap was absent for which re-trabeculectomy was performed (Figure 2 (A,B)). Iris was blocking inner window in one case, problem was solved by repositioning of iris back along with revision of iridectomy (Figure 3 (A,B)). In one patient inner window was blocked by vitreous, which was released by vitrectomy and window was opened (Figure 4 (A,B)). Fibrous band closing window and covering iridectomy was seen in one patient, fibrous band was cut and inner window was reformed (Figure 5 (A<B)).
In the good blebs (48%) IOP was in normal range, while in the poor bleb (10%) IOP was more than 18 mm of Hg. The fair category (42%) had IOP in both the controlled and the uncontrolled level. This shows that the type of blebs is directly significant for the maintenance of normal IOP post trabeculectomy.
From the chi square test result, that came out to be highly significant (0.000), which approves that the IOP is positively correlated to the UBM findings. Better the score of the bleb; the better the IOP levels are attained.
The route under the scleral flap was not visible in 11 (22%) patients. Out of these 11 patients 6 had IOP more than 18 mmHg. While in 39 (78%) patients the route was visible and only 1 patient had IOP more than 18 mmHg rest all patients had normal IOP. This one patient had an encapsulated bleb which was responsible for the increase in IOP despite functioning inner ostium and the visibility of the route under the scleral flap.
This clearly shows that the visualization of the route under the scleral flap in the post trabeculectomy patients on UBM is positively correlated to IOP which is also highly significant (p=0.00). The visualization of the route is a good sign for the evaluation of the surgery.
There is high positive significant correlation of type of reflectivity of the scleral flap judged on UBM to the IOP. The more is the reflectivity, the higher range of the IOP levels is present.
This table observed that morphologically poor bleb had reason to fail to function and reasons were identified and managed. One patient had encysted bleb, which was treated with needling to achieve functioning bleb (Figure 1 (A,B)). In two cases bleb was fibrosed and route under the flap was absent for which re-trabeculectomy was performed (Figure 2 (A,B)). Iris was blocking inner window in one case, problem was solved by repositioning of iris back along with revision of iridectomy (Figure 3 (A,B)). In one patient inner window was blocked by vitreous, which was released by vitrectomy and window was opened (Figure 4 (A,B)). Fibrous band closing window and covering iridectomy was seen in one patient, fibrous band was cut and inner window was reformed (Figure 5 (A<B)).
DISCUSSION
We had 50 patients out of which 29 were females and 21 were males. The mean age of presentation was 62.16 years. There were more number of females (n= 29, 58%) as compared to the males (n=21, 42%) in our study. We divided the patients into 3 groups (Table 1) with IOP > 18 mmHg, 10 to 18 mmHg and equal to or < 10mmHg. The group with IOP more than 18 mmHg was considered failure while rest were considered successful [10,11]. This reference range was taken into account according to the study of Avitable et al., who used this division of the IOP range while studying the IOP correlation with the UBM findings. In our study also, we compared the IOP levels in the post trabeculectomy patients with UBM findings.
On statistical analysis, the correlation of IOP to the type of glaucoma was not significant (Table 2). These findings are consistent with the findings of Sihota et al., [12] where they studied long-term follow up of 64 patients after trabeculectomy in both POAG and PACG and concluded that trabeculectomy is equally effective in both for controlling the IOP. It interprets that the type of glaucoma was not a confounding factor in our study while deriving the conclusion.
On statistical analysis, the correlation of IOP to the type of glaucoma was not significant (Table 2). These findings are consistent with the findings of Sihota et al., [12] where they studied long-term follow up of 64 patients after trabeculectomy in both POAG and PACG and concluded that trabeculectomy is equally effective in both for controlling the IOP. It interprets that the type of glaucoma was not a confounding factor in our study while deriving the conclusion.
