
Understanding of the Aetiology and Management of Secondary Macular Hole Using Optical Coherence Tomography Angiography
*Corresponding Author(s):
Abhishek SharmaRetinal Surgeon, Department Of Ophthalmology, Royal Brisbane & Women’s Hospital, Queensland Eye Institute 140 Melbourne Street, South Brisbane, QLD 4101, Australia
Tel:+61 0732395000,
Fax:+61 0738445000
Email:Abhishek.Sharma@qei.org.au
Abstract
Purpose: The purpose of this case report is to describe application of Optical Coherence Tomography Angiography (OCT-A) imaging technique in diagnosing and managing a case of secondary macular hole.
Methods: A case report was conducted.
Results: A 34-year old female presented with painless loss of vision in the right eye. Fundus examination and OCT showed atypical macular hole with atrophic changes, and optical coherence tomography angiography showed hypoperfusion within the deep retinal layers. Clinical findings suggest that patient had chorioretinitis at the macula, presumed ocular toxoplasmosis. Retinal inflammation reduced and vision slightly improved in the affected eye, as result of treatment with antibiotic.
Conclusion: Secondary macular hole formation is an atypical consequence of toxoplasmosis that can be associated with significant central vision loss. Optical coherence tomography angiography for this case demonstrates the loss of vascular architecture, indicating a guarded poor visual prognosis.
Keywords
Chorioretinitis; Optical coherence tomography angiography; Macular hole
INTRODUCTION
Macular Hole (MH) is a clinical entity that mainly occurs idiopathically [1-3], however MH can also be associated with trauma [4], inflammation and myopia [5,6]. Morphological changes in MH have been extensively studied using Optical Coherence Tomography (OCT) [7-9]. Along with the structural changes, it is also important to assess retinal vessels calibre that is known to be involved in the development and healing of retinal diseases.
Optical Coherence Tomography Angiography (OCT-A) is an innovative revolutionary technology that uses motion contrast to visualize the microvasculature features of various retinal diseases. Recently, a few studies employed OCT-A to document changes in foveal microvasculature in the MH eyes [10-12]. In this report, we investigated the characteristics of the foveal structure and retinal vasculature for a patient using OCT-A, before and after macular hole closure.The formation of the macular hole took place due to an acute retinochoroiditis that was thought to be associated with macular toxoplasmosis.
CASE REPORT
A 34-year-old female presented in our clinic with a 10-day history of painless loss of vision in the right eye. The Best-Corrected Visual Acuity (BCVA) was count finger vision in the right eye and 20/20 in the left eye. The patient did not give any history of ocular trauma, redness or pain or any history of previous uveitis in that eye. She was originally from Latin America and reported that she had multiplecats in her home country. She was diagnosed with Guillain-Barré Syndrome four years prior to this visit; otherwise, she had no other significant medical, surgical or ocular histories. The anterior segment examination was unremarkable, with no signs of inflammation. The fundus examination in the right eye had a central appearance of MH, with an underlying yellow lesion that appeared active, with overlying vitreous debris at the macula and optic disc with mild disc hyperaemia (Optos® California, Figure 1A). There were no signs of peripheral retinitis, vasculitis, or previous fundus lesions. The left fundus was normal. Optical Coherence Tomography (OCT) B-scan (acquired by Carl Zeiss Meditech Cirrus HD-OCT 5000) (Figure 1B) of the right eye showed atypical MH with necrotic material at the centre of the hole. There was a loss of retinal layer architecture in the adjacent retina. Fundus auto-fluorescence images, acquired by Spectralis, Heidelberg Engineering, showed hyperautofluorescent ring around the central macula (Figure 1C).
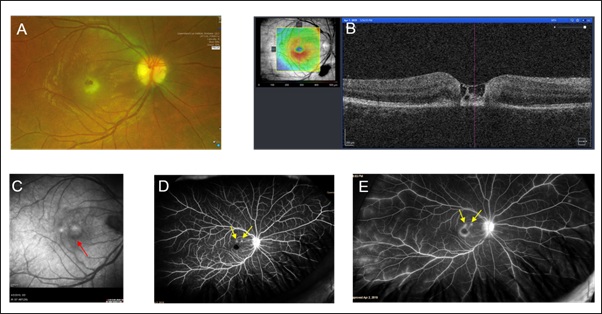 Figure 1: Optos fundus photograph of the right retina (A) and OCT B-scan (B) showing atypical macular hole with separation between inner and outer retina with irregular foveal contour. Fundus auto-fluorescence image of right eye shows hyper-auto ring around the central macula (C) [marked with a red arrow]. Early phase (D) and late phase (E) fluorescein angiography shows two hyper reflective dots near fovea between 12-2 O’clock position (marked with yellow arrows), increased foveal avascular zone, hyper reflective disc (late phase) and peripheral leaky vessels (late phase), with no evidence of choroidal neovascularization.
Figure 1: Optos fundus photograph of the right retina (A) and OCT B-scan (B) showing atypical macular hole with separation between inner and outer retina with irregular foveal contour. Fundus auto-fluorescence image of right eye shows hyper-auto ring around the central macula (C) [marked with a red arrow]. Early phase (D) and late phase (E) fluorescein angiography shows two hyper reflective dots near fovea between 12-2 O’clock position (marked with yellow arrows), increased foveal avascular zone, hyper reflective disc (late phase) and peripheral leaky vessels (late phase), with no evidence of choroidal neovascularization.
Clinical findings suggested that the patient had chorioretinitis at the macula with some active inflammation, so fundus fluorescein angiography (FFA, acquired by Optos® California) was performed. FFA demonstrated an enlarged right foveal avascular zone with no perfusion, and two areas of pinpoint hyperfluorescence superior to the fovea in the early phase, that had a mild increase in leakage in the late phase. There was mild peripheral diffuse vascular leakage in the late phase in the right temporal periphery (1D and 1E). OCT-A demonstrated loss of flow at all three layers of parafoveal superficial and deep plexus, as well as choriocapillaris (Figure 2). OCT of the optic disc confirmed disc hyperemia with a thickened retinal nerve fibre layer (Figure 3).
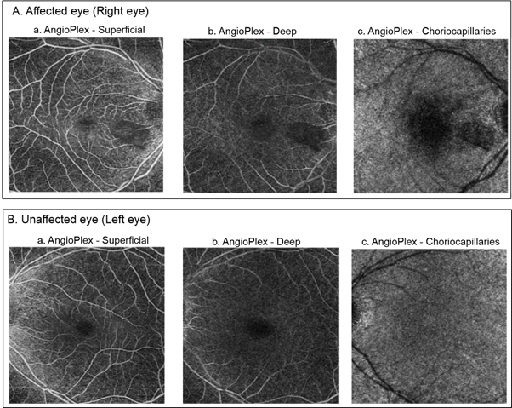 Figure 2: Top (A) and bottom (B) panels illustrate enface images of optical coherence tomography angiography of the superficial (a) and deep (b) retina and choriocapillaries (c) for affected eye (right eye) and unaffected eye (left eye), respectively.
Figure 2: Top (A) and bottom (B) panels illustrate enface images of optical coherence tomography angiography of the superficial (a) and deep (b) retina and choriocapillaries (c) for affected eye (right eye) and unaffected eye (left eye), respectively.
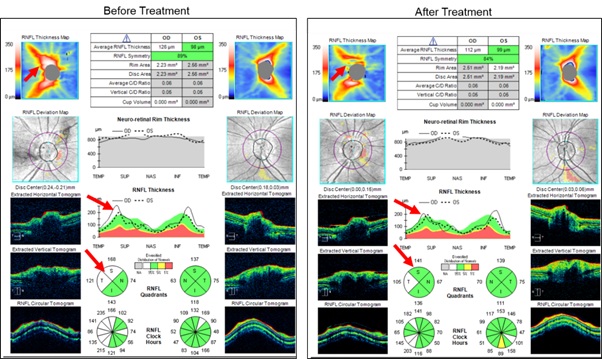 Figure 3: Optical coherence tomography images for optic discs (left panel) show mild disc oedema in the right eye (average Retinal Nerve Fiber Layer (RNFL) thickness 126 microns and 98 microns in the Right Eye (RE) and Left Eye (LE), respectively, prior to treatment commenced. After treatment received for four weeks, average RNFL thickness for the RE reduced to 112 microns (right panel).
Figure 3: Optical coherence tomography images for optic discs (left panel) show mild disc oedema in the right eye (average Retinal Nerve Fiber Layer (RNFL) thickness 126 microns and 98 microns in the Right Eye (RE) and Left Eye (LE), respectively, prior to treatment commenced. After treatment received for four weeks, average RNFL thickness for the RE reduced to 112 microns (right panel).