| Value | Sig. | |
| Pearson Chi-Square | 1.247 | 0.996 |
| Value | Sig. | |
| Pearson Chi-Square | 39.456 | 0.000 |
| Value | Sig. | |
| Pearson Chi-Square | 20.141 | 0.000 |
| Chi-Square Tests | |||
| Value | df | Asymp. Sig. (2-sided) | |
| Pearson Chi-Square | 40.505a | 4 | 0.000 |
| Cross table | ||||||
| IOP range | Total | |||||
| 1 | 2 | 3 | ||||
| Type Of Glaucoma | PACG | Count | 1 | 13 | 2 | 16 |
| % of Total | 2.00% | 26.00% | 4.00% | 32.00% | ||
| POAG | Count | 2 | 23 | 5 | 30 | |
| % of Total | 4.00% | 46.00% | 10.00% | 60.00% | ||
| Neovascular | Count | 0 | 2 | 0 | 2 | |
| % of Total | 0.00% | 4.00% | 0.00% | 4.00% | ||
| Exfoliative | Count | 0 | 1 | 0 | 1 | |
| % of Total | 0.00% | 2.00% | 0.00% | 2.00% | ||
| Angle recession | Count | 0 | 1 | 0 | 1 | |
| % of Total | 0.00% | 2.00% | 0.00% | 2.00% | ||
| Total | Count | 3 | 40 | 7 | 50 | |
| % of Total | 6.00% | 80.00% | 14.00% | 100% | ||
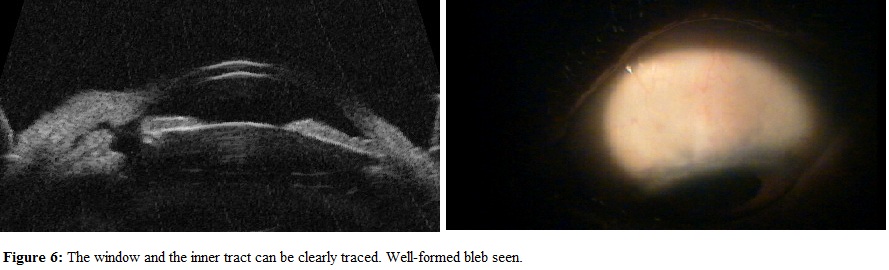
In the examination of the UBM grading (Table 3 and 4), all the patients with good blebs (48%) (Figure 6) had IOP in normal range, while all patients with poor bleb (10%) had IOP more than 18 mmHg. The fair category (42%) had IOP in both the controlled and the uncontrolled level. This signifies that the low reflectivity and the presence of the route under the scleral flap are significant for the maintenance of normal IOP post trabeculectomy. The correlation of UBM grading with IOP levels was found to be highly significant (p<0.01). Similar findings were seen by Avitabile et al., [10] who also did same kind of study graded the bleb into good, fair, poor on the basis of type scleral reflectivity and the visibility of route under the scleral flap and concluded that the UBM grade function of the bleb was significantly associated with IOP control (p<0.01). Similarly, Yamamoto et al., [13] considered these two criteria important for the prediction of the bleb.
| Type of bleb | Scleral reflectivity | Route under scleral flap |
| Good | Low | Seen (present) |
| Poor | High | Not seen |
| Fair | Any of the bleb which don’t fall in any of the above category | |
Table 3: Comparison of Ultra Biomicroscopy (UBM) to IOP Range.
| Cross-table | ||||||
| IOP range | Total | |||||
| 1 | 2 | 3 | ||||
| UBM | Fair | Count | 3 | 16 | 2 | 21 |
| % of Total | 6.0% | 32.0% | 4.0% | 42.0% | ||
| Good | Count | 0 | 24 | 0 | 24 | |
| % of Total | 0.0% | 48.0% | 0.0% | 48.0% | ||
| Poor | Count | 0 | 0 | 5 | 5 | |
| % of Total | 0.0% | 0.0% | 10.0% | 10.0% | ||
| Total | Count | 3 | 40 | 7 | 50 | |
| % of Total | 6.0% | 80.0% | 14.0% | 100% | ||
Considering the individual findings on UBM, the route under the scleral flap (Table 5) was not visible in 11(22%) of the patients. Out of these 11 patients, 6 had IOP more than 18 mmHg. While in 39 (78%) of the patients the route was visible and only 1 patient had IOP more than 18 mmHg rest all patients had IOP less than 18. The visualization of the route under the scleral flap in the post trabeculectomy patients on UBM is significantly correlated [p < 0.01] to the IOP. These findings are consistent with the findings of Yamamoto et al., [13] and Avitabile et al., [11] who quoted that presence of route under scleral flap is correlated with the IOP of glaucomatous eyes that underwent trabeculectomy in their study.
| Cross table | ||||||
| IOP Range | Total | |||||
| 1 | 2 | 3 | ||||
| Route Under The Scleral Flap | 0 | Count | 1 | 4 | 6 | 11 |
| % of Total | 2.0% | 8.0% | 12.0% | 22.0% | ||
| 1 | Count | 2 | 36 | 1 | 39 | |
| % of Total | 4.0% | 72.0% | 2.0% | 78.0% | ||
| Total | Count | 3 | 40 | 7 | 50 | |
| % of Total | 6.0% | 80.0% | 14.0% | 100% | ||
The high scleral reflectivity (Table 6) was present in 7 patients, out of these 6 patients had IOP more than 18mmHg signifying that high scleral reflectivity point to impending failure. All the patients with low reflectivity had patients with IOP less than 18 mmHg. Hence, the low reflectivity foretells the good prognosis of the bleb. These findings were also highly significant (p<0.01) showing that the scleral reflectivity is correlated to the IOP. Our findings are consistent with the findings of Yamamoto et al., [13] and Avitabile et al., [11], who also concluded the high correlation of scleral reflectivity to IOP. They also found that the failing or failed bleb do show high reflectivity on UBM.