A full uveitic history otherwise was negative, and an infective and autoimmune blood screen was performed. Toxoplasma gondii serologic testing was positive for IgG and negative for IgM. Treatment was commenced with Trimethoprim and Sulfamethoxazole for presumed ocular toxoplasmosis. Examination at one-week post-treatment revealed an improvement in the size of the right central yellow lesion and at fourweeks mild visual restoration in the right eye (BCVA 20/100, with eccentric fixation). The option for further treatment with oral steroids discussed but the patient denied this treatment option. Due to the guarded central vision prognosis with atrophic and avascular foveal changes, macular hole surgery was discussed but ultimately decided against it.
In figure 4, the top panel shows OCT B-scans for the right retina that indicates reduced macular inflammation, that took place after treating the patient with the antibiotic. After 4 weeks of treatment, a remarkable reduction of hypoperfusion observed in enface OCT angiography, within the ellipsoid zone, between inner and outer segments (IS/OS junction) of the photoreceptors (marked with red arrows in Figure 4 - bottom panel). In addition to changes in the macula, optic disc hyperemia partly resolved, as shown in figure 3.
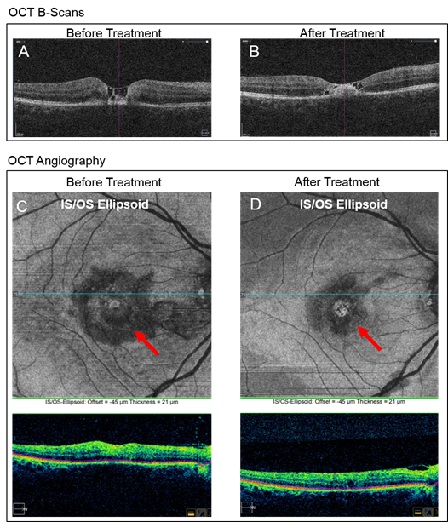 Figure 4: Optical coherence tomography B-scans of right retina, before (A) and after (B) treatment. Enface images of optical coherence tomography angiography of the ellipsoid zone [i.e., between inner and outer segments (IS/OS junction) of the photoreceptors] before (C) and after (D) treatment.
Figure 4: Optical coherence tomography B-scans of right retina, before (A) and after (B) treatment. Enface images of optical coherence tomography angiography of the ellipsoid zone [i.e., between inner and outer segments (IS/OS junction) of the photoreceptors] before (C) and after (D) treatment.
DISCUSSION
In this report, we investigated the OCT-A measured features of the retinal microvasculature in the eye with the therapeutically closed secondary MH that was associated with chorioretinitis. The clinical features of chorioretinal lesion and the patient’s past medical history suggest that our patient had unilateral acute maculopathy associated with toxoplasmosis. A previous case study reported an association between Guillain-Barré Syndrome and acute toxoplasmosis in a 21 years old man, due to a new and unknown zemodeme [13]. While negative serology of IgM typically suggests no acute infection occurred within the last six months, correct immunoglobulins responses may not be seen in patients with reactivation of the disease [14].
Despite a large number of cases presented with ocular toxoplasmosis related to various retinal complications [15-18], there have been few studies that reported on macular holes [19,20]. This is the first report of a toxoplasmosis related secondary macular hole with OCT-Angiography (OCT-A) imaging demonstrating loss of flow in the parafoveal region that partly is restored following treatment. Previous reports suggested that MH formation in ocular toxoplasmosis can be caused by vitreoretinal tractions [19,20]. In our report, OCT-A images demonstrated subfoveal ischemic retinochoroidal vasculitis, thus may suggest that posterior uveitis or choroiditis (e.g., sarcoid lesions at the fovea) can be an another possible pathophysiological mechanism for macular hole formation in ocular toxoplasmosis.
Spectral-Domain Optical Coherence Tomography (SD-OCT) is an important diagnostic tool that can be used to identify morphological features of the chorioretinal changes associated with ocular toxoplasmosis [21-22]. In addition to SD-OCT, we used OCT-angiography that was a relatively new technology for high resolution visualization of the individual vascular layers of the retina. In figure 4, the acute phase of ocular toxoplasmosis was presented with hyporeflectivity of the neurosensory retina with photoreceptor interruption that referred to an active inflammation within the deep retinal layers. During follow-up, with the treatment of disease, the inflamed area became smaller thus led to an improvement in vision by 10-15%. These features were identified by enface OCT-angiography images than SD-OCT images.
In conclusion, formation of macular hole is an atypical consequence of toxoplasmosis. Early diagnosis and treatment may prevent vision loss in patients. OCT angiography is safe and non-invasive that can be used to study retinochoroidal vascular features, thus may provide valuable information in examining retinal pathophysiology and therapeutic response, and guide discussion for surgery.
ETHICAL APPROVAL
Written informed consent was obtained from patient to use non-identifiable medical data for research purpose. This report respects the confidentiality and anonymity of the patient.
DECLARATION OF CONFLICTING INTERESTS
The authors(s) declared no potential conflicts of interest with respect to research, authorship, and/or publication of this article.
FUNDING
The author(s) received no financial support for the research, authorship, and/or publication of this article.
REFERENCES
- Margheria RR, Schepens CL (1972) Macular breaks. 1. Diagnosis, etiology, and observations. Am J Ophthalmol 74: 219-232.
- McDonnell PJ, Fine SL, Hillis AI (1982) Clinical features of idiopathic macular cysts and holes. Am J Ophthalmol 93: 777-786.
- Morgan CM, Schatz H (1985) Idiopathic macular holes. Am J Ophthalmol 99: 437-444.
- Knapp H (1869) Überisoliertezerreissungen der aderhaut in folge von traumen auf demaugapfel. Arch Augenheilkd 1: 6-12.
- Collins ET (1900) Unusual changes to the macular region. Trans Ophthalmol Soc UK 20: 196-197.
- Noyes HD (1871) Detachment of Retina with Laceration at Macula. Trans Am Ophthalmol Soc 1: 128-129.
- Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, et al. (2013)The International Vitreomacular Traction Study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120: 2611-2619.
- Kusuhara S, Escaño MFT, Fujii S, Nakanishi Y, Tamura, Y, et al. (2004) Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol 138: 709-716.
- Yun C, Oh J, Hwang SY, Togloom A, Kim SW, et al. (2012) Morphologic characteristics of chronic macular hole on optical coherence tomography. Retina 32: 2077-2084.
- Rizzo S, Savastano A, Bacherini D, Savastano MC (2017) Vascular features of full-thickness macular hole by OCT angiography. Ophthalmic Surg Lasers Imaging Retina 48: 62-68.
- Teng Y, Yu M, Wang Y, Liu X, You Q, et al. (2017) OCT angiography quantifying choriocapillary circulation in idiopathic macular hole before and after surgery. Graefes Arch Clin Exp Ophthalmol 255: 893-902.
- Baba T, Kakisu M, Nizawa T, Oshitari T, Yamamoto S (2017) Superficial foveal avascular zone determined by optical coherence tomography angiography before and after macular hole surgery. Retina 37: 444-450.
- Bossi P, Caumes E, Paris L, Dardé ML, Bricaire F (1998) Toxoplasma gondii-associated Guillain-Barré syndrome in an immunocompetent patient . J Clin Microbiol 36: 3724-3725.
- Ozgonul C, Besirli CG (2017) Recent Developments in the Diagnosis and Treatment of Ocular Toxoplasmosis. Ophthalmic Res 57: 1-12.
- Smith JR, Cunningham ET Jr (2002) Atypical presentations of ocular toxoplasmosis. Curr Opin Ophthalmol 13: 387-392.
- Pereira A, Orefice F (2001) Toxoplasmosis. In: Foster CS, Vitale AT, , Diagnosis and treatment of uveitis (1st Edn, Pg no’s: 385-410), W.B. Saunders Company, Philadelphia, USA.
- Holland GN (2003) Ocular toxoplasmosis: a Global Reassessment. Part I: epidemiology and course of disease. Am J Ophthalmol 136: 973-988.
- Schlaegel TF Jr, Weber JC (1984) The macula in ocular toxoplasmosis. Arch Ophthalmol 102: 697-698.
- Blaise P, Comhaire Y, Rakic JM (2005) Giant Macular hole as an atypical consequence of a toxoplasmic chorioretinitis. Arch Ophthalmol 123: 863-864.
- Panos GD, Papageorgiou E, Kozeis N, Gatzioufas Z (2013) Macular hole formation after toxoplasmic retinochoroiditis. BMJ Case Rep 2013: 008915.
- Alwassia AA, Cho H, Adhi M, Duker JS, Baumal CR (2013) Sequential optical coherence tomography images of retinal necrosis in acute ocular toxoplasmosis. Retina Cases Brief Rep 7: 98-101.
- Goldenberg D, Goldstein M, Loewenstein A, Habot-Wilner Z (2013) Vitreal, retinal, and choroidal findings in active and scarred toxoplasmosis lesions: a prospective study by spectral-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 251: 2037-2045.
Citation: Ghosh A, Sharma A (2020) Understanding of the Aetiology and Management of Secondary Macular Hole Using Optical Coherence Tomography Angiography. J Ophthalmic Clin Res 7: 069.
Copyright: © 2020 Atanu Ghosh, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