| Cross table | ||||||
| IOP Range | Total | |||||
| 1 | 2 | 3 | ||||
| Route Under The Scleral Flap | 0 | Count | 1 | 4 | 6 | 11 |
| % of Total | 2.0% | 8.0% | 12.0% | 22.0% | ||
| 1 | Count | 2 | 36 | 1 | 39 | |
| % of Total | 4.0% | 72.0% | 2.0% | 78.0% | ||
| Total | Count | 3 | 40 | 7 | 50 | |
| % of Total | 6.0% | 80.0% | 14.0% | 100% | ||
In this study, etiology for bleb failure could be established during the evaluation, which was not identified in previous studies. (Table 7) Established etiology for bleb failure was managed by removing the cause responsible for blockage of aqueous flow. This was very useful in treating failed bleb and achieving goal of functioning bleb and maintaining IOP. This was superfluous value in this study.In this study, etiology for bleb failure could be established during the evaluation, which was not identified in previous studies. (Table 7) Established etiology for bleb failure was managed by removing the cause responsible for blockage of aqueous flow. This was very useful in treating failed bleb and achieving goal of functioning bleb and maintaining IOP. This was superfluous value in this study.
| Serial no. | IOP | UBM | Duration of surgery | Cause of failure | Post failure surgical management | |
| 1 | 23 | FAIR | 3 Months | Iris in window | Repositioning of iris | |
| 2 | 40 | POOR | 12 Months | Membrane at window | Removal of membrane | |
| 3 | 25 | POOR | 14 Months | Absent route | Revision of bleb | |
| 4 | 27 | POOR | 12 Months | Open window | Needling | |
| (Encysted) | ||||||
| 5 | 42 | POOR | 24 Months | Absent route Fibrosis | Re- trabeculectomy | |
| 6 | 22 | FAIR | 8 Months | Vitreous tag in window | Cutting vitreous | |
| 7 | 23 | POOR | 30 Months | Absent route Fibrosis | Re trabeculectomy |
CONCLUSION
UBM is helpful in appreciating the morphology and predicting patency of the aqueous drainage pathway created post-trabeculectomy. Both the scleral reflectivity and the route under the scleral flap are significant in predicting the outcome of the bleb. It is also supportive in identifying etiology of bleb failure, those in front and behind the iris, which is useful in decision-making intervention to manage bleb failure. In patients where the AS OCT, gonioscopy and slit lamp is not conclusive for the cause of failure and assessment, UBM is helpful for the assessment of trabeculectomy.
REFERENCES
- Furrer S, Menke MN, Funk J, Töteberg-Harms M (2012) Evaluation of filtering blebs using the ‘Wuerzburg bleb classification score’ compared to clinical findings. BMC Ophthalmol 12: 24.
- Skuta GL, Parrish RK 2nd (1987) Wound healing in glaucoma filtering surgery. Surv of Opthalmol 32:149–170.
- Nakano N, Hangai M, Nakanishi H, Inoue R, Unoki N et al., (2010) Early trabeculectomy bleb walls on anterior-segment optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 248: 1173-1182.
- Maslin JS, Barkana Y, Dorairaj SK (2015) Anterior segment imaging in glaucoma: An updated review. Indian J Ophthalmol 63: 630-640.
- Pavlin CJ, Harasiewicz K, Foster FS (1992) Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol 113: 381-389.
- Pavlin CJ, Sherar MD, Foster FS (1990) Subsurface ultrasound microscopic imaging of the intact eye. Ophthalmology 97: 244-250.
- Pavlin CJ, Harasiewicz K, Sherar MD, Foster FS (1991) Clinical use of ultrasound biomicroscopy. Ophthalmology 98: 287-295.
- Kapetansky FM (1997) A new water bath for ultrasonic biomicroscopy. Ophthalmic Surg Lasers 28: 605-606.
- Esaki K, Ishikawa H, Liebmann JM, Ritch R (200) A technique for performing ultrasound biomicroscopy in the sitting and prone positions. Ophthalmic Surg Lasers 31: 166-169.
- Avitabile T, Russo V, Uva MG, Marino A, Castiglione F et al., (1998) Ultrasound biomicroscopic evaluation of filtering blebs after laser suture lysis trabeculectomy. Ophthalmologica 21: 17-21.
- Osman. Can Ultrasound Biomicroscopy (UBM) Predict Bleb Function? A Comparative Study between Ultrasound Biomicroscopy (UBM) Guided Bleb Morphological Assessment and the Actual Intraocular Pressure (IOP) Outcome. Kasr El Aini Medical Journal. July 2012; 18(3):75-83.
- Sihota R, Gupta V, Agarwal HC (2004) Long-term evaluation of trabeculectomy in primary open angle glaucoma and chronic primary angle closure glaucoma in an Asian population. Clin Exp Ophthalmol 32: 23-28.
- Yamamoto T, Sakuma T, Kitazawa Y (1995) An ultrasound biomicroscopic study of filtering blebs after mitomycin C trabeculectomy. Ophthalmology 102: 1770-1776.
Citation: Thatte S, Rana R (2017) UBM - A Tracker for Trabeculectomy. J Ophthalmic Clin Res 4: 029.
Copyright: © 2017 Shreya Thatte, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!

